Survey: Understanding and mitigating risk in compensating physicians
Physicians, like many other healthcare workers, bring their expertise, dedication and commitment to their jobs. With physicians representing some of the frontline of the coronavirus (COVID-19) pandemic, ensuring that they are paid for all their hard work and sacrifice is more important than ever. But compensating physicians for their hard work can be a complex and challenging process for healthcare organizations, especially given the tight regulations that govern compensation and the unique nuances involved in physician and healthcare organization relationships.
To avoid financial risks and ensure compliance with laws and regulations, healthcare organizations must adopt sufficient and reliable physician compensation procedures and internal controls. Sound processes that identify, capture and exchange physician compensation information can increase compliance assurance as well as physician satisfaction, laying the foundation for building trust and strong working relationships between physicians and health systems.
To gain a better understanding of how healthcare organizations compensate their physicians, the Healthcare Financial Management Association (HFMA) surveyed a group of healthcare organization leaders in hospitals, health systems and physician practices. The online survey, conducted across two weeks in February, involved 101 respondents from around the country. Ludi sponsored the research conducted by HFMA. The following sections discuss key takeaways from the survey.
Provider organizations find opportunities to improve their processes
Almost half of healthcare organization leaders surveyed (45%) expressed that there may be areas to improve their physician compensation processes. Many of the concerns expressed center around two themes. The first relates to physician alignment. Several respondents were unsure whether their organizations were sufficiently capturing and documenting the data required to understand the success of their physician alignment strategies. The second theme deals with timeliness and whether compensation is in accordance with policies that relate to a physician’s contract.
“A lack of confidence in physician compensation processes is concerning because if an organization’s processes are not reliable and consistent, it can lead to compliance issues as well as physician satisfaction problems,” says Gail Peace, president and CEO for Ludi. “This in turn can have long-term implications for an organization’s ability to attract and retain physicians, as well as provide the best possible patient care. Hospitals need to do all they can to limit the uncertainty regarding all aspects in their relationship with their medical staff.”
Organizations find physician compensation processes to be cumbersome
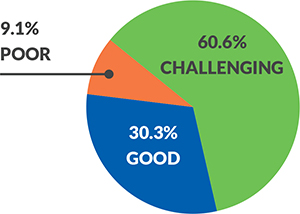
Fully 70% of leaders surveyed believe their processes to compensate their physicians are difficult, with 60% saying they are challenging and almost 10% indicating they are poor. “There could be many reasons for this,” says Peace. “If processes are still on paper or there are too many people and departments involved in compensation, or there is a lack of ownership across these departments, it can lead to clunky and inconsistent workflows.”
“The fact that so many healthcare leaders view their processes as cumbersome should be a red flag to provider organizations, prompting them to look ‘under the hood’ and pinpoint risks and opportunities for improvement,” says Peace. “This may entail deconstructing what’s not working, making sure the right people and departments are involved in improvement efforts and assigning ownership for compensation processes. Depending on the organization, representatives from legal, compliance, physician enterprise and finance should be included in any initiatives.”
Description of current process
Almost 10% of respondents characterize their current process as “poor.”
Having a true picture of physician expenditures is important
Physician expenditures (also known as physician spend) equals 5% to 10% of the average hospital’s net patient revenue, and this number is projected to grow at 5.4% annually.a This percentage can translate into millions of dollars for a hospital or health system.
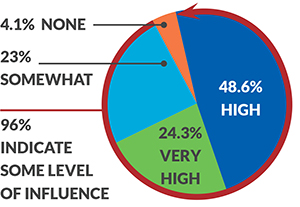
According to the survey, 96% of organizations consider physician spend when planning their budgets. Consequently, it is reasonable to assume that having a full and accurate appreciation of physician spend is important to ensure proper budgeting and strategic planning.
Influence of physician spend on organizational discussions about budget
96% of organizations indicate physician spend has some level of influence on budget discussions.
“Since nearly half of respondents have expressed dissatisfaction with physician compensation processes in their organizations, hospitals, health systems and physician practices may not have a complete picture of their entire physician spend and could be making budgeting decisions based on incorrect information,” says Peace. “At the same time, because a hospital’s physician compensation investment includes both employed and independent doctors (1099 employees), tracking this business area is not always clear cut. Without an effective and efficient program for managing and tracking physician compensation, organizations may find it hard to gauge the impact of their physician resource needs, which could impair judgement and increase the risks associated with long-term financial decisions.”
Automation may hold the key
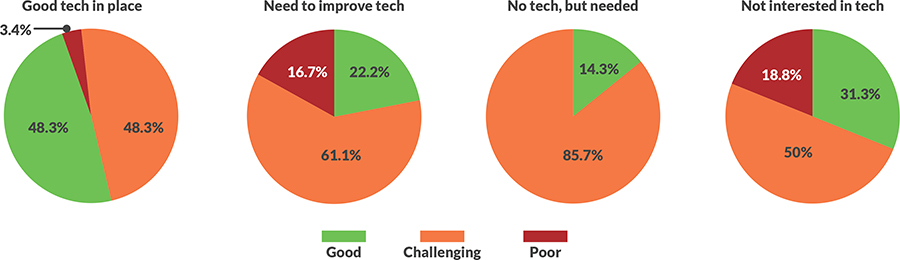
Technology investment appears to have a positive impact on an organization’s perceptions of how they compensate physicians. Respondents who have invested in physician compensation technology are 64% more likely to be very confident in the way they compensate their medical teams than respondents who haven’t made these investments. Moreover, organizations that are satisfied with their physician compensation technologies rate their current processes higher than organizations that don’t have automated solutions or are looking to improve the ones they have.
“Although two-thirds of organizations have invested in some sort of technology to improve their physician compensation processes, there appears to be an underinvestment in the right solutions,” says Peace. “The majority (51.7%) of respondents who are satisfied with their solutions still report challenging or poor processes, revealing a potential performance gap that could be closed with an updated or upgraded system. Automation is key to improving hospital-physician relationships and managing an organization’s total investment in their physician spend.”
Status of automation
Footnotes
a. Source: National Health Expenditure Projections, 2018–27: Economic and Demographic Trends Drive Spending and Enrollment Growth.” Health Affairs, February 20, 2019.
About Ludi
Ludi, Inc., is a healthcare technology and physician-advocacy firm that simplifies the way hospitals and health systems track, manage and audit payments to their physicians. Ludi’s team of physician advocates has helped more than 225 hospitals and health systems nationwide save millions of dollars, eliminate manual operational processes and stay within key compliance regulations. Visit Ludi at www.ludiinc.com.






