How a dashboard and an 8-step process helped a hospital slash drug costs
Using an innovative dashboard and change management principles, an academic medical center was able to persuade its anesthesia providers to switch from a high-cost anesthesia drug to an equally effective, lowercost alternative, substantially reducing its cost for anesthesia care.
Runaway increases in pharmaceutical costs are a major contributor to rising overall costs of care that threaten the ability of U.S. hospitals and health systems to maintain positive operating margins (see sidebar). Like many of its peers, the Penn-Presbyterian Medical Center (PPMC) of the University of Pennsylvania Health System in Philadelphia recognized the need for an aggressive strategy to reduce its pharmaceutical spend.
The medical center — one of six major medical centers in Pennsylvania and New Jersey that along with multiple outpatient centers, make up the larger health system — decided to tackle the challenge by focusing initially on reducing costs for anesthesia medications, which are among the costliest medications used in hospitals.
The tool: an anesthesia dashboard
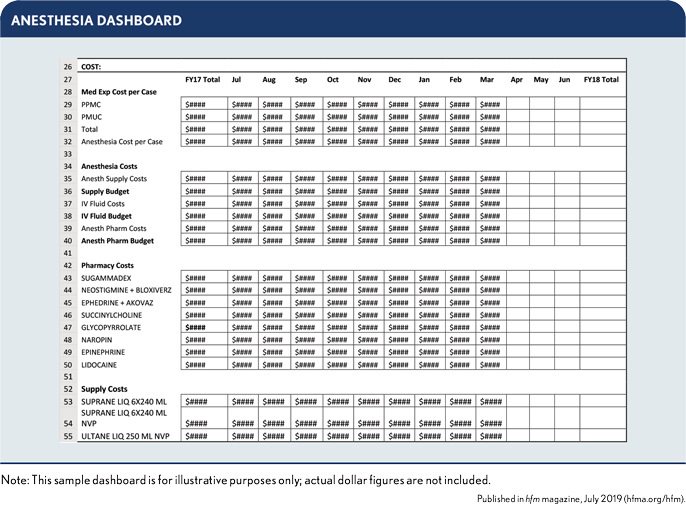
PPMC’s first step was to develop an anesthesia dashboard to track usage patterns in the anesthesia department for the various types of drugs used for anesthesia care. The tool was constructed to provide a 40,000-foot view of many aspects of the department, including staffing utilization, volume, safety, quality and efficiency and cost. (See the exhibit below for a snapshot view of the type of cost analysis that the dashboard makes possible.)
On drilling down to analyze medication expenses, PPMC noticed anesthesia providers were frequently using ephedrine, a high-cost drug whose purpose is to raise blood pressure and heart rate during anesthetic cases or in the ICU. Anesthesia providers would routinely have ephedrine drawn and available as a rescue medication even when a patient had no impending need for the intervention. The drug had been in use for so long across the industry, having been first isolated in 1885, that anesthesia specialists assumed its cost was negligible. They were incorrect in this assumption, however, because they were unaware that the cost of ephedrine had increased significantly over many years.
In addition to helping PPMC identify the need to change this practice, the dashboard also pointed to a less expensive but equally efficacious alternative to the routine use of ephedrine: another medication called epinephrine. Although epinephrine is not exactly the same as ephedrine, it does have similar effects, is as effective and does not pose a patient safety risk. Getting all anesthesia providers on board with this change would require the perioperative group and hospital to adopt a new vision, which was something that could not be accomplished overnight. It would require a journey.
(See the sidebar for a discussion of the steps PPMC took top create the dashboard. The discussion also includes a link to an Excel template that can provide a basis for developing a similar dashboard.)
8-step process: application of change management principles
To realize the necessary practice changes, PPMC used the eight-step process outlined below, based on the “8-Steps for Leading Change” described by John P. Kotter, MD.a
1. Create a sense of urgency. The anesthesia dashboard alone was sufficient to create the sense of urgency: It showed medication costs were out of control, and at the top of the cost list was ephedrine. As a perioperative center with 31 operating rooms (ORs), PPMC saw it was spending $30,000 to $40,000 per month on this single drug. The clinicians were in disbelief, prompting the pharmacy department to recheck the numbers and confirm that the annual opportunity cost for ephedrine amounted to hundreds of thousands of dollars. These findings created a sense not only of urgency but also of excitement.
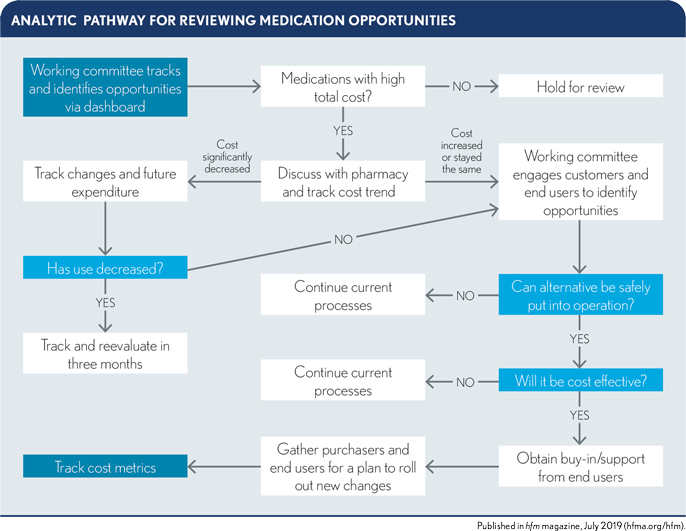
2. Form a guiding coalition. PPMC recognized that collaboration from a diverse group was required to understand the opportunity, outline alternatives, agree on the solution and create a new process. Perspectives of diverse stakeholders were needed, ranging from those charged with the initial decision to purchase medications, to those on the administrative team responsible for budgeting medication costs, to end-user clinicians delivering the direct patient care. To provide the necessary oversight, PPMC established the Medication Value Committee, comprising leaders from administration and the departments of anesthesiology and critical care, pharmacy and finance. Then committee was charged with reviewing and evaluating medication opportunities within inpatient (including OR), skilled and outpatientareas of PPMC. (See the exhibit below for the analytic pathway the committee used for this purpose.)
3. Create a strategic vision. The committee mapped out a plan to exchange ephedrine with the less-expensive epinephrine. The clinical members provided crucial input regarding how to create a safe and cost-effective process for making this change, including assigning additional pharmacy staff to accomplish the task. Compounding or pre-making the epinephrine in syringes to replace ephedrine required an additional pharmacy technician to support the increased workload. Even after accounting for the costs of these resources, the committee projected a solid six-figure gain from the initiative.
4. Communicate the vision. Successful health systems need to be cautious with increasing personnel costs, which become a recurring fixed annual expense for the system. For this reason, the committee first needed to obtain approval from PPMC’s CEO and CFO for increasing the pharmacy staff outside of the normal budget cycle. They presented the projected savings and ROI to the CEO and CFO, and to anyone else who might have influence to sway their decision. The vision also was presented at processimprovemen meetings, anesthesia and executive leadership meetings and even in impromptu discussions in the hallway. The two executives approved adding an FTE on a one-year trial basis, providing a defined timeline for proving the concept and demonstrating projected savings.
5. Empower others to act on the vision, enabling action by removing barriers. Before the initiative could move forward, the committee needed to remove any barriers that impeded further action. First was the need to build consensus among committee members regarding next steps. The team also required authorization for engaging with other stakeholders to gain their buy-in and bring them on board. These stakeholders included:
- Front-line providers who delivered the medications to patients
- Pharmacy staff charged with pre-drawing the medications
- Purchasing staff, who were in constant negotiations with vendors
- The medical departments, which would not see direct financial gains from the reduced costs
The approval to proceed by the CEO and CFO was instrumental in removing these barriers to action.
6. Plan and create short-term wins. Obtaining positive results from switching from ephedrine to epinephrine would be the quick win needed to validate the committee’s overall mission and change-management approach. Full implementation of the shift in anesthesia drugs began after a small price drop in November 2016. Through emails, word-of-mouth and weekly departmental meetings, the committee informed and educated the anesthesia providers about the cost of ephedrine and requested that they refrain from routinely using the medication. They also promoted the benefits of epinephrine, with the result that by May 2017, the anesthesia group had adopted the alternative medication. The committee’s clinical members were instrumental in driving these results.
The initiative’s definitive accomplishment came in July 2017, when pharmacy staff began to routinely provide pre-drawn epinephrine syringes, thereby completing the shift in choice of medication. Ephedrine would still be available for use if a clinician deemed it necessary. But overall, staff were satisfied with the changes and the ease of use of the pre-drawn syringes.
7. Consolidate improvements and accelerate more change thorough sustained improvement activities. The success of the ephedrine/epinephrine initiative enabled the committee to turn its attention to the larger task of extending drug cost savings across the entire health system. By reinforcing and legitimizing PPMC’s approach, the ephedrine/epinephrine initiative paved the way for the broader use of medication dashboards to identify high-cost and frequently used medications and to encourage staff to look for savings opportunities. As identifying additional opportunities became easier, the use of dashboards expanded, to the point that a half a dozen additional medications are currently under review and the committee also is looking at using the approach for achieving cost savings on disposable equipment in the perioperative area.
8. Institutionalize new approaches. PPMC’s process has been extended to other hospital entities across the University of Pennsylvania Health System through executive informational meetings and systemwide groups such as the Penn Medicine Anesthesia Consortium (PMAC), a committee of the anesthesia leaders for the system, and the University of Pennsylvania Health System Perioperative Consortium, comprising system perioperative leaders. With the expansion of the Medication Value Committee’s role beyond PMCC, the pharmaceutical cost-reduction approach is well on its way to becoming an integral part of the health system’s operations.
Results and impact
To test the effects of the ephedrine/epinephrine initiative, the Medication Value Committee used the anesthesia dashboard to track pharmacy costs for ephedrine and epinephrine during the initial implementation period of July 2016 through November 2017. PPMC experienced a nearly continuous decrease in drug costs, from averaging $38,000 per month up to November 2016 on ephedrine alone to a little under $8,000 for both ephedrine and epinephrine (about $4,574 and $3,155 for each, respectively) as of November 2017. The new use pattern emerging five months after the intervention was compared with an established 12-month base period, and results were annualized to project the impact of the change. This single intervention reduced spend by 67%.
As noted, after completing the ephedrine/epinephrine initiative, the Medication Value Committee turned its attention to several other medications, adding two full-time pharmacy technicians to the staff to expand its work and role. Annual savings for FY19 are projected to approach half a million dollars. And as the process is further expanded into PPMC’s sister hospitals in the University of Pennsylvania Health System, net savings are expected to grow well into the seven-figure range — all from what started as a one-hour biweekly committee meeting and a plan designed around time-tested change management strategies.
Footnotes
a. One of the foremost leaders in change management and author of 20 books on the subject, Kotter is Konosuke Matsushita Professor of Leadership, Emeritus at the Harvard Business School and the founder of Kotter, Inc., an international firm dedicated to promoting leadership principles (see kotterinc.com).





