4 goals for bundled payment: How a hospital succeeded under BPCI-A
An East Coast hospital’s positive experience participating in the Bundled Payments for Care Improvement Advanced model reinforces why it is imperative for organizations to clearly define their goals for participation before moving ahead with the model.
As a community hospital in Abington, Pennsylvania, Abington Hospital has achieved success participating in CMS’s Bundled Payments for Care Improvement Advanced (BPCI-A) Model through the understanding that certain episode bundles offer greater opportunities for improvements than others. The hospital secured a clear clinical and financial rationale for model participation, which, along with the target-price opportunities that were presented, informed decision-making. Three factors in Abington’s approach to BCPI-A were instrumental in driving its success under the model:
- Thoughtful deliberation, with an awareness of the increased demands on organizations under BPCI-A, compared with the original BPCI program, to implement effective interventions aimed at decreasing costs and improving quality for episodes of care
- A clear knowledge of its goals for participation
- The capability to assess where the greatest opportunities lie
Case study: Abington Hospital
Abington Hospital is a 655-bed community-based teaching hospital within Jefferson Health, a health system serving Philadelphia and the surrounding areas of Pennsylvania and New Jersey. The hospital first participated in BPCI before embarking on BPCI-A. In April 2015, Abington enrolled in the major joint replacement lower extremity (MJRLE) episode, which the hospital dropped in 2016 due to a change in the orthopedics group with which it worked. Although Abington participated in the MJRLE episode for only one year, it still saw success between the baseline and when it dropped the episode, including:
- A 54% reduction in patients discharged to a skilled nursing facility (SNF)
- A 26.3% average decrease in SNF length of stay (LOS)
- A 35.8% decrease in readmissions for MJRLE episodes
Although Abington dropped the MJRLE episode, it chose to continue in the BCPI model with stroke and congestive heart failure (CHF) episodes. Through its participation in both BPCI and BPCI-A, Abington directed its efforts at enhancing the quality of care it delivered by increasing patient engagement and improving care coordination and care transitions.
The role of nurse navigators
Under BPCI, Abington invested heavily in care transformation to improve quality of care and established a nurse navigation program, in which navigators were charged with:
- Furnishing the initial information on the program to patients
- Collaborating with multidisciplinary inpatient and outpatient teams for a safe and effective discharge
- Providing follow-up from 24 hours after discharge extending through the 90-day episode
The care navigators worked with patients to deliver disease and care management, including goal setting and teach-back techniques, encouraging follow-up and self-monitoring, and providing an ongoing link between the hospital and SNFs. Navigators also reviewed a zone management action plan, where different zones are established that indicate disease progression and outline the necessary steps a patient or caregiver must take in those circumstances. Navigators also assisted, as necessary, in scheduling appointments, arranging for transportation and initiating referrals for community services.
Abington’s episode selection process
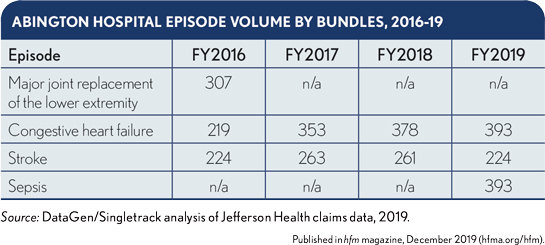
When BPCI-A began in 2018, Abington chose to remain in CHF and stroke episodes, while also pursuing a new episode, sepsis. Abington chose to focus on these episodes because they had sufficient volume to be financially stable and presented significant opportunities for reducing expenditures on post-acute care (PAC). High-volume episodes are preferable, because increased volume increases the reliability and generalizability of the data. (See exhibit below.)
Abington’s decision to participate in the stroke episode was based on its previous investment in this episode under the original BPCI program, creating the opportunity to leverage its existing nurse navigation program for the population.
4 goals for participation
The hospital also determined its successful participation in CMS’s BPCI-A model would depend on the extent to which it could achieve
the following four goals.
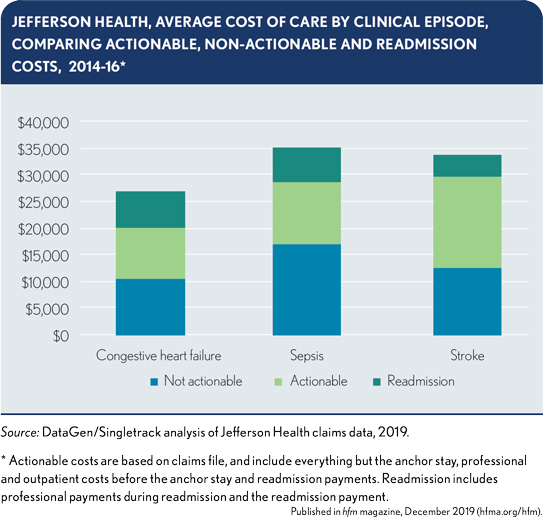
Goal 1: Achieve clinical transformation where there is a clear financial opportunity. Abington began the episode selection process by working with its clinical and analytic teams to identify episodes that had both clinical champions and sufficient opportunities to reduce costs below CMS’s target prices. To identify these opportunities, it was necessary for Abington to analyze the proportion of costs that were actionable, meaning the costs could be affected by clinical changes. The cost of initial hospital admission is not considered actionable, for example, because it has a fixed DRG payment. Similarly, physician services also are largely fixed. Actionable costs, therefore, primarily consist of PAC, institutional and home health services, as well as readmissions. (See exhibit below.)
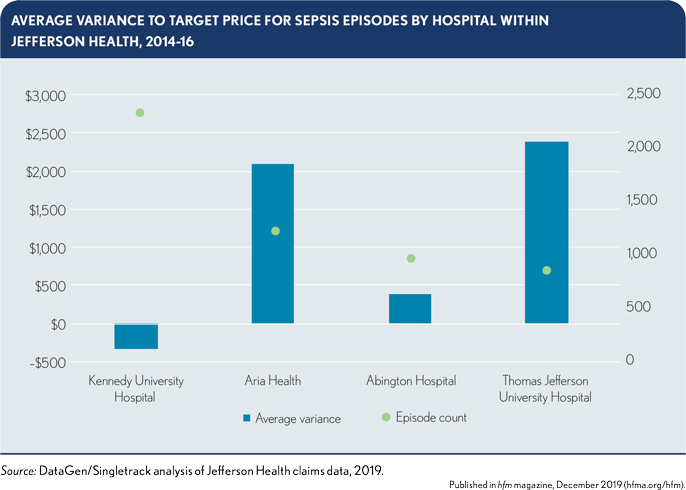
For Abington and other hospitals within Jefferson Health, there were strong clinical and financial opportunities associated with sepsis. Jefferson New Jersey, comprising three hospitals that are part of Jefferson Health, had previously implemented interventions to address sepsis as one of the leading causes of readmissions. In addition, two Jefferson Health hospitals had episode costs that were already above their target price in the baseline period, while the other two hospitals were only slightly below target, as shown in the exhibit below.
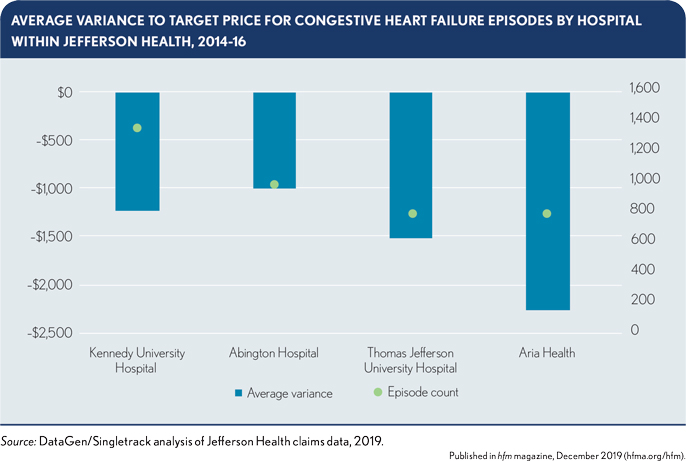
Goal 2: Extend clinical transformation to places where there is limited financial opportunity. Based on Abington’s previous success with CHF in the original BPCI program, Jefferson Health chose to participate in CHF episodes during BPCI-A, even though the episode targets were somewhat less favorable than the sepsis episode targets, relative to the organization’s baseline spending. This less favorable target price for CHF occurred as a direct result of the efficiency factor, which intentionally sets lower targets for already-efficient participants. (See the exhibit below, and see the sidebar, “How CMS sets the target price for bundles under BPCI-A,” for additional detail on the efficiency factor.)
Abington had previously established clinical champions and programs for CHF, creating opportunities to build on and extend interventions to other hospitals within Jefferson Health. These CHF initiatives resulted in:
- A 16.8% decrease in SNF admissions
- A 23.5% decrease in SNF LOS, on average
- A 24% reduction in readmissions for Abington between the baseline in 2012 and the start of BPCI Advanced in 2018
Based on these investments, Abington determined that the potential existed to lower episode costs below the target price by improving quality, which was founded on the system-level clinical transformation the hospital was pursuing for CHF. The emphasis on clinical change and quality was the driving force behind this participation decision, because the financial targets for CHF episodes presented greater challenges than those for sepsis.
Similarly, Abington selected the stroke episode based on the inpatient and outpatient interventions implemented during the original BPCI model. Abington had achieved success with stroke bundles in BPCI by investing in the development of new clinical resources, including the nurse navigation program and a preferred-provider SNF network. These interventions resulted in strong clinical outcomes and high patient satisfaction. For stroke episodes, Abington saw:
- A 9% decrease in SNF admissions
- A 25.5% decrease in SNF average LOS
- A 15.2% reduction in readmissions between the baseline period in 2012 and the start of BPCI-A in 2018
Goal 3: Build a value-based care infrastructure. Abington’s participation in stroke episodes reflected its desire not only to maintain and build upon the success of existing clinical initiatives, regardless of the limited financial opportunities, but also to establish value-based care capabilities. For example, Abington’s nurse navigation program was not limited to its care management capabilities for stroke episodes, but extended to the provision of a template the hospital could apply to other conditions.
Abington also saw the preferred SNF network, which it developed for the original BPCI program, as a component of its value-based care infrastructure, which could be expanded to new episodes. Leaders from this SNF
network meet with Abington and disease- specific hospital leaders monthly to discuss facility statistics, readmission initiatives, educational opportunities, new programs, and issues or concerns. Abington’s emergency department staff also developed a tool to
connect physicians and staff with SNFs to discuss patient care plans.
Goal 4: Develop the capability to analyze data on episode performance. Jefferson Health’s analytics department performs ongoing analyses on each individual episode to identify appropriate quality improvement opportunities, which drives performance under BPCI-A. The analytics team tracks acute care hospital and PAC LOS, assigned case costs, readmission rates and excess acute days, all of which are collected from the CMS claims provided through both BPCI models. Based on the analyses, Abington created
care redesign plans centered on increasing efficiencies by reducing duplicative and unnecessary services, supporting appropriate care transitions and improving medication reconciliation. This effort resulted in the adoption of shared care plans and reductions in admissions, LOS, unnecessary prescriptions and adverse effects.
Under the shared care plans, the facility and the index hospital agreed to care for patients under BPCI-A collaboratively. Best practice guidelines from evidenced-based research are relayed to the facility from the navigator. For preferred SNFs and many community partners, in-person educational sessions were scheduled to review and teach key employees in the SNF. The navigator is the gatekeeper to relaying the care plan to the facility and assuring that the facility follows through. Collaboration occurs between the navigator and the facility when managing high risk patients.
Conclusion
BPCI-A offers opportunities for patient-centered care improvements that focus on the entire continuum of care. However, certain episode bundles offer greater opportunities for success than others.
Abington Jefferson Health has demonstrated, through its participation in sepsis, stroke, CHF and joint replacement episodes, the clinical and financial reasons that drive health system participation in these models. By investing in clinical transformation and value-based care infrastructure, Abington Jefferson Health is establishing itself as a leader within its health system and community in delivering high-quality, high-value care.
Sidebar: Why participate in BPCI-A
Hospitals and physician group practices participate in CMS’s Bundled Payments for Care Improvement Advanced (BPCI -A) model to meet a range of goals. The decision-making process used by Abington Hospital around the selection of each episode encompassed four goals considered by many hospitals:
- Invest in care transformation with the potential for shared savings, through the identification of episodes with strong clinical and analytic opportunities.
- Maintain the success of existing clinical initiatives, even for episodes with limited financial opportunities.
- Develop value-based care experience in preparation for the potential introduction of mandatory models, by building out infrastructure for care transitions, data analytics and health IT.
- Obtain data in support of other quality-improvement work, such as initiatives targeting CMS’s Hospital Readmission Reduction Program.





