How to determine appropriate patient status and navigate observation-level care
The financial implications of ensuring appropriate patient status throughout a hospital stay are substantial, so it is in organizations’ interest to enhance the process.
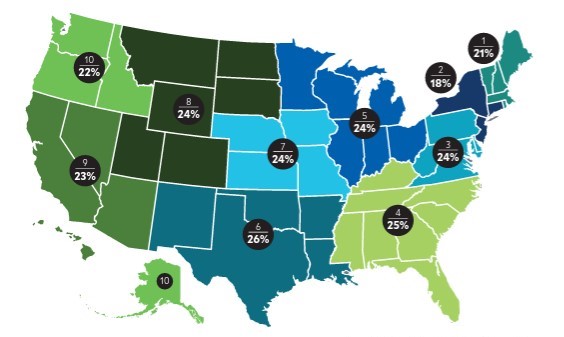
Challenged by the status determination process, many hospitals often inappropriately admit patients into observation or inpatient status. The nature of the challenge is illustrated in the exhibit below, which shows that observation rates among different CMS regions vary by as many as 8 percentage points.
Fee-for-service Medicare observation rates by CMS
Choosing the most appropriate designation is vital to ensure high-quality patient care is delivered and that financial reimbursement is appropriate for services rendered. To augment net patient revenue while prioritizing patient outcomes, hospitals and health systems should consider whether they need to improve their processes for determining patient status.
Financial implications of status determinations
Appropriate care delivery and optimal patient outcomes are the primary priorities, which can be achieved irrespective of status. Nevertheless, the ability to determine appropriate patient status and level of care has significant implications for payment.
Payer reimbursement typically differs between observation and inpatient status. While the nuances of agreements may vary across payers and facilities, reimbursement for observation discharges often is lower than for inpatient care.
Consider a standard inpatient case that may be reimbursed at about $6,500, based on CMS regulations, compared with $2,000 for a standard observation discharge. In this example, there is a $4,500 variance for a case that might have received the exact same care but was discharged with an inappropriate status. This variance is similarly prevalent with other payers, meaning documentation of medical necessity and deliberate processes for status determination can have a significant impact on net patient revenue.
On the other hand, while inpatient status potentially generates more revenue, the payer might deny that revenue and revert payment to observation status if the patient does not meet criteria for inpatient status.
Appropriate status determination and discharge status can also have significant financial consequences for the patient. A discharge from observation status may result in a higher out-of-pocket expense compared with an inpatient discharge if not performed in the most fiscally appropriate and time-dependent manner. Since observation status is an outpatient service, a Medicare patient pays 20% of billed charges as coinsurance.
However, a well-run and fiscally responsible observation stay can result in out-of-pocket expenses not unlike a daily deductible for an inpatient stay. Such an outcome depends on determining appropriate status, minimizing unnecessary testing and treatment, and expediting discharge or, if necessary, transition to inpatient status.
Best practices for observation management
Implementing the following approaches can help hospitals and health systems align care delivery and revenue cycle functions, ensuring patients are in the right status and receiving the appropriate level of care throughout their hospital stay.
Care team collaboration. Collaboration and communication among the care team members (physicians, utilization management staff and nursing staff) are critical to a successful observation management program. Keys include deliberate discussions between care teams regarding patient needs and plans of care, as well as documentation within the medical record that clearly substantiates medical necessity (see the sidebar “Observation status hinges on medical necessity” below).
A dedicated huddle to focus on observation patients also enables communication and collaboration. This huddle serves as a forum for case management, utilization management and physician advisers to review all observation patients at least once a day. It also provides an effective means for highlighting barriers to discharge, necessary follow-up actions and status conversion potential.
Status determination at the portal of entry. Determining status appropriately in the emergency department (ED) reduces the potential need for a conversion to inpatient status later in the stay and helps place the patient in the proper care setting.
In facilities with leading patient-status processes, case management or utilization management staff in the ED assume ownership of the initial status determination process. These staff are integrated into a collaborative process between ED clinicians and hospitalists that focuses on effective communication, accurate initial medical necessity reviews and timely provider documentation of patient needs and acuity.
Integration of physician advisers. A sophisticated program utilizes physician advisers as engagement liaisons between case management, utilization management, clinicians and administration. Advisers can aid in status determinations through secondary reviews of observation cases and can assist the utilization management team and physicians throughout the process. Advisers may also be involved in additional processes, including payer appeals, denials management, and education for clinicians and other quality improvement efforts.
Utilization of observation units. Dedicating provider staffing models to observation medicine ensures appropriate status designation and improves outcomes for this patient population. Much has been published on ways to implement observation-status designation, but all data point to the superiority of dedicating physician, nursing and ancillary staff to the process of observation medicine and the creation of dedicated units.
Devoting space and staffing to observation status allows the focus to remain on one type of patient and one type of medicine. Though the patients and their conditions can vary, the types of patients and conditions do not.
This uniformity allows for creation of protocols for conditions that historically tend to meet observation criteria, fitting nicely into a standardized approach. It limits variation in the general pathways for workup and treatment of these conditions, creating efficiency and, in turn, cost containment. That’s especially key for observation stays because reimbursement tends to be significantly less per patient encounter compared with inpatient status.
Dedicated observation units repeatedly have shown far superior metrics regarding length of stay and cost to the facility compared with patients in observation status who are not in a dedicated unit. Working to ensure most if not all appropriate observation patients fall under the purview of staff on dedicated units becomes a matter of not only clinical but also financial importance.
Patient outcomes are improved through the use of protocols for specific diagnoses that are tailored to short-stay observation medicine. Such protocols can eliminate unnecessary testing and potentially unwarranted treatments that could prolong the patient’s hospital stay at least and result in patient harm at worst.
Dedicated staff who consistently adhere to the same process better understand the expectations and can deliver a higher quality of care, resulting in higher patient satisfaction scores, improved clinical outcomes and, invariably, cost savings.
These savings can be seen in two distinct forms:
- On a per patient basis from the efficient workup and expedited treatment of a patient in a dedicated observation unit, specifically through less testing, consultation and patient time spent in the facility
- In reduced bed hours in the facility, thus opening beds for higher-revenue-generating patients
An urgent priority
Appropriate status determination is a nuanced process that has significant implications for patient care and reimbursement. Fortunately, the steps needed to improve this process are well within reach for hospitals.
Observation status hinges on medical necessity
Observation status is an outpatient designation that allows providers to place a patient in an acute care setting to monitor the need for an inpatient admission and diagnose and treat disease pathologies that may respond or improve quickly. Common signs and symptoms including chest pain, shortness of breath, nausea/vomiting/stomach pain and fever might result in patients being placed in observation for further testing.
Patients who have been appropriately assigned to observation status typically have much lower acuity and severity of illness compared with patients receiving inpatient care and are commonly discharged from the facility within 24 to 36 hours.
A bedded observation patient can be appropriately converted to inpatient status if needed. Medical necessity, the principle defined by CMS and other payers, establishes the distinction between observation and inpatient levels of care.
Medical necessity is documented within the medical record and should clearly and precisely illustrate the complexity of medical factors and the reasoning for the required inpatient admission. Inadequate documentation can result in payer denial of inpatient authorization and refusal of payment for services delivered.
Examples of how medical necessity can support an inpatient admission
Appropriate for observation status
- Patient complaint of shortness of breath
- Abnormal labs
- Vital signs stable
- Will need to monitor
- Consult with nephrology and cardiology
Appropriate for inpatient status
- Patient complaint of shortness of breath with imaging findings of new onset of congestive heart failure
- Lasix 80 mg IV given
- Oxygen saturation 87% on room air, improved to 100% once on 4L of O2
- Abnormal renal function, consider acute kidney injury
- Will need cardiology and nephrology consulted
- Patient appropriate for inpatient level of care, anticipate 2-midnight stay
Importance of physician documentation for patient statys
Appropriate documentation in the medical record has been a mainstay of coding and billing, and more recently the basis for determining patient status as well.
Both physicians and utilization management staff can make the best upfront determinations regarding whether a patient would be best suited for observation or inpatient status. Each patient should be viewed in totality as opposed to simply on the basis of one problem at a time. It is hence vital that as much appropriate and useful information as possible be entered into the medical record up front.
All staff — including providers and utilization management, coding and billing — must understand the various components to documentation:
- Appropriate chief complaint
- Supporting diagnoses
- Acknowledgment of physical examination
- Historical and workup findings (e.g., lab, imaging)
- Assessments of patients
- Plans for treatment and/or further workup
Documentation should support medical necessity. All who review the medical record must fully understand the primary and secondary diagnoses, the recommended treatment and additional workup, the overall level of concern for the patient, risk factors that make the patient more complex, and the patient’s anticipated trajectory during the hospitalization.
The need for comprehensive, precise documentation
The clinician must offer as many potential diagnoses as possible to support better understanding of the presented chief complaint. This list should contain all acute pathologies, including new acute conditions and chronic conditions.
Additionally, any significant comorbid disease that could factor into the level of complexity or affect the patient’s hospital stay should be mentioned in the medical record to support documentation indicating the trajectory could be longer or more complex than the presenting acute condition suggests.
Equally important is highlighting abnormal lab, imaging and vital-sign findings. If a patient has vital-sign abnormalities such as transient hypoxia, tachycardia or tachypnea, but no such acknowledgment is in the record, anyone reviewing the chart (including other clinicians) would be unable to make a fair determination about the patient’s stability or potential hospital course. Such information can be the difference between inpatient and observation status. More important, a lack of information can prevent other clinicians from efficiently ascertaining a patient’s acuity.
Why the impetus is on clinicians
It can be difficult for non-clinicians to recognize whether patients have the potential to get sicker more quickly and thus require a higher degree of services and more time in the hospital. Therefore, it is important for trained clinicians to make this distinction. This step can have important consequences for status determination.
Consider young, otherwise healthy patients with no comorbid disease who present with pneumonia. Clinicians know that in most cases, those patients very well might not need hospitalization. However, any such patients who have significant comorbid disease are at considerable risk for both failed outpatient treatment and longer hospital stays. Properly relaying the potential for higher-level needs can be the difference between observation versus inpatient status.





