Administration finalizes requirement for hospitals to post rates paid by health plans
The Trump administration requires hospitals to post online the rates they negotiate with health plans, as well as rates for 300 “shoppable services,” by 2021.
The Nov. 15 final rule from the Centers for Medicare & Medicaid Services (CMS), which prompted one hospital advocate to immediately promise to file a lawsuit, requires hospitals to post online all their standard charges (including gross charges, payer-specific negotiated charges, de-identified minimum and maximum negotiated charges and discounted cash prices) for all items and services in a single digital file and in a machine-readable format.
Hospitals also must post online their standard charges for at least 300 “shoppable services” (that is, 70 CMS-specified and 230 hospital-selected services) that the hospital provides. This information must be made available in a consumer‑friendly manner. The posted rates must include charges for services that the hospital customarily provides in conjunction with a primary service that is identified by a common billing code.
CMS will deem a hospital compliant with the new requirements if the hospital maintains an Internet-based price estimator tool that meets specified requirements, including real- time estimates for consumers on their costs for a shoppable service offered by the hospital.
Failure to comply with the requirements could lead CMS to impose fines of up $300 per day (totaling $109,500 annually) and to publicize a hospital’s lack of compliance on its website.
The following are details of price posting requirements:
- Describe each item or service
- Display prominently and clearly, and identify the hospital location
- Ensure the data is easily accessible, without barriers, is free and does not require an account or password or a user to submit personal information
- Update the data at least annually
Definition of standard charges
CMS is finalizing the definition of standard charges to include the following 5 elements:
- Gross charge. The charge for an individual item or service that is reflected on a hospital’s chargemaster, absent any discounts
- Discounted cash price. The charge that applies to an individual who pays cash, or cash equivalent, for a hospital item or service
- Payer-specific negotiated charge. The charge that a hospital has negotiated with a third-party payer for an item or service
- De-identified minimum negotiated charge. The lowest charge that a hospital has negotiated with all third-party payers for an item or service
- De-identified maximum negotiated charge. The highest charge that a hospital has negotiated with all third-party payers for an item or service
Source: CMS, “CY 2020 Hospital Outpatient Prospective Payment System (OPPS) Policy Changes: Hospital Price Transparency Requirements (CMS-1717-F2),” Nov. 19, 2019.
Congress is still expected to pass a surprise bill measure this year


Two leading Senate proponents, Senators Maggie Hassan (D-N.H.) and Bill Cassidy (R-La.), and a spectrum of healthcare policy advisers are expressing optimism that Congress is likely to pass legislation this year to bar surprise healthcare bills.
Several bills have relied on a rate-setting approach advocated by health plans, which has drawn congressional support because it would provide the biggest federal savings — through reduced subsidies to Affordable Care Act marketplace plans — which in turn could be used to fund other healthcare legislative priorities.
Some members of Congress are urging use of an arbitration system in which an arbitrator decides disputed rates using guidance from legislators, such as the approach used under New York state law.
Ongoing negotiations have sought a compromise that would entail replacing the arbitration benchmark used in New York — 80% of billed charges, which critics say fuels spending increases — with existing in-network rates.
Separate legislation that aims to cut drug prices is seen as less likely to pass Congress in 2019.
M&A trend: More acquisitions of small or ‘distressed’ hospitals
Hospital acquisitions ticked up in the third quarter of the year, and smaller or “distressed” hospitals increasingly were targets, according to tracking firms.
Hospital merger-and-acquisition (M&A) activity accelerated in the latest quarter, which returned the overall volume of deals in 2019 to that seen in previous years, according to several tracking firms.
Hospital deal volume reports differed based on the methodology used by different firms, but reported year-to-date total deals included:
- • 61 announced transactions versus 68 at this point in 2018 (Hammond Hanlon Camp LLC)
- • 71 announced transactions versus 68 at this point in 2018 (Kaufman Hall)
- • 62 transactions versus 92 at this point in 2018 (Ponder and Co.)
- • 70 definitive-agreement-stage or closed transactions versus 61 at this point in 2018 (Irving Levin Associates)
A recent trend has been the increasing number of deals involving financially “distressed” hospitals, analysts said.
Irving Levin found that deals involving hospitals with net income losses increased 30% from this point in 2018 to total 16 of the deals thus far in 2019.
“There’s still distressed activity happening throughout the market, but in this quarter, this year, it’s been greater than before,” Mike Tierney a director for Hammond Hanlon Camp LLC (H2C), said. “You’re seeing hospital systems that are finding ways to operate the assets they operate well, and then those that don’t do a good job, finding new homes for them.”
One health system finds ‘millions’ of reasons to audit value-based payments
Ochsner Health System in Louisiana used audits to learn that health plans with which it had entered value-based payment contracts had underpaid on those contracts by “millions” of dollars.
Ochsner took the unusual step of auditing bonus payments it received under the first two upside-only value-based payment (VBP) models it pursued with commercial health plans.
“In both cases, the audits led to multi-million-dollar adjustments” for the health system,” said David Carmouche, MD, senior vice president of community care for Ochsner. “So that doesn’t give you a lot of trust when you’re trying to enter into a collaborative relationship.”
The health system undertook the audits because Carmouche, as a former health plan executive, understood the challenge that health plans face in interpreting complex new VBP models.
White House healthcare leader expresses skepticism of mandatory models
When asked about whether the administration will accelerate the push toward value-based payment, Joseph Grogan, JD, assistant to the president and director of the Trump administration’s Domestic Policy Council, said he was “skeptical” about any program that required participation by either providers or beneficiaries.
“We need to make sure that patients and physicians have the flexibility they need to make the healthcare choice that’s going to make the patient healthier,” Grogan said. “We’re about the patient being in control and the patient being at the center of this, so any time we’re talking about forcing arrangements, it’s something we would be very skeptical about.”
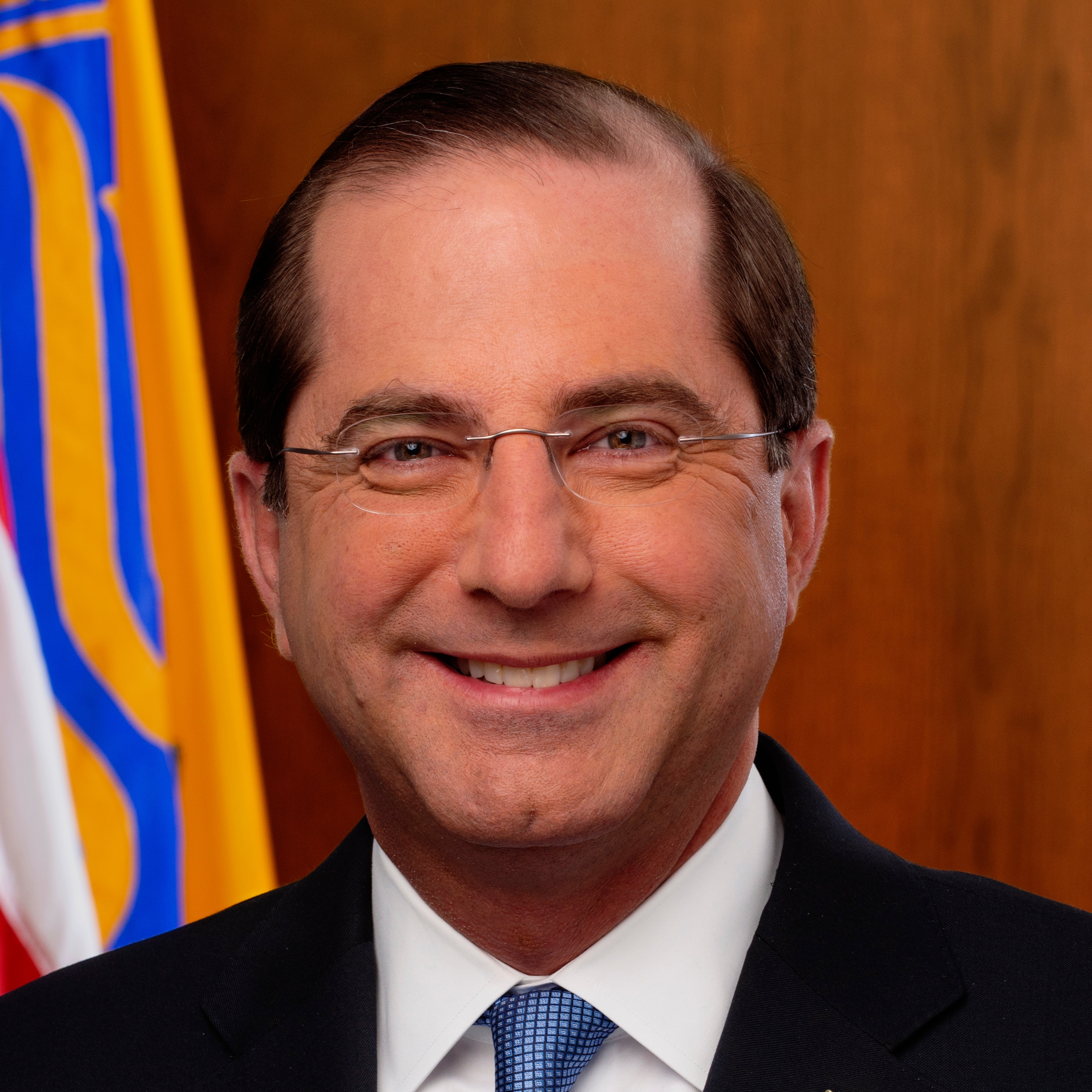

Alex Azar, secretary of the Department of Health and Human Services (HHS), and Seema Verma, administrator of the Centers for Medicare & Medicaid Services (CMS), have promised increased use of mandatory payment models, which often draw provider criticism.
“Looking forward, you can expect that some of the models we have under development will be mandatory,” Verma said. “One reason for mandatory models is that selection effects can be significant in voluntary models.” Grogan’s skepticism toward mandatory models is significant because — as he made clear — his policymaking position in this administration outranks that of any officials at HHS or CMS.





