Value-Based Employee Compensation in an Inpatient Rehabilitation Facility
Evaluating employees based on the quality of care they provide can help encourage direct contribution to a healthcare organization’s strategic goals.
The rising cost of health care, coupled with the need for better business analytic tools and support applications, has shone a light on a serious gap in hospital efficiency. Until now, the solution for hospitals to continue to grow profits was to expand, build more beds, and hire more workers. Little attention was paid to innovation of operations, efficiency of the new facilities, or the evaluation of the skill of the workers that were being hired. The main focus over the past decade was solely on accommodating the massive growing patient population. Today, however, healthcare organizations must begin to employ strategies for increasing efficiency if they are to stay financially viable.
Gap Analysis
First, hospitals and health systems should begin to treat human capital expenditures as thoroughly and as rigorously as equipment capital equipment expenditures. The most significant capital cost in health care (as is the case with any service industry) comes from labor, but hiring decisions are often made by single managers with little training on hiring and little vetting. Decisions may be based on intangible factors such as team fit and likability of the candidate. Hiring based on these soft factors presents a massive gap in the healthcare industry relative to the efficiency of their capital dollars expended on labor.
Another major point of emphasis in healthcare hiring is the experience level of workers. Health systems often expend significantly higher capital dollars for workers with adequate experience. There is a common misconception that experience is valuable in and of itself; however, experience alone offers no value to a healthcare facility. In reality, expending more capital dollars at an increasing rate for experience ensures a decreasing ROI for staffing. For example, consider a physical therapist (PT). A new graduate PT may command an annual salary of $70,000, compared with $85,000 for an experienced PT. If both PTs have the same performance standards, and both exactly meet them, the new grad PT offers more tangible value to the company than the experienced PT.
When a staff member’s performance plateaus after a certain amount of experience, yet his or her salary continues to grow, the ROI on that particular staff member begins to decrease, hurting the organization’s bottom line. Evaluation of an employee’s performance is often subjective and based on manager reviews. The value the employee produces and contributes to the company is not necessarily correlated to the salary or pay increases that may occur from year to year. In addition, companies are handicapped by an all-or-none approach—they must continue to invest the same amount in an employee, or fire the employee. There is little flexibility to pay solely on the value the employee produces.
In addition to these concerns, most organizations lack an objective means to assess employee value, relying instead on managers’ subjective assessments of employees’ contributions. Managers can tell you who their best employees are, but they often cannot give an objective analysis why or offer an objective, value-based justification for how much more those employees deserve than the lower performers.
To improve efficiency, instead of allowing experience to dictate pay levels, healthcare organizations should adopt an approach in which employees are paid according to the measured value they provide. Going forward, the most successful companies will define value within a job code measuring the extent to which the worker contributes to the company’s strategic goals, and then design a system of value-based human capital expenditure with a pay structure based on the value each worker is capable of producing. The purpose of such a system would be to avoid a decreasing ROI on human capital acquisitions, thereby drastically reducing wasted labor costs and maximizing labor efficiency costs year-over-year.
Potential Solutions
In adopting such a compensation system, hospitals must embrace an analytical approach to how expenditures are used. Hospital and health systems must rely on business analytics rather than employee experience level or seniority to determine how much to invest in employees. These organizations should establish objective, analytical rewards packages that renew regularly to prevent diminishing returns on high-cost human capital. The company should evaluate its own ROI related to the employee on a regular basis, just as it evaluates ROI related to capital equipment purchases. The company’s return should correlate directly with employee rewards.
To quantify the appropriate value in terms of investment in human capital, the value of each employee must be represented via statistical analysis. A value-above-replacement (VAR) analysis should be implemented specific to each major job code within the hospital. The VAR analysis should be directly related to the company’s strategic goals as well as the bottom line.
An individualized VAR for each employee should be used to determine yearly or even quarterly bonuses above a lower base salary. Quarterly would be optimal for performance, but that timing also would be labor-intensive from a payroll and human resources perspective. The VAR can be positive, neutral (essentially zero), or negative.
If an employee’s VAR is positive, the employee is producing tangible value above what could reasonably be expected if the employee were replaced by an individual whose performance reflects the average market value an organization could expect related to the job code. The higher the VAR above zero, the more the employee will earn. If the VAR is neutral, or near zero, the employee is producing no more and no less than what a reasonable replacement could produce, and should not earn above market value regardless of experience level, or seniority. If the VAR is negative, the value of the employee is less than typical, and the employee should not be retained if subsequent review periods consistently indicate negative VARs. If used accordingly, the VAR would facilitate selective turnover and reward positive performance thereby overall boosting the company’s performance.
VAR Application and Benefits
Following is an example of an in-depth VAR assessment focusing on physical therapists in an inpatient rehabilitation facility (IRF) setting. This model could be applied to other settings and positions with some adjustments based on job duties and responsibilities. To fully represent the total value of an individual employee, it first must be determined how that employee (in this case a physical therapist) is capable of contributing to achievement of the company’s strategy. Not every job role will be applicable to every strategic goal. For example, a staff physical therapist in the IRF setting is not directly capable of contributing to facility volume growth or expansion. A physical therapist VAR in the IRF setting would include the following components.
Productivity. This measure is defined as therapy units produced/hours worked. A therapist who can see more patients (thereby generating more revenue) than an identified average within a set time frame would, by definition, be more valuable to a company. Judging performance on this basis alone might raise a concern about fairness, because one could argue that some patients simply demand more time, and at any given time, one therapist may be required to treat more patients who need more time and attention. To mitigate that concern, management should strive to keep uniformity and fairness across employee caseload assignments. Obviously productivity alone cannot gauge the full scope of employee performance; therefore, additional factors must also be considered to account for quality, safety, etc.
Cancellation rate. Defined as the amount of scheduled therapy units that were scheduled yet not completed. Scheduled time that is missed could be the result of therapist cancellation, patient cancellation, or cancellations due to medical concern. Immediate medical factors are not always directly controllable to the employee; however, over the course of quarterly or yearly reviews, true differences will emerge and therapists who consistently show the scheduling flexibility to recapture missed time will perform better. In addition, cancellation rate is an indirect measure of patient satisfaction. Employees who provide excellent patient experience consistently show a lower cancellation rate and should be rewarded. Therapists with a lower cancellation rate contribute to the efficiency of the company by reducing the costs of rework needed for rescheduling patient appointments and rearranging schedules.
Patient experience. All service companies including hospitals strive for high customer satisfaction. The satisfaction related to specific employees should be included in any VAR. Most often, hospital systems manage patient satisfaction via third party vendors for reliability and objectivity which can be included.
Fall rate. In the IRF setting, falls must be minimized. Falls lead to injuries, unnecessary tests such as x-rays, and MRIs, and overall increased costs. Any therapist who consistently has a higher-than-average incidence of patient falls will have a negatively impacted VAR.
Percentage of patients discharged home. IRFs are evaluated based on the percentage of patients who are discharged directly back to home as opposed to requiring continued care (at a higher cost) at a nursing home. Therapists who are more creative in tailoring their treatments toward directing their patients home will benefit the facility.
Length of stay (LOS) efficiency. The LOS of an IRF is determined by the functional gain of the patient divided by the amount of days the patient was in the IRF. Functional gain is determined by the functional independence measure (FIM). The FIM is a comprehensive standardized assessment of the patient’s function at any given time and is typically scored at admission and again at discharge to indicate the amount of functional progress. The formula is simply to divide LOS by FIM. Each therapist should be held accountable for the amount of functional improvement they are able to achieve with their patients per day.
The VAR Calculation
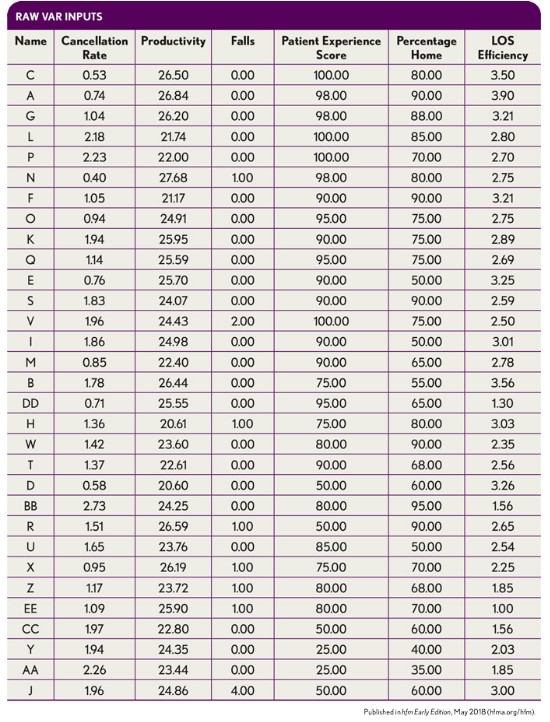
The VAR is calculated from a weighted average of the above components. The individual weighting of components should be determined by management in accordance with the company’s strategic goals. The exhibit below shows the raw inputs necessary for the VAR equation for 31 hypothetical therapists in an IRF department.
Once the raw inputs are acquired and recorded as shown, they must be normalized into a usable and comparable form so they can be appropriately weighted. The way to normalize each input relative to the others is by ranking each employee in each category. The exhibit below shows the employee rankings for five of the inputs, with falls being the exception.
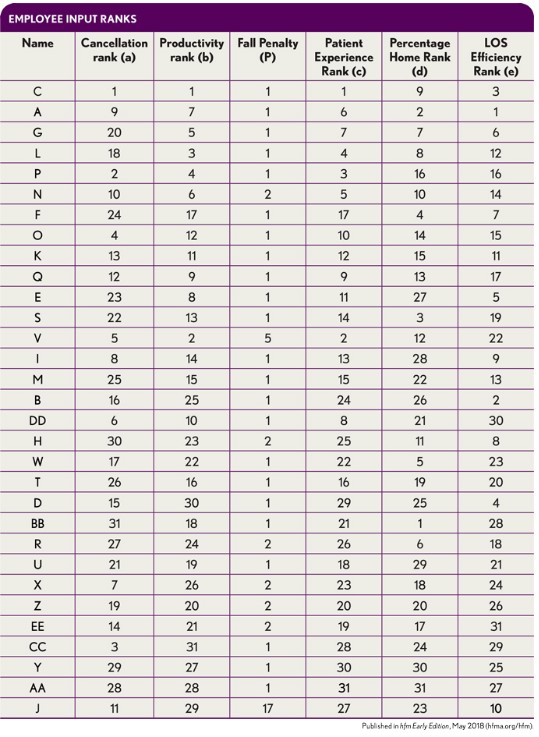
For this VAR, rather than involving rankings, the falls input is factored into the overall score differently. Because each individual fall has significant tangible dollars of added costs, any patient falls that occur under a therapist’s care are amplified and added to the final VAR in the form a penalty. Specifically, the fall penalty is calculated as follows:
1 + (falls)^2
This approach can have profound effect when a single therapist is allowing multiple falls. The minimum score a therapist can receive, and not incur a penalty, is 1, reflecting no patient falls. With a single fall, a therapist’s score increases to 2. And with each additional fall, the score (or penalty) increases exponentially. Hence, as shown in the first exhibit above, therapist J has allowed four falls, leading to the exponentially higher fall penalty of 17, as shown in the second exhibit above.
It is at this point that the VAR can begin take form. First, management needs to assign appropriate weights to each input to calculate an initial therapist composite score. Accurate weighting of the inputs is crucial and should correlate directly to the company’s overall strategy. For the IRF example, the weighting is set as follows:
- Cancellation rate: 10 percent
- Patient experience: 20 percent
- Productivity: 20 percent
- Discharge home: 20 percent
- LOS efficiency: 30 percent
Once a composite score is calculated with the weighting system, the fall penalty will be added directly to it.
Composite Score = (0.1a + .02b + 0.2c + 0.2d + 0.3e) + P
For the composite score, lower is better, as it is the average of the employee ranks. Therefore, adding raw points via the fall penalty will be detrimental to the final composite score. Once the final composite score is formed, the “replacement value” will be set equal to the 25th percentile. Once the 25th percentile score is determined, each individual composite score will be subtracted from the 25th percentile score to reveal the individual VAR:
VAR = (25th percentile composite score) – (individual composite score)
The table below shows the composite score and subsequent VAR.
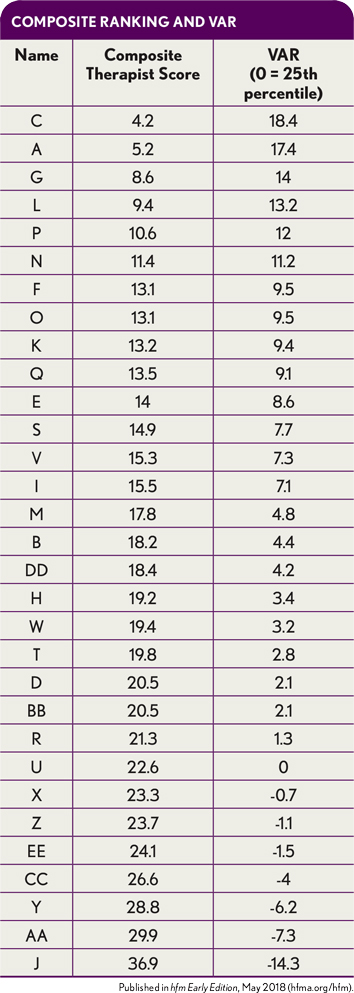
In this example, simple calculations can determine that the 25th percentile of overall performance is equal to 22.6. At the 25th percentile, the VAR should be set to zero, with the idea that any employee whose score is worse (indicated by a negative number) can likely be outperformed by a replacement. Essentially, the 25th percentile of performance level is equal to the expected replacement value that can be acquired in a new hire.
Based on the VAR rankings, therapist C is the highest performer and should be paid the most in the review period that was evaluated. Conversely, therapist J was the lowest performer. Therapist J’s VAR was drastically reduced due to allowing the most falls. If therapist J had allowed zero falls for the review period, the VAR would have remained positive; instead, it dropped to -14.3.
It makes sense that increased falls would have a substantial negative impact on an employee’s VAR and ultimately the amount of capital invested in the employee because each fall leads to increasing costs for the company. By using VAR, the company would not incur a loss by overly investing in the employee without regard for the employee’s negative financial impact.
Benefits of VAR Analytics
The previously mentioned example of an IRF’s ability to recover unnecessary costs related to excessive falls with a therapist is one of several benefits of using VAR analytics. VAR can be applied to virtually any job code that has several workers with the same expectations. A VAR system could easily be designed for a registered nurse using inputs such as productivity (number of patients cared for/hours), patient experience score, infection rates, fall rates, and medicine administration error rate. VAR systems also could be applied for case managers, with inputs for factors such as raw LOS, and durability of outcomes (hospital readmission rates).
VAR analytics also help ensure a positive ROI on human capital expenditures. The “margin,” so to speak, on an employee is always preserved by the nature of the statistic. Traditional systems pay only for experience and seniority, without attempting to provide an accurate measure of the employee’s true value or production ability. VAR eliminates wasted capital dollars on high-salaried, low-performing employees.
In addition to the clear tangible benefits, VAR offers several intangible benefits. VAR facilitates selective turnover. Employees who are not highly motivated and produce little, relative to others, will not have their behaviors reinforced by a static salary and be inclined to leave the organization. Thus, the use of VAR not only can help the company avoid losses, but also can facilitate the removal of low performers altogether.
The use of VAR also should attract high performers from all spectrums of the experience/seniority continuum. Potentially the greatest benefit of VAR is that it provides a direct link between the company strategy and the front-line worker. Often, front-line workers feel far removed from the company’s top management and strategy makers. With a properly aligned VAR, the front-line staff directly impact and enjoy company success.
Disadvantages of VAR Analytics
VAR analytics does have limitations. VAR is very individualized and accounts only for individual contributions to the company’s strategic initiatives. What it fails to recognize is the contributions team members may have to each other. For example, consider a new employee hired directly out of school with no experience. An experienced team member who helps new employees to raise their performance receives no individual benefit in return via his or her own VAR, even though the company receives additional value. In fact, the helpful team member may even be undermining his or her own VAR, because the scores are relative. Individual competition within the same team could potentially hinder overall progress in certain scenarios.
One of VAR’s most obvious strengths is objectivity and fairness amongst employees. The disadvantage associated with its fairness is that not every employee will be placed under the same circumstances every time but will be evaluated as if they were. For example, in a given period one employee may randomly draw a substantially higher fall risk patient and have a subsequent negative impact by no fault of their own. This phenomenon is short-term in nature and in theory would be mathematically corrected over time. By shortening the review cycles to quarterly, certain high risk or unfair situations would be mitigated by not lingering on and continuing to impact employee scores negatively.
VAR also disregards employee engagement and satisfaction. VAR’s nature is capitalistic and assumes that employees want to earn more money; however, that is not always the case. Some employees perform better in a more supportive and less competitive environment. This could be countered by incorporating an employee satisfaction component into the VAR of management.
An interesting potential flaw of VAR that applies mostly to smaller teams is that it may encourage the formation of employee cartels. In theory, employees could form cartels and agree to alter their own performance to maximize VAR returns to their own pay.
Arguably the most significant intrinsic flaw to VAR is in its effect over the long term. VAR scores assume that the employee at the top of the bottom performance quartile represents the replacement value. However, over time, if VAR takes hold and performance improves within a company, the statistic becomes skewed, so the lower quartile VAR within a company might actually be higher than the real VAR in the market. When a company’s VAR becomes positively skewed, the company’s average performance becomes superior to the market average; in this instance, the company runs the risk of replacing its own relative low-performers with even lower performers from the market.
In addition to its intrinsic limitations, VAR may difficult to implement in some labor markets because of extrinsic factors. For example, organized labor unions may resist implementation of such performance standards. In such markets, healthcare systems would need to ensure that the total compensation pool is not changed but is redistributed, with more compensation directed toward higher performance to improve the company’s overall financial viability. If VAR-based compensation is implemented correctly with full alignment to the facility’s financial goals, it might be feasible to increase total compensation pools in direct correlation with the company’s margins, thereby making VAR more attractive to labor unions.
Healthcare costs have continued to skyrocket out of control, largely in part because of the hospital industry’s inability to effectively develop analytical tools to assist with decision making in unison with the expanding patient population. As with any service company, the most significant operational cost in a healthcare organization is labor. Historically, hospital systems have paid little attention to the ROI they gain from their labor expenditures, instead directing labor dollars toward traditional components such as seniority or experience.
To improve the efficiency of operations and recoup wasted human capital expenditures, hospital systems should establish analytical support tools to help determine how much to invest in each employee based on that employee’s actual contribution to the organization. Designing a unique VAR for each job code and a rewards system based on quarterly or yearly VAR performance numbers may be the best option available to them.





