How Orlando Health stemmed healthcare costs by eliminating unnecessary clinical process variation



A six-step initiative by Orlando Health in central Florida to eliminate avoidable variation in healthcare delivery reduced the health system average length of stay (LOS) by roughly 0.75 days, while yielding a corresponding financial benefit of about $1.2 million.
Variation in healthcare delivery is necessary to some extent because of the need to tailor interventions to each patient’s unique circumstances. But it also can reflect inefficiencies in care processes that contribute unnecessarily to the nation’s high costs of care.
Recognizing this reality, in 2017, Orlando Health, a $3.8 billion not-for-profit healthcare system serving central Florida and beyond, embarked on an initiative to eradicate unnecessary variation in care to its patients with the goal of improving quality and outcomes while addressing rising hospital lengths of stay (LOS) and resource utilization. Unnecessary variation was defined as “differences in care provided by different care givers, for patients with the same diagnosis, that increase costs without contributing to better outcomes.” The health system branded the initiative internally as “Right Care.”
Focus for Right Care
The initiative’s goal was to design and implement standard processes, or care pathways, to deliver the most appropriate care to every patient, every time, across Orlando Health facilities. The care pathways aimed to define processes founded in evidence-based medicine wherever possible, and to supplement gaps in evidence-based care with physician consensus on how to deliver high-quality, consistent patient care. The care pathways were designed to be interdisciplinary tools easily accessible for all Orlando Health providers. Although reducing practice variation was the primary goal, pathways were designed to allow for interventions to be tailored to unique patient needs.
The initiative was led by Orlando Health’s vice president of quality and clinical transformations, with a project management team (Right Care team) that included representatives from clinical informatics, clinical transformation and the enterprise data warehouse. Deployment of the care pathways was preceded by two years of groundwork in project planning, communicating with physicians, and organizing and validating necessary databases. The overall initiative encompassed the following six steps.
1. Identify targeted disease states
The initiative’s first phase involved determining which diagnoses would be best to target first for developing care pathways. The Right Care team planned to use these initial diagnoses as a pilot to refine processes for developing and implementing pathways in the future. Based on the time commitment for each diagnosis, and the level of impact desired based on the time and resources invested, the team decided to limit the initial focus to six diagnosis groupings.
The team determined that the most suitable diagnoses to focus on at this stage would be diagnoses that presented the greatest improvement opportunity. To identify where the greatest opportunities lay, the team analyzed key quality indicators based on patients’ discharge diagnoses, looking at discharges from the system’s five acute care hospitals for the prior 12 months of calendar year 2016.
Diagnoses were selected based on the following factors:
- Cases with high actual LOS compared with expected LOS based on the diagnosis’s MS-DRG
- High-volume cases systemwide
- Disease states most capable of being standardized
Based on this review, the team selected the following diagnoses:
- Large and small bowel procedures
- Congestive heart failure
- Sepsis
- Chronic obstructive pulmonary disease (COPD)
- Pneumonia
- Urinary tract infection (UTI)
2. Identify champions and build clinical consensus teams
To lead in creation of the care pathways, the Right Care team identified physician champions who possessed deep clinical expertise and a high degree of influence within the system. The physicians then provided input regarding who should be selected to be members of the focused multidisciplinary teams, called clinical consensus teams (CCTs), that would be charged with creating the pathways.
Although each CCT’s composition was tailored to the particular diagnosis, CCTs typically included the physician champion, key specialist physicians and surgeons, hospitalists, quality officers, nursing staff, case managers, pharmacists and an executive leader. Depending on the nature of the diagnosis, the teams could also include representatives from therapy teams, nutrition, palliative care and various other departments.
To incorporate input from across the system, and increase physician buy-in, participants were purposefully selected from each hospital. Wherever possible, the teams also tried to leverage existing system initiatives focused on a diagnosis to reduce duplicative work.
3. Develop care pathways
Once the CCTs were assembled, the Right Care team scheduled three working sessions with each team to collaboratively establish the process for creating care pathways. The in-person meetings were held in a conference room of the most centrally located and largest hospital in the system.
The rationale and goals for Right Care were introduced during the first of the three working sessions. The Right Care team reviewed with the CCT the benefits of reducing unnecessary variations in care and the reason for selecting the particular diagnosis as an initial area of focus for the project. To highlight the improvement opportunity, analytics were shared summarizing hospital and overall system performance in chief quality indicators for the targeted diagnoses.
Prior to each CCT’s initial meeting, the physician champion identified key articles and resources with the most up-to-date, evidence-based practices for the diagnosis. During the meeting, all attendees received flash drives with these resources and asked to review them prior to the next working session.
The initial meeting concluded with an overview of the structure and benefits of care pathways.
Three to four weeks preceded each of the next two working sessions. These sessions were scheduled for four hours to provide dedicated time for the CCTs to develop, review and finalize their care pathways.
Care pathways were goal-oriented and time-specific based on a patient’s progression in care. Areas of focus varied depending on the diagnosis, but pathways typically accounted for the following:
- Patient education
- Consultations
- Assessment and testing
- Medication
- Dietary recommendations
- Recommendation for patient activity levels
- Discharge criteria
- Post-acute follow-up
Based on key questions and follow-up items discussed during the second session, subgroups of four to six members were deployed to explore ideas and best practices and then return to the third working session to report recommendations to the greater team. Subgroups focused on topics such as pharmacy, lab, patient education, nutrition and anesthesiology.
The third working session served as the platform to finalize and review the care pathway. During this meeting, the subgroups presented their recommendations on key action items, and any incomplete areas from the previous session were addressed. At the end of the meeting, the CCT was given an opportunity to review the final draft of the care pathway and relay feedback to the Right Care team and physician champion.
4. Communicate pathways throughout health system
To help all employees understand the mission and vision of the Right Care initiative, the Right Care team partnered with Orlando Health’s marketing and communications team on developing a comprehensive internal communication strategy and plan.
The goals of the plan were to:
- Inform and educate
- Connect the dots to strategic imperatives and Truven 100 goal[1]
- Obtain buy-in that Right Care is everyone’s responsibility
- Ensure compliance
The communication plan was executed using electronic communications via all existing portals to all audiences, posters on nursing units, presentations to operations and team member councils and online assigned education through an internal platform. The plan helped to gain buy-in prior to the rollout of the pathways and continued to motivate the team throughout the implementation phase.
5. Implement care pathways
Once a care pathway draft was finalized, the physician champion brought the draft to the Orlando Health medical executive meeting for review and approval. Approved pathways then were rolled out at each of the system’s hospitals simultaneously (with the exception of Orlando Health’s children’s hospital), without any intervening pilot program. Leading up to the go-live date, targeted communication plans were deployed to inform physicians of the release, changes to workflows and expectations moving forward.
The Right Care team recognized early that the success of the pathways hinged on willingness of the system’s hospitalists to adopt them, and this was the reason each CCT included a hospitalist. During implementation, the teams conducted regular follow-up meetings with key hospitalists to socialize the pathways and reassure the physicians that their daily workflows would not be significantly impacted.
The Right Care team offered continuous support throughout the rollout to answer questions, collect feedback and quickly address barriers or concerns. Although the benefits of the pathways were clearly communicated, physicians were not formally required to use the pathways for their patients. To encourage adoption, the team developed and distributed tracking tools to demonstrate the benefits in care associated with the pathways.
6. Monitor results
The Right Care team worked closely with members of the system’s enterprise data warehouse to analyze and compare patient outcomes when care pathways were used and when they were not used. The outcomes were aggregated in monthly scorecards at the hospital and system level to monitor successes and identify improvement opportunities.
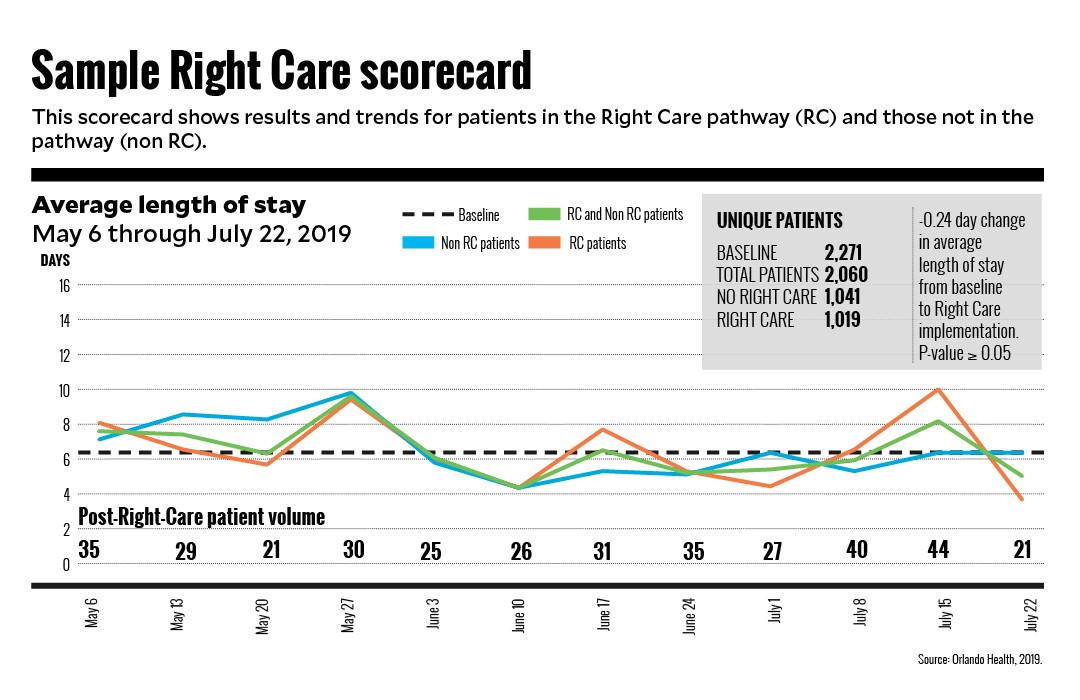
The scorecards tracked key quality metrics for patients who were eligible for a care pathway based on diagnoses and compared results with a baseline time frame prior to Right Care deployment. Results were reported for patients on a pathway compared with patients not on a pathway to illustrate the benefits associated with using the pathway. The key quality indicators included in scorecards were LOS, mortality, complications in care and readmissions.
The Right Care team also worked with the finance department to calculate the financial impact of the improvements in quality. These results were intermittently communicated to the physicians to further validate their efforts but not regularly tracked on the monthly scorecards.
Results and keys to success
Within a year after deploying the care pathways, Orlando Health realized the significant improvements in outcomes for patients with a pathway diagnosis noted at the beginning of this article. The health system attributed this success to strong project planning and execution, continuous communication, internal ownership and effective efforts to build a physician culture of continuous improvement.
Physician leadership, engagement and advocacy was paramount. From the very start, the continual and consistent physician messaging on the importance of clinical standardization and the expected benefits was instrumental in motivating physicians to get on board with the process of developing and utilizing the refined care pathways.
To ensure the pathways would live up to the promise of not substantially changing physicians’ daily workflows, which was deemed critical to success, the Right Care team worked closely with the clinical informatics department to integrate the pathways into preselected order sets in the electronic health record. To encourage hospitalists to use the order set, the team uses the scorecards and other means to show them that the tools would promote higher-quality care, based on the most recent evidence-based medicine, without requiring additional consults or otherwise adding time to their day.
Beyond the quality and financial benefits, the team knew it had achieved success when physicians began to come forward without any prompting, asking to be part of CCT for the next care pathway.
Top 10 clinical variation keys to success
- Physician ownership
- Hospitalist and specialist physician involvement
- Accurate and vetted data with analytical support
- Leadership engagement
- Strong project managers
- Organized communications plans
- Multidisciplinary clinical consensus teams
- Clinical informatics support
- Performance tracking scorecards
- Defined reevaluation structure
[1] Truven Health Analytics is part of IBM Watson Health, which annually recognizes the 100 Top Hospitals in terms of overall performance around quality of patient care, operational efficiency and financial stability. Truven uses publicly reported data, mostly Medicare, to compare hospitals’ performance.





