How investing in the workforce can improve a health system’s bottom line
Like health systems nationwide, Keck Medicine of USC saw workforce challenges explode in the wake of the pandemic. The health system has met those challenges with a systematic approach to workforce well-being and resiliency.

The year 2022 will be remembered as one of the worst financial years on record for healthcare. It will also be recalled as the year when the anticipated workforce shortage moved from being just one of many strategic concerns for health system leaders to becoming their most critical and urgent challenge.
The rapidity with which the intensified workforce crisis was sweeping across the healthcare industry prompted Los Angeles-based Keck Medicine of USC to reconsider its workforce strategy. The health system’s leaders recognized that devoting resources to the well-being and resiliency of the healthcare workforce is essential, not optional. They also came to see that these outlays of resources — time, effort and dollars — should be viewed not as expenses and financial burdens, but as investments that will produce a greater payoff in the future.
3 focus areas to improve ROI
Keck Medicine also saw opportunities to view these investments through a new lens, by focusing on the following three areas, which showed the greatest promise for delivering a strong ROI and improving the organization’s bottom line: retention, safety and professionalism, and organizational culture and health.
1 Retention
Keck Medicine executives had been mindful of news stories reporting study findings of widespread dissatisfaction among healthcare workers. Healthcare staff were reporting that they felt unfulfilled and lacked a sense of belonging and connection — findings that the leaders recognized should not be overlooked or undervalued. Multiple studies had shown that people who report a sense of belonging are more likely to perform exemplary work, build stronger relationships with colleagues and go above and beyond for their organizations. These were employee attributes that Keck Medicine wanted to work hard to retain.
Healthcare organizations had tended to view turnover as a normal cost of doing business. But Keck Medicine leaders recognized the fallacy of that idea. Organizations pay a high price for attrition and for the less visible costs of absenteeism, low morale and lower productivity. The American Medical Association (AMA) found that the cost to replace a physician in 2018 ranged from two to three times their annual salary.a AMA also reported in 2022 that job turnover of primary care physicians adds $979 million to the nation’s annual excess healthcare costs. However, the largest cost associated with replacing a physician is the opportunity cost of lost patient care revenue.
Focus on promoting well-being and resiliency. Even before the pandemic, Keck Medicine had been designing a systemic approach to workforce well-being and resiliency. The approach, called Care for the Caregiver, was based on the premise that physicians and other staff will be more satisfied with their work roles and more likely to stay with an organization if they are offered meaningful support systems.
As it became clear with the pandemic that the workforce would experience unprecedented levels of stress for a prolonged and uncertain time, the health system accelerated efforts to refine and roll out Care for the Caregiver. Programs focused on initiatives to help staff and physicians cope with stressors in the work environment. But it also became quickly apparent that Keck Medicine could also provide support to staff to fulfill their responsibilities outside of their work lives.
Keck Medicine expanded initial programs focused on providing meal and grocery services, housing and peer group support by adding childcare services, legal assistance, emergency financial assistance and online tutoring for children of physicians and staff. A robust feedback loop allowed the workforce to comment on existing support services and suggest additional ones as the COVID-19 crisis persisted.
Keck Medicine also tapped into USC’s university resources and community partnerships, which provided programs such as music therapy (in a program called Music as Medicine).
Focus on program expansion. Programs continue to be added, including more than 2,300 grants representing $939,000 in Keck Kindness awards that assist employees with financial support to assist with an immediate monetary need.
Other retention strategies Keck Medicine is using include a boomerang strategy — hiring back workers who left during the pandemic. Using feedback solicited during exit interviews, former workers are given incentives to return. As of November 2022, Keck Medicine had rehired 224 staff members.
Keck Medicine has also secured a $2 million grant from the UniHealth Foundation to fund a clinical research trial that will explore approaches for improving mental health and job satisfaction of clinicians. Four hundred participants will participate in the trial that examines three major elements of clinician burnout and demoralization: emotional stress, skill mastery and workflow. Research findings will be used to continue to refine the Care for the Caregiver program and other support systems.
Commitment to transparency and program assessment. Reflecting its commitment to program transparency, Keck Medicine shares a dashboard with leaders to demonstrate how the Care for the Caregiver programs are being used. The health system also uses staff feedback to assess the impact of these programs.
While hearing directly from staff is powerful, Keck Medicine does not rely on the hunches and anecdotal feedback to assess the impact of these programs. Keck Medicine also uses a SCORE (Safety, Communication, Operational Risk, Resilience/Burnout, Engagement) survey instrument to identify challenges and barriers to delivering highly reliable patient care.
Keck Medicine survey results point to success in fostering resiliency and well-being within the health system’s workforce

instrument for identifying challenges and barriers to delivering high-reliability patient care.
Retention results. On a number of key metrics, Keck Medicine has demonstrated progress — even during the pandemic. Key improvements include:
- Highest improvement in local leadership scores by any peer system
- Reduction in employee burnout risk of about 33%
- Work-life balance score improvement of four points; 90th percentile nationally
- Teamwork domain score increased seven points, which is the largest increase among peer health systems
- Nine-point improvement on “I would feel safe being treated here” bellwether question
- Zero-point change in burnout climate, while most other systems saw drops of 5 to 10 points
While Keck Medicine’s focus on resilience and wellness has been driven by its commitment to caring for its workforce, an added benefit has been over $400,000 in insurance premium discounts in FY2022 due to the Care for the Caregiver program, culture of safety and transparent communication practices.
Most important, Keck Medicine’s turnover rates are well under the national averages based on PwC benchmark data, with a hospital turnover rate of 12% (compared with 20.7% nationally) and a staff registered nurse turnover rate of 13.3% (compared with 21.1% nationally).
2 Safety and professionalism
Another important workforce-related area of concern is attentiveness to clinicians exhibiting signs of high stress and exhaustion, as they don’t collaborate well with colleagues, which can create difficult work environments for their coworkers.
These clinicians are also more likely to make mistakes. Researchers from the Stanford University School of Medicine linked burnout to medical errors across specialties, finding that within a three-month period, physicians who reported signs of burnout were twice as likely to self-report a medical error.c
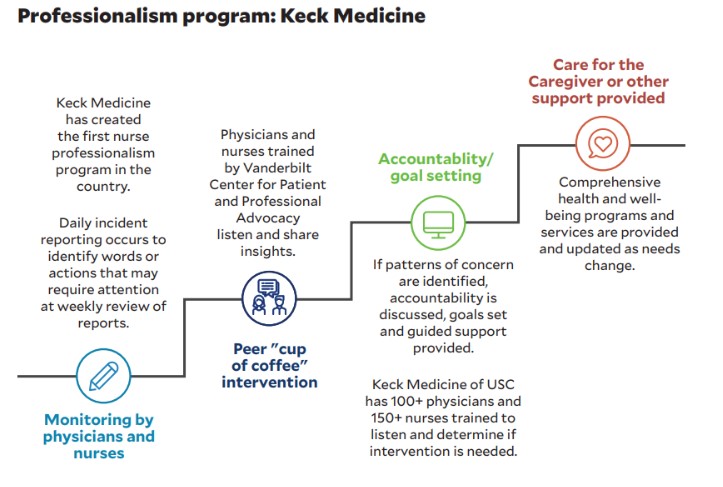
To address this concern, Keck Medicine embarked on a six-year journey in 2016 to create a culture of professionalism, in part to help detect individuals in need of early intervention. This program is built on the philosophy that professionals want to be professional and that, given the opportunity to reflect on flawed behavior in the work environment, they will self-correct.
About 150 nurses and 100 physicians from Keck Medicine who received training by the Vanderbilt University Medical Center for Patient and Professional Advocacy perform daily monitoring and incident reporting. In response to an incident, group members are charged with listening and sharing insights, ultimately to determine whether a “cup-of-coffee” intervention (i.e., a one-on-one meeting in a non-threatening environment) is needed. If patterns of concern are identified, accountability is discussed, goals are set and guided support is provided for as long as needed.
Keck Medicine’s nurse and physician professionalism programs have conducted 50 interventions over a five-year period, and they found demonstrated improvements in 92% of interventions, with only 8% of caregivers departing the organization — a rate much better than national averages.
3 Organizational culture and health
Keck Medicine recognized that success with any initiatives focused on retention and safety and professionalism depended on organizational culture and health, as all these areas are inextricably linked. When an organization’s culture communicates to employees that their employer is invested in them — including their career development — they are more likely to stay loyal to an organization.
A key tenet of Keck Medicine’s workforce strategy is that an organization’s culture is strengthened by the opportunities for growth that the organization provides. Keck Medicine recognized that such opportunities must speak to employee’s passions and desire for performing meaningful work. They wanted viable career paths and opportunities to enhance their quality of life and avoid feelings of stagnation.
A key consideration is the potential impact of the loss of institutional knowledge, which can be costly to develop, on both the daily provision of services and key initiatives. Keck Medicine’s goal, therefore, was to offer workforce development programs that signaled to existing staff and to potential new hires that the organization cared about them as individuals.
Keck Medical Center, Keck Medicine’s flagship facility, launched a mid-level leadership development program in 2022 focused on creating a culture of purpose with its caregivers and staff. The program had origins in a recent nursing strike, when nurse managers were challenged with finding ways to effectively communicate with and manage nurses during and after a labor strike.
Keck Medicine solicited feedback amounting to 95 hours from managers and directors regarding opportunities to improve its work environment. The health system used that feedback to create a framework for helping managers and directors understand staff needs for support and resources, as well as barriers to high performance, so they could become transformational leaders rather than just overseers of day-to-day tasks. The framework ensures that leaders have a common understanding of barriers, support and resource needs and that the goals of each operating unit are aligned.
The health system also has been careful to ensure the program, which is still in the early stages of implementation, does not create additional duties for managers and directors. Rather, it is designed to be a tool to help them feel supported, focused and aligned with others through ongoing conversations and periodic reviews. The tool enables them to measure several domains to assess progress:
- Performance and outcomes
- Alignment and priorities
- Worthwhile work and engagement
- The ability to make a difference and create a sense of belonging
To ensure the leadership development program receives the commitment and attention it should, Keck Medicine is piloting offering managers a stipend for implementing it.
Keck Medicine’s seven employee resource groups (ERGs) are also being strategic in using their platforms to foster a culture of safety, recognition and inclusion in their work environment and community and better respond to workforce needs. From the Armenian Health Professionals of USC to Keck Pride, these groups have been advancing personal and professional development and building inclusion using events on topics such as personal finance and gender-affirming care, which have helped drive growth in ERG participation by over 18% in the last six months.
The path forward
Healthcare’s workforce crisis will not be solved in the near term. The labor pipeline is too deficient to hire or pay a way out of the current situation. But action is needed. For Keck Medicine, the path forward has been to care for staff through investments in retention, safety and professionalism, and organizational culture and health.
Footnotes
a. Berg, S., “How much physician burnout is costing your organization,” AMA, Physician Health, Oct. 11, 2018.
b. Henry, T.A., “Nearly $1 billion in excess patient costs tied to physician turnover,” AMA, Physician Health, May 24, 2022.”
c. White, T., “Medical errors may stem more from physician burnout than unsafe health care settings,” Stanford Medicine news center, July 8, 2018.
Conflicting trends portend increasing workforce challenges for healthcare
According to the Bureau of Labor Statistics, employment in healthcare occupations is projected show 13% growth from 2021 to 2031 — much faster than the average for all occupations in the United States. This growth will add about 2 million new jobs during this 10-year period, while it is projected that roughly 2 million jobs will open each year as a result of the need to replace existing staff who leave for various reasons.
A study published in Mayo Clinic Proceedings revealed that nearly 1 in 3 physicians and nurses reported a clear intention to reduce work hours, and nearly 2 in 5 nurses and 1 in 5 physicians intend to leave their practices altogether.a
This confluence of the labor supply shrinking, while demand for services grows, is having a profound impact. Hospitals and health systems are paying $24 billion more annually for clinical labor than they did pre-pandemic, placing current and future missions at risk, slowing or halting transformational initiatives and jeopardizing their ability to manage future potential health crises.b
These challenges are forcing healthcare employers to rethink how they view their workforce. They have long viewed employees as costs to be minimized, and regarded wellness programs as opportunities to lower healthcare insurance costs, not to directly address stress and burnout. While attitudes have changed, action has not been robust. A study by WTW found that while 86% of employers said that mental health, stress and burnout are a top priority, 49% have not formally articulated a well-being strategy for their workforce and only 25% have articulated and adopted a well-being strategy. c
Footnotes
a. Sinsky, C.A., Brown, R.L., Stillman, M.J., and Linzer, M., “COVID-related stress and work intentions in a sample of U.S health care workers,” Mayo Clinic Proceedings, Dec. 8, 2021.
b. Premier, “PINC AI data shows hospitals paying $24B more for labor amid COVID-19 pandemic,” Blog, Oct. 6, 2021.
c. WTW, “Employers pinpoint workforce mental health as one of HR’s top priorities for 2022,” Press release, Jan. 24, 2022.





