Paul Keckley: 2 major changes in the value agenda require finance leaders’ attention

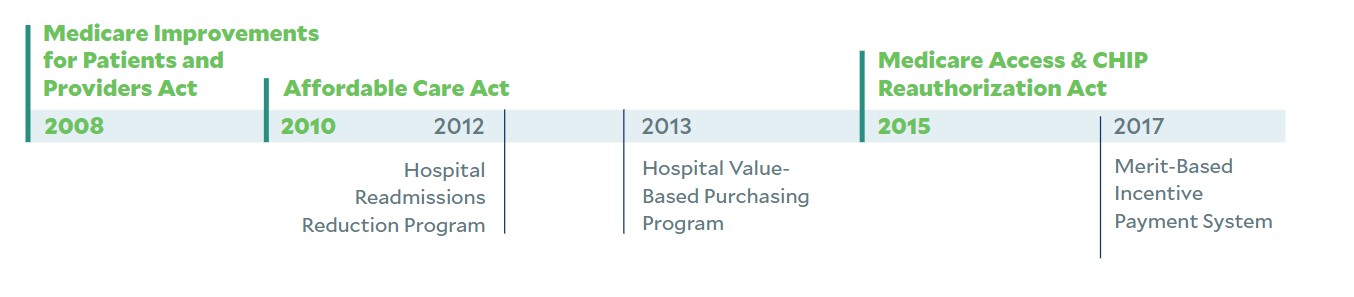
For the past 15 years, the U.S. healthcare system has sought to reduce spending and improve quality by changing incentives from volume to value. Primarily through its fiduciary control of Medicare and authority granted the U.S. Department of Health and Human Services and other federal agencies, the nation has seen numerous key laws passed with bipartisan support to advance better care at a lower price. And still pending, despite continuing bipartisan support in the 117th Congress is the Value in Health Care Act (HR 4587), introduced by Rep. Peter Welch (D-Vermont) in 2021.
In tandem, CMS implemented a flurry of programs to codify the value agenda, including more than 50 alternative payment models (APMs) piloted since 2013. Notably, these efforts spanned three administrations, also garnering bipartisan support and widespread voluntary participation among provider organizations. But the results of all these initiatives are mixed.
U.S. legislation (in green) and regulatory initiatives (in black) aimed at promoting value-based payment, 2008-22
To date, quality improvements have been significant around care coordination, but cost savings have been modest. In a white paper issued in October 2021, the Center for Medicare & Medicaid Innovation reported, “Over the last ten years, only six out of more than 50 models launched generated statistically significant savings to Medicare and to taxpayers, and four of these met the requirements to be expanded in duration and scope.”a
Case in point: On Aug. 30, CMS released 2021 results for the performance of accountable care organizations (ACOs) under its Medicare Shared Savings Program (MSSP) — arguably the flagship of its value agenda. It reported ACOs had saved Medicare $1.66 billion, with 99% of ACOs meeting quality standards and 58% earning a shared savings bonus.b
But Meena Seshamani, MD, PhD, CMS deputy administrator and director of the Center for Medicare, noted that annual savings dropped from $2.3 billion in 2020.
Nonetheless, CMS has set a goal that 100% of people with traditional Medicare will be part of an accountable care relationship by 2030.c
What’s ahead
The value agenda in U.S. healthcare is critical to its future, but redirection is likely in two areas.
1 Increased emphasis on APMs that produce the highest Medicare cost savings. Funding for the Medicare program is not sustainable: As Rachel Burton, senior analyst for the Medicare Payment Advisory Commission, noted in a recent presentation, the numbers of workers contributing to the Medicare Program through payroll taxes has dwindled over the years.d In 1970, more than 4.5 workers contributed to the program through their payroll tax to fund care for one beneficiary; today, the ratio is 2.9 workers per beneficiary. Burton suggested that to sustain the Medicare Hospital Trust Fund (Part A) another 25 years, the government might need either to raise the percentage of the workers’ pay from today’s 2.9% to 3.66% or to decrease Medicare
Part A spending by 16.9%, or $69 billion per year.
Thus, streamlining the APM options, modifying benchmarking and risk methodologies and moving toward mandatory participation are likely changes that would stimulate greater Medicare cost savings. Two-sided risk in direct contracting, bundled payment and MSSP programs is inevitable along with possible limits on the roles business partners play in clinical and administrative governance. In tandem, CMS will pursue closer alignment among terms of participation, network adequacy and coverage requirements in Medicare Advantage plans and the Medicare value agenda. The bottom line is that reducing Medicare spending is as important as improving quality in the value agenda to quality improvement, and it is clearly urgent.
2 Expanded participation in high-value programs by Medicaid, large employers and private insurers. CMS can be expected to reach beyond Medicare to standardize its value agenda in other settings. Through negotiations with state regulators and partnerships with the private sector, CMS will enact mechanisms whereby the most effective value programs are adopted.
Considerations for finance leaders
Given near-term financial pressures resulting from the pandemic, higher supply chain and workforce operating costs and a slow economic recovery, organizations might be inclined to delay or suspend pursuit of value-based initiatives. To do so is risky. The value imperative has fundamentally changed the retail, transportation, higher education and insurance industries. It has found its way to healthcare services.
Value is defined by Webster’s as “the monetary worth of something” and “a fair return or equivalent in goods, services, or money for something exchanged.” In essence, it is the relationship between what something costs and the benefits that accrue to the purchaser.
In healthcare, consumers, employers and the government are the purchasers. Hospitals, physicians and ancillary services are producers, and insurers are intermediaries. Today’s purchasers demand more value from the healthcare system in terms of things like price transparency, underlying costs and expected outcomes.
It’s an uncomfortable position for healthcare finance leaders who must balance the reality of declining operating margins with the inevitable need to invest in a value strategy. But the decision not to make those investments is more problematic.
Footnotes
a. CMMI, Innovation center strategy refresh, October 20, 2021.
b. CMS.gov, “Medicare Shared Savings Program saves Medicare more than $1.6 billion in 2021 and continues to deliver high-quality care,” Press release, Aug. 30, 2022.
c. Folger, S., et al. “Pathways for specialty care coordination and integration in population-based models,” CMS.gov, Jun. 17, 2022.
d. Frieden, J., “MedPAC Members Concerned About Medicare’s Finances,” Medpage Today, Sept. 1, 2022.





