States advance hospital price caps
Price cap bills remain active in two states' currently underway 2026 legislative sessions.
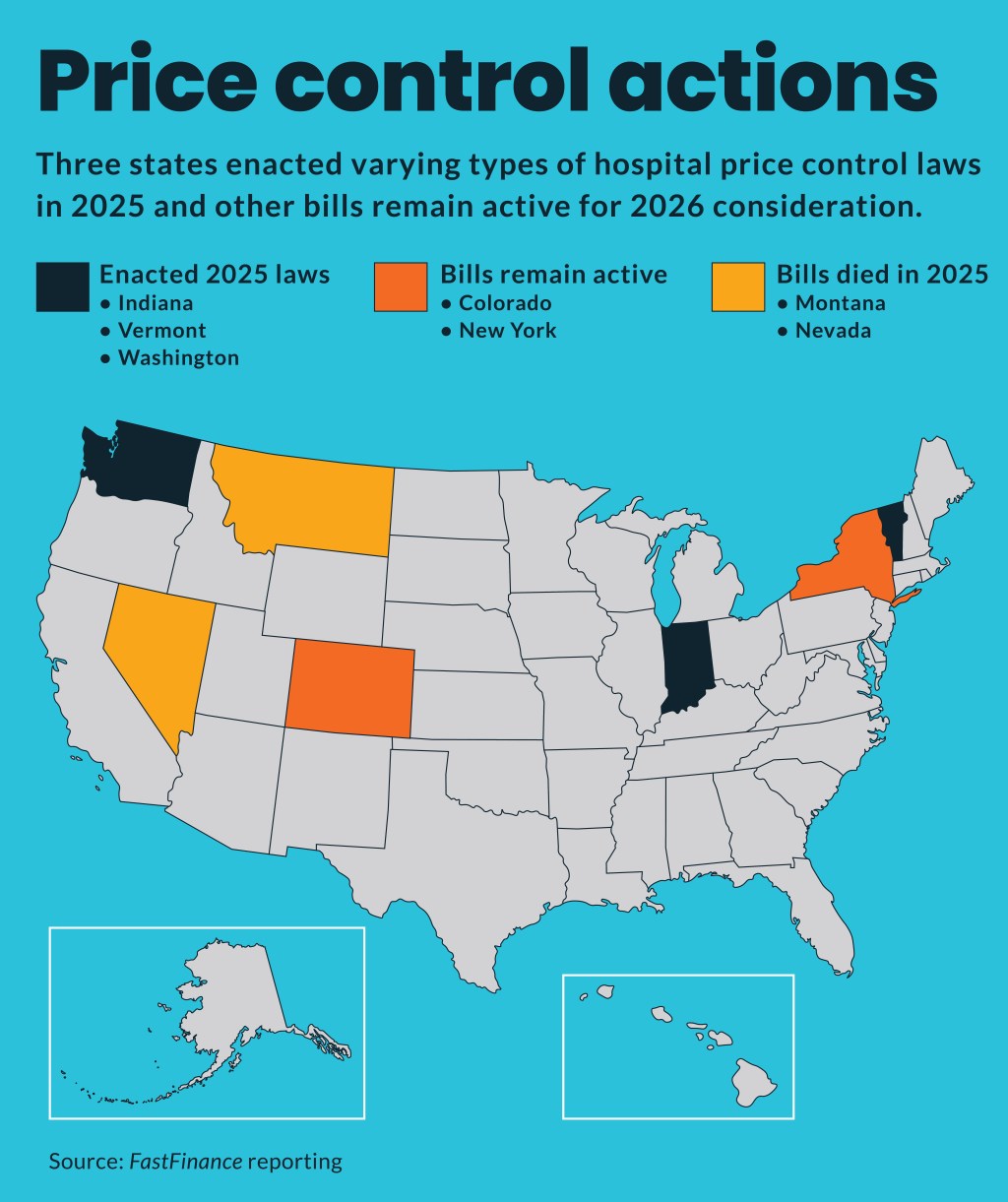
Three states enacted hospital price caps in 2025 and more could act this year.
The new state laws varied widely but all targeted some type of limit on hospital prices.
Indiana
The highest profile new law came in Indiana. That law (HB1004) went into effect in July 2025 and imposes price controls and additional price transparency requirements on the largest Indiana not-for-profit health systems. Key dates include:
- July 1, 2026: Not-for-profit health systems will have to submit annual audited financial statements, federal tax forms and related data to the state; state studies and reports inpatient and outpatient hospital pricing to determine the statewide average cost of care.
- June 30, 2029: Not-for-profit health systems are required to align their prices at or below the statewide average or risk losing nonprofit tax status.
- Sept. 1, 2025: Not-for-profit health systems must offer a direct-to-employer healthcare arrangement at no more than 260% of Medicare rates.
The law was enacted over the objections of the Indiana Hospital Association (IHA), which recently highlighted new data “showing a clear downward trend in Indiana health care costs and hospital prices.”
For instance, recent rankings from WalletHub showed the state ranked as the eighth best in the nation for healthcare costs — up from 15th best in 2021.
“Indiana hospitals are committed to making care more affordable without compromising quality,” said Scott Tittle, JD, president of IHA. “These rankings reflect the hard work and collaboration happening across the state to lower costs and improve access for Hoosiers.”
Washington
Another price cap law enacted in Washington state, which goes into effect in 2027, will limit hospital prices for plans covering state and public school employees.
For such public employees, the measure limited in-network hospital rates to 200% of Medicare rates and limits out-of-network hospital rates to 185% of Medicare.
Supporters said the measure was based on a similar law implemented in Oregon in 2019.
Recently published research credited the Oregon law with generating $50 million in annual savings for the state and resulted in “small and nonsignificant changes in Oregon hospitals’ revenues, expenses and margins after implementation of the cap.”
But an Oregon hospital advocate blamed the law for deteriorating finances at those facilities and multiple subsequent hospital closures.
“This research is disconnected from reality and tone deaf, coming at a time when half of Oregon’s hospitals are consistently operating in the red,” said Becky Hultberg, president and CEO, Hospital Association of Oregon. “In the final weeks of 2025 alone, two Oregon hospitals announced the closure of inpatient beds. Oregon’s health care system is in crisis. A cascading series of well-intentioned but disconnected policy choices, including rate caps, are challenging hospitals’ ability to continue to care for patients in their communities.”
Vermont
Also in 2025, Vermont enacted a law that tasks the existing Green Mountain Care Board (GMCB) to set healthcare provider rates through Medicare-based price caps by FY27, establish global hospital budgets for non-critical access hospitals by hospital FY27 and for all hospitals by FY30.
Hospitals are required to provide advance notice of any service eliminations and the GMCB can modify hospitals’ budgets or take other appropriate action “to preserve access to necessary services.”
“Vermont’s entirely not-for-profit hospitals system is deeply concerned about affordability and to address these concerns, we are making operational changes,” said Mike Del Trecco, CEO of the Vermont Association of Hospitals and Health Systems. “Part of the changes must include payment models that fairly and accurately pay for care.“
Did not advance
Several other state legislatures also considered various types of hospital price caps but did not pass them in 2025, including:
- Colorado
- Montana
- Nevada
- New York
Nevada and Montana have no regular legislative sessions in 2026 but the other two states already have started their 2026 sessions.
The Colorado bill would cap reimbursement rates based on Medicare rates for larger hospitals under the state employees’ health plan and for small employer group plans.
The New York bill would cap how much hospitals can bill for outpatient care, especially for services that otherwise could be provided in less expensive settings such as clinics or urgent care centers.





