Minimizing Readmission Penalties with Palliative Care
Increasing costs and less-than-optimal outcomes have plagued U.S. healthcare leaders for years and ushered in the era of value-based care programs that factor cost and quality into payment calculations. One of the first of such programs is the Medicare Hospital Readmission Reduction Program (HRRP), which reduces Medicare payments to hospitals with excess 30-day readmissions, up to 3 percent of total Medicare payment the facility would otherwise receive. Since the HRRP began in 2013 (using 2012 readmission performance data), more than half of U.S. hospitals have seen reductions in their Medicare revenue in all five years of the program. a
Hospitals have deployed various strategies to reduce readmissions, including adding case managers/wellness coaches, narrowing the post-acute care network, and enhancing medication reconciliation. Nonetheless, many continue to face revenue reductions due to excessive readmissions. In 2017, for the performance period beginning June 2012 and ending July 2015, 79 percent of hospitals faced a financial penalty for their readmission performance. b
One solution to the readmissions problem that hospitals are increasingly adopting to good effect is palliative care—specialized care that focuses on providing relief from symptoms and stresses for patients living with serious illness and their families. This type of care is appropriate at any age and any stage of serious illness, and can be provided concurrently with curative treatment. Typically, physicians approach medical problems by attending to discrete organ systems in silos; palliative care teams work to improve the quality of life for the patient as a whole person.
Palliative Care and Its Growth
Palliative care is a team-based approach to care involving specialty-trained physicians, nurses, social workers, chaplains, and other specialists. In hospitals, palliative care is predominantly offered through a consultative team model, but it also can be delivered through co-management models or through an inpatient palliative care unit. As patient’s needs go beyond the walls of the hospital, palliative care also is provided across the continuum of care in settings such as nursing homes, office and clinic practices, and patients’ homes. c
In 2000, little more than 20 percent of U.S. hospitals with 50 or more beds had palliative care programs; by 2015, three-quarters of such hospitals had palliative care programs. d For hospitals with 300 or more beds, that figure jumps to 90 percent. There has been similar growth in palliative care team staffing with 44 percent of hospitals reporting complete interdisciplinary palliative care teams (physician, advanced practice or other registered nurse, social worker, and chaplain). Further, the total number of dedicated FTEs in hospitals with fewer than 150 beds grew by 31 percent from 2009 to 2015 and by more than 50 percent in hospitals with 300 or more beds, according to research conducted by Center to Advance Palliative Care and the National Palliative Care Research Center. e However, despite these increases in staffing levels, many programs are still not adequately staffed to meet patient need. f
Palliative care physicians and appropriate clinicians can bill Medicare Part B for their services under fee-for-service, but this revenue covers only a fraction of the team’s efforts. Hospitals continue to invest in palliative care because of the strong value that such a program delivers.
The Benefits of Palliative Care to Hospitals
Palliative care has been shown to simultaneously improve quality and satisfaction and decrease spending, making it an attractive program for healthcare organizations. Consider these findings from published studies:
- The average per-patient per-admission net cost saved by hospital palliative care consultation has been estimated as $2,659. g
- Inpatient palliative care results in significant improvements in pain scores and symptom burden, with the improvement holding after discharge. h
- Families of patients who receive a hospital-based palliative care consultation rate the quality of care higher than do families of patients who do not receive palliative care. i
- Early palliative care consultation reduces total length of stay and total costs among patients in the advanced stages of cancer. j
The Impact of Palliative Care on Readmissions and HRRP Penalties
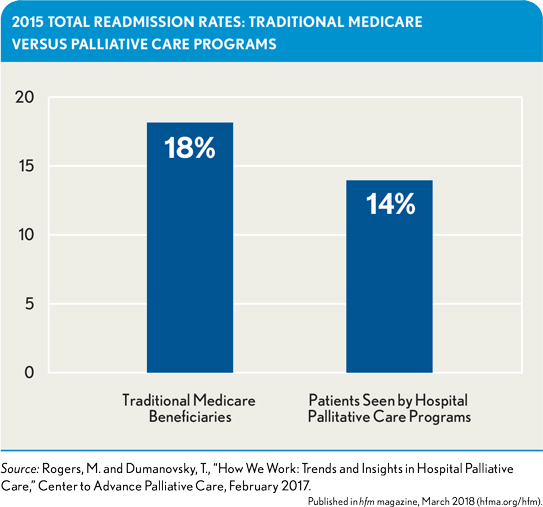
Currently, the Centers for Medicare & Medicaid Services (CMS) considers only selected diagnostic categories in its calculations for the HRRP program (i.e., acute myocardial infarction, chronic obstructive pulmonary disease, heart failure, pneumonia, total hip/knee arthroplasty, and coronary artery bypass graft). Although it is uncertain whether additional diagnoses will be added to the program going forward, private health plans have followed suit and are evaluating—and financially rewarding—their network hospitals for overall 30-day readmission rates, regardless of diagnosis. Inpatient palliative care consultations have been correlated with lower overall readmission rates. k Nationwide, the Center to Advance Palliative Care and the National Palliative Care Research Center found that palliative care programs report an average readmission rate of only 14 percent for their patients compared with a total Medicare readmission rate of 18 percent, as shown in the exhibit below.
Why Palliative Care Reduces Readmissions
With its proven ability to reduce readmission rates for seriously ill patients, palliative care has the potential to reduce penalties and improve performance for hospitals. Palliative care professionals work as an interdisciplinary team—spanning medicine, nursing, social work, and chaplaincy—to effectively address the sources of distress a patient experiences during a serious illness. This approach to care involves expert management of pain and other symptoms such as shortness of breath, fatigue, and nausea. Too often in traditional care, these symptoms are under-treated, leading to undue distress following discharge and a return to the emergency department (ED) and hospital. A 2017 study of patients with cancer showed that 53 percent of ED visits were related to symptoms that could be managed on an outpatient basis. l
Palliative care also relieves distress by assisting both the patient and family with decision making. Palliative care professionals ensure an understanding of disease progression and prognosis, and then work with both the patient and family to clarify care priorities and match treatment and services to those goals. Unfortunately, too many practicing physicians find such conversations challenging. A 2016 survey of physicians who regularly treat Medicare beneficiaries revealed that nearly half (46 percent) frequently or sometimes feel unsure what to say when helping patients to plan ahead. m Yet avoiding conversations about goals and the quality of life deprives patients of both knowledge and a feeling of control, which empower them following discharge.
It is important to note that effective communications need not be limited to palliative care specialists. In fact, certified palliative care specialists currently are in short supply, making it essential to equip selected clinicians with effective communication skills so that the specialists remain free to focus on the patients with the greatest need, such as those with intractable symptoms, compromised function, and/or overwhelmed caregivers.
Next Steps
Palliative care has proven beneficial for patients with serious illness, and by ensuring those patients access to high-quality palliative care, hospitals also may benefit financially under the HRRP. Hospitals without palliative care programs should consider this and other benefits when creating palliative care strategies, while hospitals that currently offer this type of care should ensure that the right patients can easily access this expertise in a timely manner.
Allison Silvers, MBA, is vice president, payment and policy, Center to Advance Palliative Care, New York.
Maggie Rogers, MPH, is senior research associate, Center to Advance Palliative Care, New York.
Footnotes
a. Thompson, M.P., Waters, T.M., Kaplan, C.M., Cao, Y., Bazzoli, G.J., “Most Hospitals Received Annual Penalties for Excess Readmissions, But Some Fared Better Than Others,” Health Affairs, May 2017.
b. Boccuti, C., and Casillas, G., “Aiming for Fewer Hospital U-Turns: The Medicare Hospital Readmission Reduction Program,” The Henry J. Kaiser Family Foundation, March 10, 2017.
c. Kamal A.H., Currow D.C., Ritchie C.S., et al., “Community-based palliative care: the natural evolution for palliative care delivery in the U.S.,” Journal of Pain and Symptom Management, August 2013.
d. Cassel J.B., Bowman B., Rogers, M., et al., “Palliative Care Leadership Centers Are Key to the Diffusion of Palliative Care Innovation,” Health Affairs, February 2018.
e. Rogers M., Dumanovsky, T. How We Work: Trends and Insights in Hospital Palliative Care. The Center to Advance Palliative Care and the National Palliative Care Research Center, February 2017.
f. Spetz J., Dudley N., Trupin L., Rogers M., et al., “Few hospital palliative care programs meet national staffing recommendations,” Health Affairs., Sept. 1, 2016.
g. Morrison R.S., Penrod J.D., Cassel J.B., et al. “Cost savings associated with U.S. hospital palliative care consultation programs,” Archives of Internal Medicine, Sept. 8, 2008.
h. Kavalieratos D., Corbelli J., Zhang D., “Association Between Palliative Care and Patient and Caregiver Outcomes: A Systematic Review and Meta-analysis,” Journal of the American Medical Association, Nov. 22, 2016.
i. Casarett D., Shreve C., Luhrs K., et al., “Measuring families’ perceptions of care across a health care system: preliminary experience with the family assessment of treatment at end-of-life short form (FATE-S),” Journal of Pain and Symptom Management, 2010 .
j. May, P., “Earlier Palliative Care Consultation May Reduce Hospital Cost, Length of Stay,” Journal of Clinical Oncology, 2015.
k. O’Connor N.R., Moyer M.E., Behta M., and Casarett D., The Impact of Inpatient Palliative Care Consultation on 30-Day Hospital Readmissions. Journal of Palliative Medicine, Nov. 18, 2015;
l. “ASCO 2017: Many Emergency Department Visits Among Patients With Cancer Appear Preventable,” The ASCO Post, June 7, 2017.
m. Perry Undem Research, Physician Views towards Advance Care Planning and End-of-Life Care Conversations , April 2016.





