Clinical audits and denials impact 3% or more of NPR being held in reserve
Clinically avoidable denials continue to impact revenue, slow cashflow and increase bad debt, yet CFOs have limited insight into why these denials occur and how to avoid them. Half of healthcare organizations hold more than 3% of total net patient revenue (NPR) in reserves each fiscal year in anticipation of denials claims, with over a third holding back greater than 5%. However, less than a quarter of organizations track trends related to clinically avoidable denials.
This finding was identified in a 2022 HFMA survey of 317 healthcare finance, accounting and revenue cycle executives, sponsored by MRO. Other results included:
- Only 7% of respondents receive more than 71% of their government and commercial claim audits electronically.
- 36% of respondents use Excel spreadsheets to track audits and denials.
- Nearly all (90%) of respondents say it’s ‘somewhat’ or ‘very’ essential for all systems that touch the revenue cycle to share data.
Understanding the impact of clinically avoidable denials
“If you’re holding back more than 5%, it’s time to step back and say, ‘Why?’ What are the root causes of denials and write-offs?” said Dawn Crump, MA, CHC, SSBB, senior director of revenue cycle solutions at MRO. “You need to start digging into the data. Even when you’re holding back 3% of NPR, that’s a significant amount of revenue.”
Unfortunately, many organizations lack the insight necessary to take a proactive approach to denial management, said Crump. A rudimentary denial tracking system, lack of interoperability between systems that touch the revenue cycle and siloed teams often stand in the way of progress, she added.
Despite these challenges, now is the time to address clinically avoidable denials — particularly as healthcare organizations continue to rebuild both financially and operationally in the wake of COVID-19, said Crump.
“Healthcare staffing shortages make it difficult to manage audits and appeals effectively, resulting in lost revenue opportunities as well as lost opportunities to learn from mistakes,” she added.
Clinically avoidable audits, denials on the rise
While government audits of high-volume claims used to have the biggest impact on healthcare organizations, now that impact has shifted to include more commercial and managed care audits, said Crump.
“Commercial and managed care audits have grown by 56% year over year for the last few years, according to MRO’s internal data. That’s even during COVID,” she said. “If you’re not tracking, trending and consolidating audit information, you’re potentially missing out on big trends.”
Pre-payment audits are also rising and continue to affect accounts receivable, said Crump.
“While not an official denial, you’re also not getting paid in a timely manner,” said Crump. “ They not only affect your aging AR with payments aging beyond 90 days; they also cause challenges in tracking the reasons for underpayments.”
Moving away from manual tracking
One reason healthcare organizations continue to struggle with clinically avoidable denials is that they don’t track and trend information on why claims are denied.
“Organizations could be using an EHR that doesn’t allow them to get down to that root cause granularity,” said Crump. “Another reason is that the denial management process is managed across three or four departments that don’t use the same or the right tools. Trying to consolidate this information to identify trends is tough.”
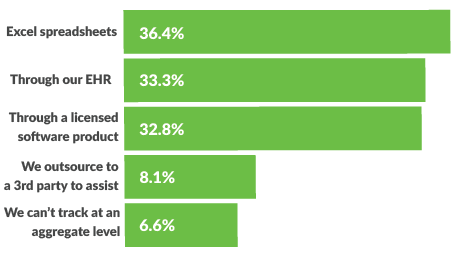
How are you currently tracking your health system’s audits and denials from government and commercial payers?
Consolidating information is particularly tough for those organizations using manual tracking (e.g., in spreadsheets). Aside from being more prone to error, spreadsheets make it difficult to work across teams, said Crump.
“Even in a smaller organization, you’re typically working with at least three departments — case management or clinical appeals, finance and compliance,” she said. “Trying to coordinate efforts even using a shared drive can cause some challenges.”
When organizations use Excel, they also cannot take advantage of automation or distribution methods and “could spend days just generating and distributing reports,” said Crump.
How are you currently tracking your health system’s audits and denials from government and commercial payers?
Drilling down into root causes of denials
While some EHRs provide the ability to track audits and denials, healthcare organizations often require a more nuanced approach.
“That’s because audits and denials are very specialized in terms of time frames, reporting and drilling down into the root cause,” said Crump. “Organizations often need something more tailored to ensure their financial work queues are designed to address the nuances of denial management.”
Receiving audits electronically
Being able to receive audits electronically sets up organizations for success.
“Paper mail is so delayed. Even after receiving the mail, organizations must scan and send that information to the right department,” said Crump. “The audit clock starts ticking based on the date of the letter.“ The more you can move toward that electronic receipt, the more time you’re giving yourself to provide the best response.”
Working with a vendor that is also a designated CMS health information handler can speed up the process because “this designation means that the vendor can receive CMS requests electronically as well as distribute necessary information electronically,” said Crump.
Addressing interoperability challenges
Reducing clinically avoidable denials also requires data sharing between disparate systems, including audit and denial software, EHRs, payers, government auditors, financial systems, contracting, health information management and others.
“Even when data sharing is in place, keeping data in sync and avoiding duplicate data entry is a challenge,” said Crump. “But there are a lot of opportunities to achieve interoperability that don’t entail a large technical investment. That’s where partnering with a vendor that specializes in audit and denial workflow can help.”
Overcoming siloes
Reducing clinically avoidable denials is not only about technology. It also requires ongoing collaboration and even consolidation between denial and audit teams, according to Crump.
“With staffing shortages, it’s important to find efficiencies,” she said. “The overall workflows are similar between audits and denials in that you need a combination of clinical, coding and financial expertise.”
Sharing knowledge internally is also important — particularly when specialized audit teams focus on certain payers.
“We need to get out of our own way and centralize the knowledge,” said Crump. “What is happening on the government side is most definitely happening with commercial payers as well.”
Effective denial tracking makes financial sense
Not all denials are preventable, and so setting aside a portion of NPR in reserve makes sound financial sense, as well as finding ways to lower reserves.
“Forming a central revenue integrity function can support better tracking and management of denials while improving collaboration efficiency,” said Crump. “Moving from manual tracking to configurable systems designed for audits and denials that support electronic data transfer and team collaboration are all steps organizations can take today.”
About MRO
MRO, a leading clinical data release platform and the KLAS-rated No. 1 provider of release of information (ROI) solutions since 2013, empowers healthcare organizations with proven, enterprise-wide solutions for the secure, compliant, and efficient exchange of clinical information. As a single source technology and service provider for health systems and providers, MRO’s EHR integration, workflow and clinical data solutions improve clinical and financial outcomes requiring extraction and interoperability of medical records, structured and unstructured data. These solutions support enterprise-wide applications, including quality measurement and reporting, payer-provider interoperability, audit and denial management, clinical registries, release of information, and more. Through innovation, emerging technologies, and deep domain expertise, MRO is connecting over 200 EHR and practice management systems, extracting more than 10,200 clinical data elements, and engaging nearly 200,000 providers, securely, efficiently, and compliantly. For more information, visit www.mrocorp.com.
This published piece is provided solely for informational purposes. HFMA does not endorse the published material or warrant or guarantee its accuracy. The statements and opinions by participants are those of the participants and not those of HFMA. References to commercial manufacturers, vendors, products, or services that may appear do not constitute endorsements by HFMA.






