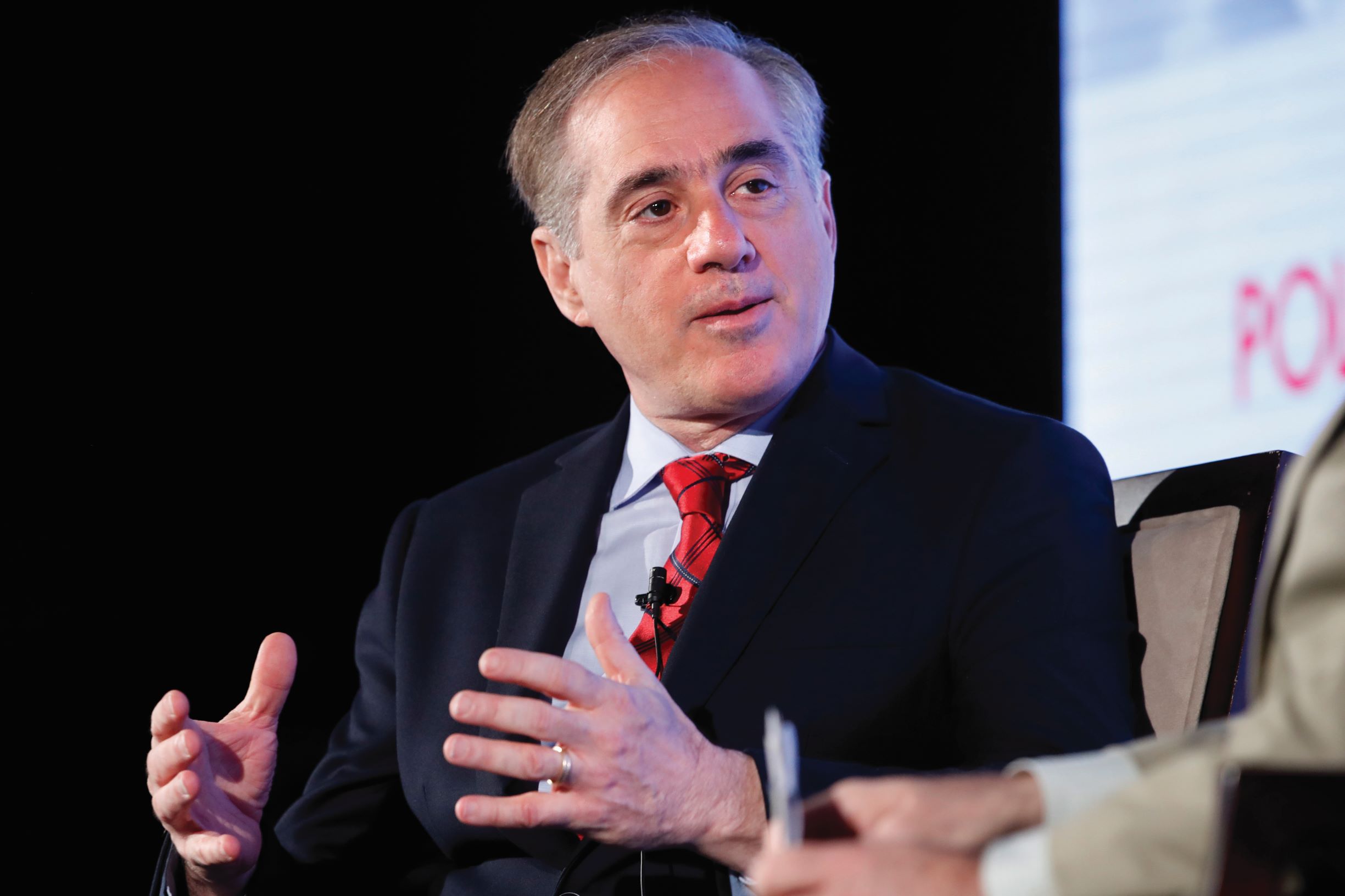
Enhanced care coordination provides a blueprint for optimal healthcare, former VA Secretary David Shulkin says

The U.S. healthcare system will thrive if leaders and policymakers take steps to promote holistic care and improved access, the former secretary of the Department of Veterans Affairs says.
When David Shulkin, MD, started working at the Department of Veterans Affairs (VA) in 2015, he was struck by the differences in the provision of care compared with what he’d seen in the private sector.
Conventional wisdom may suggest that care delivered in the private sector is more innovative and forward-thinking relative to a government-based model. But in many ways, Shulkin found, the opposite was true.
“I thought I was going to be bringing my best practices from the private sector to the government, and adding value that way,” said Shulkin, who served in the cabinet of President Donald Trump as secretary of the VA from January 2017 to March 2018.
“While there were some practices that I brought in, I actually learned a lot more about the ability to deliver population healthcare from a government perspective that now I’m taking back out to the private sector.”
As Shulkin sees it, the key is to combine the strengths of the VA and the private sector. The result would go a long way toward promoting comprehensive care and ending the type of fragmentation that defines many care experiences.
In a pair of interviews, Shulkin reflected on various issues facing the U.S. healthcare system. An underlying theme was the need to enhance customer service by improving care coordination.
The response to COVID-19
Among hospitals and other providers, the leadership response to the coronavirus pandemic has been “incredible,” Shulkin said. He cited early steps such as delaying elective surgeries to accommodate COVID-19 patients, creating unprecedented surge-capacity plans and seeking out innovative supply chain solutions. “We’re seeing the best of what American healthcare can do.”
Yet significant issues hampered the response, Shulkin said in late March. The lack of equipment was a big concern, even as manufacturers stepped up to try to address that need.
Staffing was a potentially more insurmountable obstacle. Based on past studies, he said, 35% to 50% of staff are unavailable or unwilling to work when a pandemic reaches its peak. “This is where we’re going to see the limitations of what our healthcare system can do in response to a pandemic.”
Preparation for future public-health emergencies
After the COVID-19 outbreak subsides, Shulkin anticipates a more widespread acceptance of the role of government in ensuring the safety and health of citizens. People are seeing that in a public health crisis, “It really is government that they rely upon not only to set the rules and the policies, but to answer the need for large populations,” he said.
The change in outlook also will entail a greater focus on establishing an integrated healthcare system and ensuring equitable access, Shulkin said. “You recognize that viruses like this do not discriminate based on socioeconomic status. I think it’s going to reframe the way that people view healthcare, public health and government.”
Emergency preparedness will become more of a focus. “In the VA, it was one of our missions to train and prepare for emergencies,” he said. “I think that’s going to become a core competency of healthcare leadership in the future.”
Other changes likely will involve telehealth, which has the potential to significantly improve care access and the patient experience if utilized well, Shulkin said. In response to the pandemic, CMS issued Section 1135 waivers that alleviated regulatory barriers to effective telehealth.
“It’s going to be hard to step back to regulations and reimbursement policies that frankly never really made a lot of sense if your goal was to take better care of patients,” Shulkin said.
Patient access
At the VA, which provides care for veterans starting when they leave service and continuing for the rest of their lives, “The lifelong approach to population health is very different than what many people see in the private sector,” Shulkin said in an earlier interview.
The healthcare industry long has struggled to guarantee adequate access to care. Shulkin said the concern is not merely about convenience, but more about ensuring that patients with urgent clinical issues can get care immediately — and not just at the nearest emergency department.
Shulkin joined the VA as undersecretary for health in 2015, when the agency was coming under fire for lengthy delays in the availability of appointments. He addressed the problem by making sure those with urgent clinical concerns were given top priority, eventually implementing same-day access to both physical and mental healthcare for those cases.
Another step was to publish wait times for appointments, a key aspect of being accountable to patients.
“To my knowledge, the VA is still the only health system in the country that publicly publishes its wait times,” Shulkin said. Data indicate that the VA’s wait times improved significantly from 2016 to 2018, he noted, while those in the private sector stayed flat.
A drawback of the VA model is the ability to treat only the veteran rather than the family unit. “So much of care happens in the family,” Shulkin said. “The more that we can look at how the healthcare system interacts with not only the patient but the whole unit of support around them — family, friends, community — the stronger our outcomes will be.”
Payment systems
A fundamental step toward improving care coordination and population health management is establishing a better payment system, Shulkin said.
Many industry observers can recite a litany of issues with fee for service, but Shulkin noted that past experiences with pure capitation — or with any system that assigns risk to only one party — have been problematic as well.
“We need to create a new model for reimbursement …. a hybrid system,” Shulkin said. His ideal model:
- Rewards productivity and innovation
- Incorporates components that truly impact outcomes
- Engages patients
The long-standing conflict of interest between payers and providers needs to be resolved, Shulkin added, whether through new contracting strategies or possibly formal joint-venture arrangements. “We can’t just be using language that sounds good. There has to be a true alignment of the clinical and economic goals and objectives for those types of partnerships to work. That’s going to be necessary to achieve the type of healthcare system that we want.”
Behavioral health
In his work at the VA, Shulkin knew he had to make behavioral health a top priority for those whom the department served. He wants it to become similarly urgent for the industry at large.
“Our behavioral healthcare system is probably one of the least effective parts of our system today,” he said. Among the problems:
- The science of brain health lags the study of other organs.
- Behavioral research has been dramatically underfunded in relation to, for example, cardiovascular research.
- Payment systems create a fragmented care approach in which behavioral healthcare is poorly incorporated with other types of care.
“One of the things that the VA has done — not having some of those barriers to reimbursement — it’s really worked to integrate mental health and physical health,” Shulkin said.
That concept entails delivering some behavioral healthcare in the primary care setting as part of an integrated team approach. Other key components include:
- Expansive use of telehealth, especially in areas with a shortage of specialists
- Provision of treatment in residential facilities in areas where that level of service is hard to find in the private sector
The EHR
The electronic health record (EHR) was an area in which Shulkin strived to infuse the VA with private-sector innovation. He sought to reallocate more than $700 million in FY18 federal funding to overhaul the VA’s EHR. The hope was to install a system that would allow for greater interoperability with community hospitals, many of which care for veterans. After Shulkin’s departure, the VA signed a contract with Cerner.
In Shulkin’s mind, the lack of interoperability in healthcare is not primarily a technical problem, but rather an issue with the business model. The industry should establish strict standards to prevent information blocking by technology vendors, he said.
He added, “I’m strongly advocating for the adoption of a common clinical data set that would be in the public domain, like at the National Library of Medicine, so that everybody understands a common set of definitions for sharing data.”
Technologically, Shulkin hopes something like the Fast Healthcare Interoperability Resources (FHIR) can be adopted as a common standard for data sharing. And application programming interfaces (APIs) should be made open to encourage creativity and innovation among entrepreneurs in the health-record space.
The role of financial leadership
The task of shoring up the nation’s healthcare system financially never has been more urgent and more daunting than it will be coming out of the COVID-19 pandemic, Shulkin said.
The economic consequences of the pandemic remain to be seen but figure to be profound. Shulkin’s projections indicate somewhere around a $500 billion impact on hospitals from factors such as the cancellation or postponement of elective surgeries, the closure of some physician practices and ambulatory facilities, and increased expenditures on vital supplies and staffing.
Already-thin margins will shrink further, and nonoperating revenue likely is taking a hit in the volatile stock market. “Many hospitals will have liquidity issues and have to redo a cash balance plan, will need to rethink capital investments and create new budgets because of this crisis,” Shulkin said.
The March stimulus bill included $100 billion in hospital funding. That pool will be helpful but most likely not enough to significantly blunt the impact, Shulkin said.
“This is going to be something that our financial officers and management teams are going to be dealing with for quite some time,” he said.
6 things about David Shulkin, MD
1. He was the country’s ninth secretary of Veterans Affairs (VA), heading the department for the Trump administration from January 2017 to March 2018.
2. Before that, he served in the department as undersecretary for health starting in 2015, when President Barack Obama asked him to help address the wait-time crisis afflicting the department.
3. He brought vast executive experience in the private sector to his roles in the VA. He was president and CEO of Beth Israel in New York City and president of Morristown Medical Center in New Jersey.
4. He had stints in clinical leadership with several organizations, including the Hospital of the University of Pennsylvania and then the University of Pennsylvania Health System.
5. After leaving the VA, he returned to the private sector as chief innovation officer at Sanford Health in Sioux Falls, South Dakota.
6. He also wrote the 2019 best-seller It Shouldn’t Be This Hard to Serve Your Country, which describes his efforts to navigate political challenges and implement changes at the VA.





