Healing our healthcare system starts with valuing our healthcare heroes
The C-suite leaders of U.S. hospitals and health systems have a critical charge as the stewards of our nation’s healthcare system: Cultivate an environment of well-deserved trust that encompasses patients and caregivers alike. Without such trust, our healthcare system will flounder.
Building trust starts with demonstrating integrity in upholding the organization’s mission of delivering high-quality, compassionate care to all patients. And it also starts with respecting and supporting those highly trained professionals whose job it is to deliver that care.
Yet how many C-suite leaders are aware of a smoldering discord that exists today between the healthcare establishment and its committed caregivers, who are too often referred to insensitively as simply providers?
COVID brought to light a disconnect between the profundity of the work our healthcare heroes do and the way the establishment treats them and dismisses their concerns. Healthcare’s administrative leaders need to take notice. There is something very wrong here.
More than providers
Let’s call them what they are. Our healthcare system’s caregivers comprise physicians, nurses, respiratory therapists, psychologists and the like who give their blood sweat and tears to keep patients functional, supported and alive — and never did they do so more than during the pandemic.
The term provider does not do them justice. It suggests they are akin to the service provider who changes your oil at a local Jiffy Lube or serves you a Happy Meal at your local McDonalds. The vast majority of our caregivers have shown themselves to be healthcare heroes during the pandemic. They remained in their hospitals for days on end, were moved around the country to places where clinical support was marginal to nonexistent and worked tirelessly and passionately doing what they were trained to do and what drives them: help people and save lives.
Initially, there were daily outpourings of thank you, applause and hero labeling to provide a modicum of support during the frenzy of the unknown. Then came the vaccines, which held the promise of eradicating the scourge. The caregiving heroes lined up and served as exemplars to elevate spirits and encourage people to get vaccinated, all while they continued working to heal those suffering from COVID-19.
Yet what happened next encapsulates a larger picture of how caregivers are minimized by our healthcare system and society.
Caregiver concerns minimized even as their lives were on the line
Things changed with the coming of vaccines. The Vaccine Adverse Event Reporting System (VAERS) began reporting side effects associated with the vaccines that raised concerns.a Now these findings were of course sensationalized, and in some instances distorted, by various individuals and groups to make points against vaccination. And although some of those criticizing the vaccines were caregivers, most caregivers continued to advocate for vaccines as a means to immunization against COVID-19.
Nonetheless, concerns mounted, and many caregivers had reasonable misgivings. Data were pourig out of every self-proclaimed research enterprise, and publications not yet peer reviewed were churning out both pro- and anti-vaccination rhetoric at a dizzying pace. Caregivers have a scientific background, and that includes a tendency to ask questions. But the questions kept coming, and it was hard to keep up:
- Would the mRNA vaccine affect caregivers of childbearing age? Does natural COVID infection provide immune protection?
- Should one be vaccinated after natural infection? Ninety days after the Delta variant? Five days after Omicron variant?
- Why were people mandatory proposing edicts to get vaccinated? Was the science sound or was fear driving the thinking?
Then the government stepped in. “Vaccinate or terminate” became the clarion call throughout healthcare facilities. Any caregiver belonging to a participating (state and/or facility-specific) healthcare domain (e.g., hospital, clinic, urgent care) was mandated to take the vaccination initially and then the booster — or be fired.
Why were our caregiving heroes singled out for this mandate? Why was it not overturned by the Supreme Court when President Biden sought to make vaccinations mandatory for everyone? They listened to big business, which declared it unconstitutional and argued that mandating vaccination would have dire economic consequences.
But our healthcare heroes — the folks most careful to keep social distance, wash their hands and wear personal protective equipment — were the ones who were singled out to be subject to a vaccine mandate, ignoring that they had a substantial census of vaccinees compared with other sectors of the general population.b
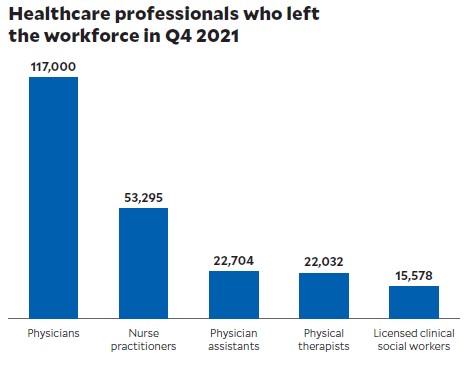
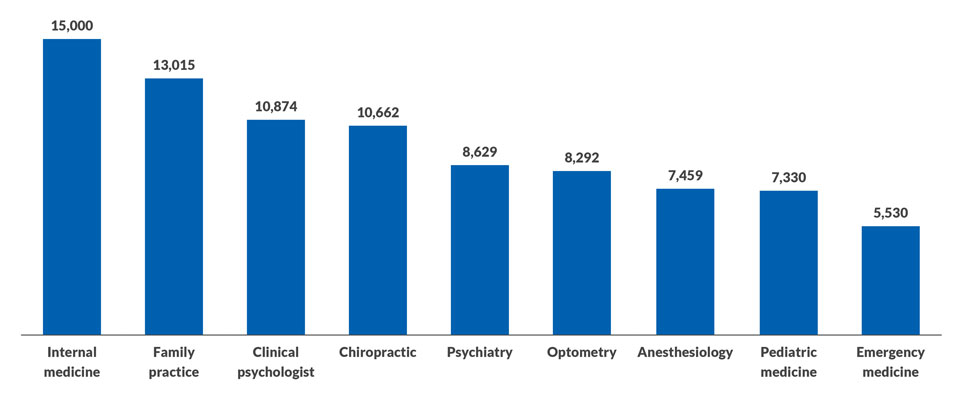
This policy likely contributed to the recent unprecedented healthcare exodus, where those that committed their lives to the most hallowed and noble of professions faded to black.c Making vaccination a mandate sent the message that the establishment would not even listen to the concerns of people who were putting their lives on the line.
Just one example of many
You may think I am being melodramatic, but I am not. This experience was just another way in which healthcare’s administrative leaders have been insensitive to needs and views of the very group of individuals who are dedicating their lives to helping humanity.d Here are other examples:
- Requiring caregivers to redefine a patient as a unit
- Reducing the time a caregiver can spend with a patient in order to meet quotas
- Making it necessary for caregivers to fight with insurance companies to authorize a procedure or lab test
- Requiring caregivers to adopt a specific pharmaceutical or instrument because the economics favor it.
Like it or not, these are the types of actions that sow discontent among caregivers and make them cynical about their organizations’ leadership.
These are the folks who know their craft better than any finance expert who transitions to healthcare from the retail sector, and they understand healthcare better than any executive who enters the industry from a leadership post in the oil or gas industry. The danger for such uninformed nonhealthcare leadership is the temptation to see the people delivering essential care as nothing more than providers.
This penny-wise and pound-foolish approach has had our healthcare heroes — now providers — clock in the units they treat per day, with the demands continuously increasing based on market share, CMS fee schedules and coverage metrics. Meanwhile, a substantial swath of the patient base is not getting better, continues repeatedly to visit clinicians and specialists, has incurred remarkable clinically related debt and has become part of the medical mud that we ignore but continue to tread upon. Our healthcare slice of the GDP increased from about 13% to 20% since the turn of the century, further cementing our nation’s dubious distinction as one of the greatest spenders on healthcare.
How to heal the rift
To reverse this trajectory, our healthcare system must first heal itself. This means truly reengaging with and appreciating our dedicated caregivers. We often talk about garnering trust between the doctor and the patient. But mending the trust and support between the doctor and healthcare’s administrative power structure is equally if not more important. If there is discord in that relationship, patients can notice it both viscerally and through verbal cues.
Healthcare finance leaders can make an enormous difference in mending this rift by embracing the following ideals.
Respect the healthcare hero. Show this respect not with lip service, media portrayals and the like, but with true deference to the understanding that each physician, nurse or other caregiver is a nonexpendable asset that provides incomparable value. Recognize that this person has committed to years of training to provide the unparalleled patient care that the healthcare industry expects. Finance leaders should keep in mind that caregivers choose measures like treatments, procedures and lab tests and other elements of care based on evidence-based information and years of practice and apprenticeship, and they should recognize how that experience provides additional dimensionality for understanding the healthcare costs incurred. This perspective can make room for an honest bidirectional discussion that reflects a shared commitment to maintaining excellent care with a sensitivity to the ever-changing landscape of healthcare economics.
Pay the price. COVID has created a major void in the healthcare skill set. This situation has led some members of the healthcare workforce to realize they can make more money and have more freedom if they work as a per diem rather than as a conventional employee. The result has unfortunately been greater cost to the healthcare system just to maintain functional and accredited staffing. The more far-sighted and frugal approach is to pay the price for key healthcare staffing needs, along with any incentives and fringe benefits that will keep them with the organization and mitigate human capital vulnerability that currently affects the market.
Engage government and politics. Healthcare finance leaders can play an important role in educating our nation’s policymakers to see how healthcare can encompass both economical and human value. They can advocate for greater governmental support of efforts to ensure caregivers can play a central and meaningful role in the creation of a more integrated healthcare system, involving increased collaboration among care delivery organizations, payers and nonhealthcare organizations that play an ancillary role in promoting health (such as community groups and organizations representing the food and transportation sectors). Such an approach would enable caregivers to direct patients to a broad range of resources that can help them maintain their health, thereby increasing their engagement. The result would be to increase caregivers’ satisfaction by engendering support that would enable them to deliver care with a sense of purpose and empowerment. Finance leaders also can raise policymaker’s awareness of the negative consequences of maintaining the status quo, including uncontrolled chronic disease, spiraling national healthcare costs and demoralized and burned-out caregivers.
A noble calling
Medicine is sacred. It is a vocation like no other. Among our nation’s caregivers, countless healthcare heroes are working tirelessly to touch body and soul, with a devout commitment to safeguarding life. Financial leaders can only benefit by recognizing and embracing this truth and forming a true partnership with their healthcare heroes in fulfilling this sacred charge.
Footnotes
a. Guo, W., et al., “Profiling COVID-19 vaccine adverse events by statistical and ontological analysis of VAERS case reports,” Frontiers in Pharmacology, June 24, 2022.
b. Farah, W., et al., “Disparities in COVID-19 vaccine uptake among health care workers,” Vaccine, April 26, 2022.
c. Yong, E., “Why healthcare workers are quitting in droves.” The Atlantic, Nov. 16, 2021.
d. Bluth, M.H., “Bringing the healthcare back to healthcare,” Cost Effectiveness of Health Report, March 2022.





