Why ensuring the appropriate assignment of observation status patients is so important


Brian Pisarsky
Jill Annala-Rogers
Managing observation status requires a focused and consistent effort. Inappropriate assignment of observation status is expensive for patients and hospitals alike and can impede the goal of providing patients with the right care at the right time in the right setting.
Since CMS issued its two-midnight rule for determining observation status in 2013, observation patients have represented a growing percentage of hospitals’ daily censuses. Although the CMS rule technically applies only to traditional Medicare beneficiaries, commercial health plans have adopted similar methods for determining observation status.
We know the percentage of observation-status patients has grown. However, we have not been able to determine what percentage of such patients is appropriate. Starting in February 2022, Kaufman Hall’s National Hospital Flash Report began publishing a new metric that tracks the number of observation patient days as a percentage of total days across the more than 900 hospitals that currently contribute data for the report.
While determining observation status is and should be a decision driven by physician judgment — and the percentage of patients in observation status will vary from hospital to hospital — this new metric will help management understand how much their observation status percentages vary from the median. If that variance is significant, management can investigate and, if appropriate, address the factors or processes that are driving the variance.
The importance of appropriate status assignment
Getting observation status right is important for patients, their providers and the organization:
- For patients, observation status can mean higher copays. and if they need to be discharged to a skilled nursing facility, Medicare coverage of their post-discharge care may be affected.
- For providers, who have a regulatory requirement to inform patients of their observation status and its implications, observation status can create tension in their relationships with patients due to reimbursement or copay implications.
- For hospitals, observation status assignment means a lower payment rate for the care the patient receives. Patients who are inappropriately assigned observation status can also tie up beds in the emergency department or on inpatient units, which can slow patient throughput, interfere with efficient delivery of service, or suggest the need for additional capacity — and the significant capital expenditures that come with it — even if that need may not, in fact, exist.
These are the downsides to observation status, but if managed well and in compliance with CMS guidelines and other payers’ contractual terms, these negative aspects can be minimized.
Under CMS guidelines, observation status should be applied to a well-defined set of specific, clinically appropriate services, including short-term treatments, or when additional time is required to determine whether a patient will need further treatment on an inpatient basis or can be safely discharged from the hospital. If a physician expects that the patient will need a hospital stay crossing two midnights and the medical record supports that expectation, observation status will typically not be appropriate. Even for stays less than two midnights, if the patient is to receive a service on CMS’s inpatient-only list or the physician expects that the patient will require inpatient services, observation status would, again, typically not be appropriate.
If observation status is being appropriately assigned, few observation patients should have a length of stay (LOS) exceeding two midnights. If a significant percentage of observation patients have stays exceeding the two-midnight benchmark, inappropriate assignment may be an issue. The exhibit below, for example, shows data for a hospital at which 47% of the discharges are observation, with 40% of the observation patient stays exceeding two midnights and an average LOS of just under 48 hours. These data suggest that too many patients are being assigned to observation status or that the process for timely discharge of observation patients is flawed, thereby warranting further investigation.
Analysis of observation patient status and length of stay
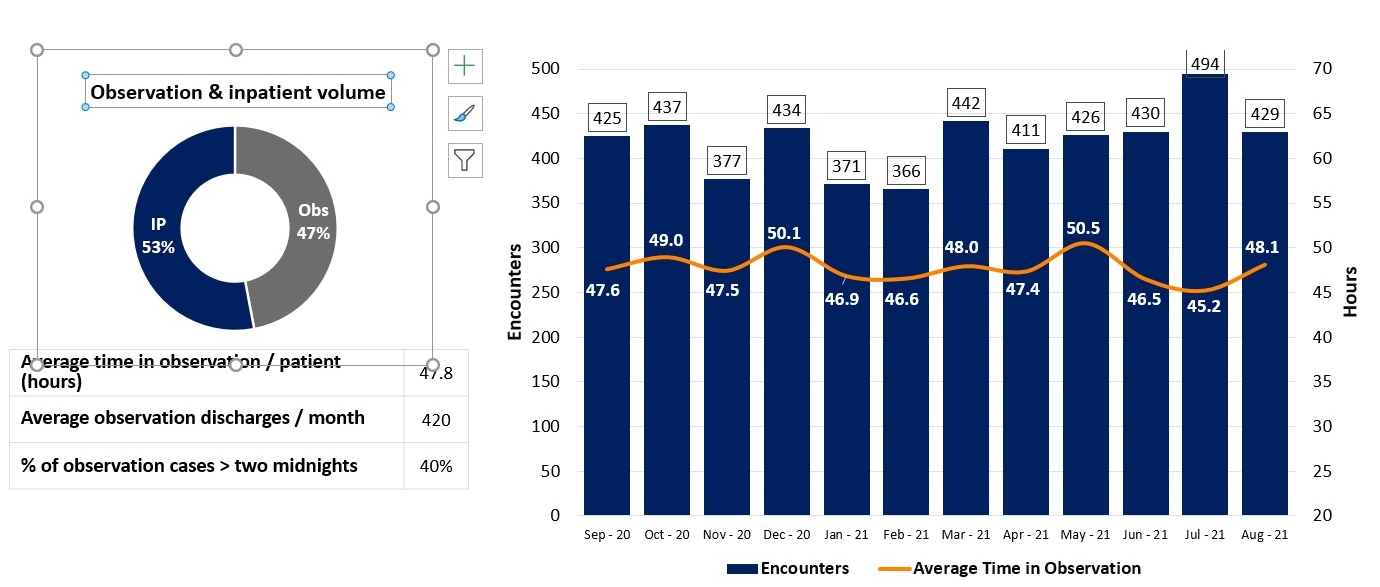
Source: Kaufman, Hall & Associates, LLC, 2021
Tactics to ensure appropriate assignment
To ensure that the status is assigned appropriately, management and clinical leaders can deploy the following tactics.
Protocols. Clearly defined protocols should be developed that establish clear criteria to support individual physician decision-making. The protocols should be both for assigning observation status generally and for determining the appropriateness of observation for conditions where the status is frequently assigned (e.g., atrial fibrillation, chest pain, congestive heart failure, chronic obstructive pulmonary disease and syncope). These protocols also will ensure the medical record includes the detail necessary to respond if a payer challenges an assignment to inpatient status. If a patient’s status changes, the protocols also help determine when reassignment to inpatient status is appropriate.
Observation Status Protocols
Observation status protocols define criteria indicating that observation status would be appropriate (inclusion criteria) or not appropriate (exclusion criteria). For example, criteria for a chest pain protocol might include:
Observation inclusion criteria
- Negative 1st Troponin (
- Chest pain resolves, chest pain intermittent, no EKG changes
- Low (HEART risk score 0 to 3) to moderate risk (HEART risk score 4 to 6)
- Stable vital signs
- No exclusion criteria
Observation exclusion criteria
- Positive troponin (1st draw > 0.011)
- Unresolved ischemic chest pain
- EKG changes (consistent with ischemia or high-risk arrhythmia)
- ECG shows evidence of acute myocardial infarction or ischemia pattern
- High risk (HEART risk score 7 or above)
- Stress test or cardiac imaging needed
- Mental illness (patients at risk of self-harm, suicidal, acutely psychotic, inebriation due to alcohol or drugs)
Observation care management team (OCMT). A dedicated, multidisciplinary OCMT can improve care delivery and throughput for observation patients and enhance communications with patients and their families. OCMTs ensure compliance with protocols, identify and resolve any barriers to treatment or discharge of observation patients, and manage and facilitate expectations and education for patients and family members. Key capabilities represented on the team include clinical care, case management and utilization management, as shown in the exhibit below. OCMTs conduct regular rounds of observation patients throughout the day at regular intervals (e.g., every four to six hours) to monitor and update the status of these patients.
An observation care management team
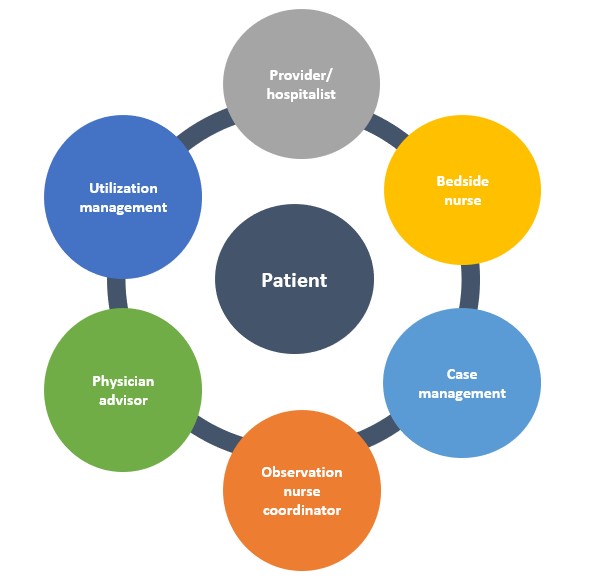
Source: Kaufman, Hall & Associates, LLC, 2021
Dedicated observation units. A dedicated unit for observation patients serves several purposes:
- It allows emergency and inpatient units to optimize the use of their space for patients who need higher acuity services.
- It enables dedicated observation unit staff, such as an OCMT, to focus their care on the specific needs of observation patients.
- It helps patients and their families understand that observation is a standard form of patient status and that the patient is receiving an appropriate level of care for that status along with the other observation patients on the unit.
Contract review. As noted above, commercial health plans have followed CMS’s lead and are closely monitoring assignment of patient status. Commercial health plans may or may not use CMS’s two-midnight rule. In any event, contracts should be reviewed to ensure that the criteria for determining observation status are clearly defined. If they are not, the hospital should negotiate these terms with the health plan and update the contract.
Community partnerships. The COVID-19 pandemic has focused even more attention on inequities in our healthcare system, many of which are driven by social determinants of health that disproportionately affect underprivileged populations. Patients may be held in observation status simply because there is not a safe or supportive environment to which they can be discharged. Partnerships with community organizations that can help improve the patient’s home environment or support the patient at home can make timely discharge a safe and viable option.
With new data that enables enhanced benchmarking of observation status, hospital leaders can obtain a significant opportunity to better identify issues with observation status assignment in their organization and apply the resources needed to address these issues quickly and effectively..






