A crisis of faith regarding value-based care
Finance executives surveyed for HFMA's third and final series of 'Healthcare 2030' reports describe an industry not ready to tie payment to value, with some wondering if there is a need to do so.

As the movement to reduce or eliminate fee-for-service payment in favor of value-based payment plods along, some in the industry are voicing doubts that it is ever going to happen or that it is even necessary.
An HFMA survey conducted in February and March for the “Healthcare 2030” series of special reports finds some of the 105 finance executive respondents to be a little irked by the concept.
Meanwhile, both large employers and some industry experts say they doubt that things will change under current conditions.
“Prices have gone up dramatically and quality has not,” said Elizabeth Mitchell, president and CEO of Purchaser Business Group on Health (PBGH), an employers’ group. Her comments appear in Part 2 of the “Healthcare 2030” series this year.
“So, value has decreased, and I do not see any serious attempts to change that by most of the industry players,” Mitchell said.
What all this means for the much-anticipated transition to value-based care is uncertain, but it’s almost certainly not good. The PBGH members’ feelings about progress have prompted them to explore other cost-saving efforts, such as by reducing specialty care spending through advanced primary care.
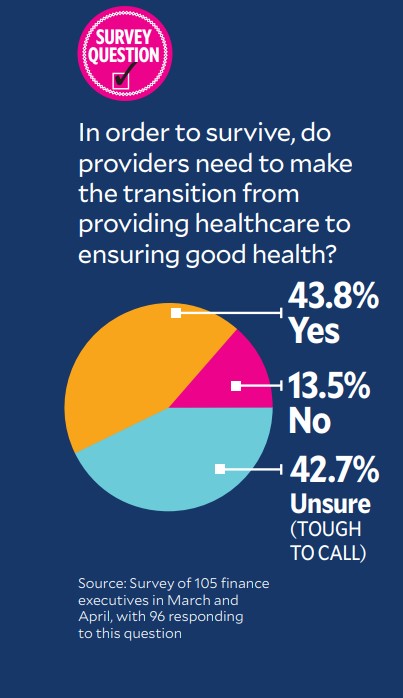
And as many survey respondents are unsure the shift to value is necessary as believe it is necessary.
Getting a stronger grip on primary care is something PBGH members believe is not a current capability of the U.S. healthcare system, which is creating opportunities for companies like Marathon Health, a primary care focused company catering to employers. On Aug. 1, Marathon closed on the purchase of Cerner’s Workforce Health Solutions unit, adding about 21 clients, 35 health centers and 300,000 members to its organization, growing its membership by about 30%, according to a spokeswoman. The purchase will expand Marathon’s footprint in 15 states, including a significant expansion in Chicago, Kansas City, Kansas, and St. Louis.
“Marathon Health’s goal is to become the leader in value-based healthcare in the commercial sector, by helping employers of all sizes achieve an advanced, population health driven model of primary care,” said Ben Evans, executive chairman and co-founder of Marathon Health, in a news release.
And Marathon is just one example of the many organizations tackling primary care and aiming to boost quality, lower costs and increase patient satisfaction. Others include Agilon Health, Aledade, ChenMed, Forward, Crossover Health, One Medical, Oak Street Health and Privia Health Group.
Moving at different speeds
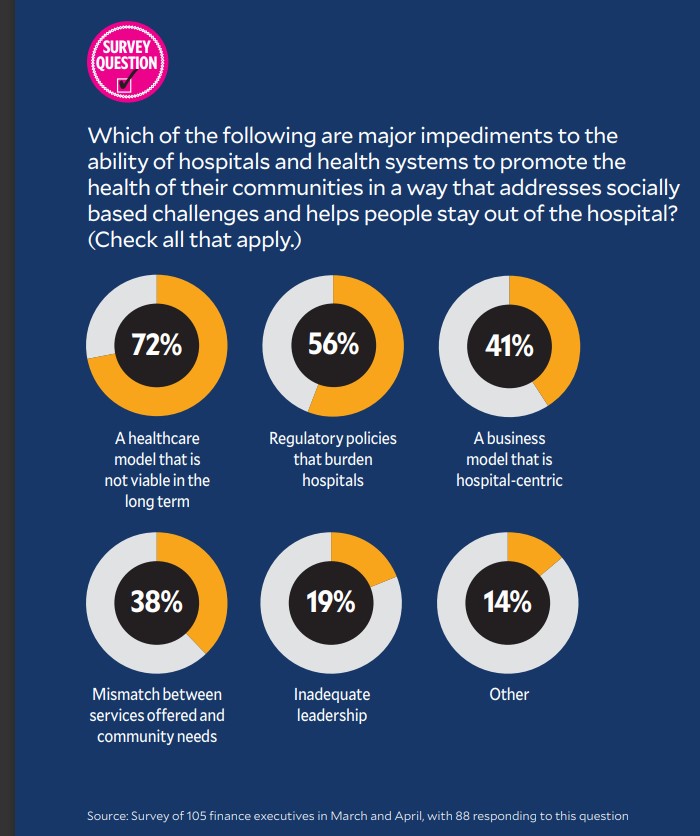
Results from the HFMA survey indicate that the hospital industry is at widely different stages in adopting a focus on promoting good health and stepping away from its traditional role of focusing solely on treating disease and conditions.
Some respondents have serious problems with the concept of needing to adopt value-based care. One put a lot of thought into criticizing the question, “Is the industry ready to accurately measure value and quality?”
“The construct that we need to get paid for value is rather insulting. Providers provide high value every single day,” the respondent wrote. “All the discussion around value-based payments is to drive down reimbursement and does little that will reduce care delivery costs.
“I don’t believe policymakers or the writers of this survey understand this industry very well. Absent breakthroughs in treatment, [value-based reimbursement] is just going to further damage the industry, which operates on tight margins industrywide.”
Another respondent said, “The question assumes there is national agreement about the value of healthcare. On the average, the country trails most developed countries on many measures, yet individual states or significant sections of states match or outperform other developed countries.”
One finance executive had low expectations and expressed them in blunt terms. The question was, “How difficult would the transition be from ensuring good healthcare to ensuring good health?” In response, the executive wrote: “We have tried to do this for many years. Some people are very focused on their health. The vast majority do not think about healthcare until they have a health issue. Even with healthy living, what we likely will see is simply deferral of the costs. A great objective but likely a fool’s errand.”
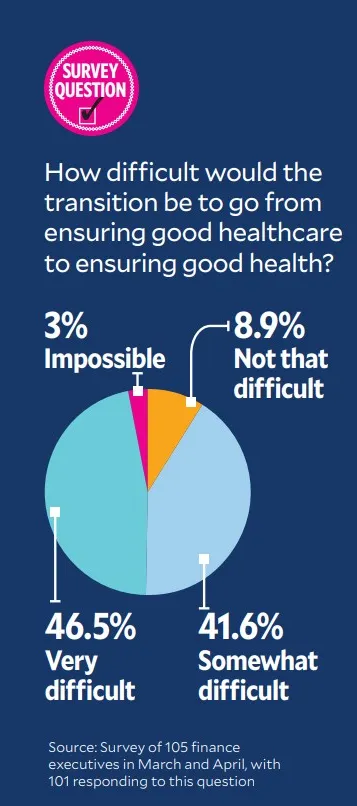
Still, nearly 42% of respondents said the transition to ensuring good health would only be “somewhat difficult” and almost 9% said it would be “not that difficult,” although none of the comments were very enthusiastic.
Putting the patient first
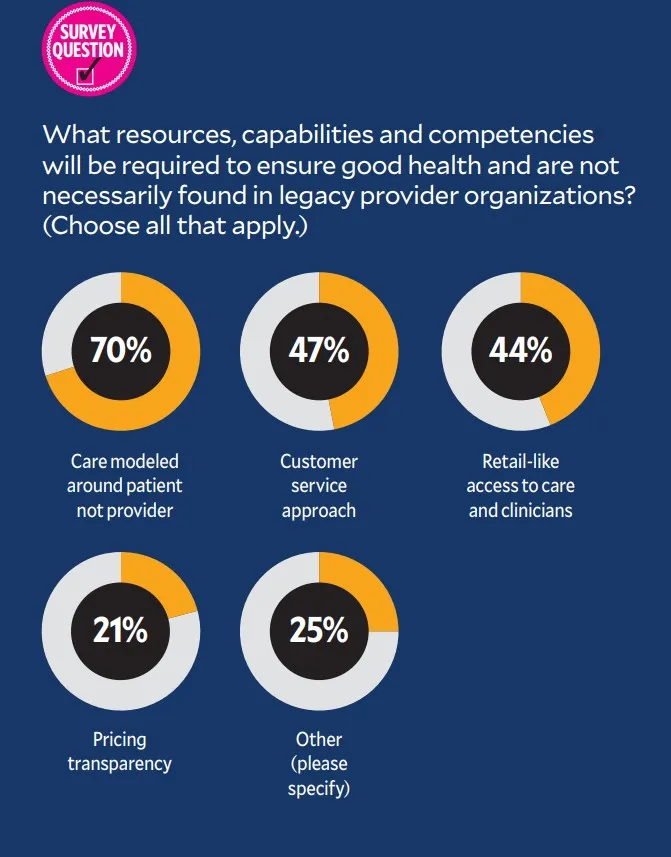
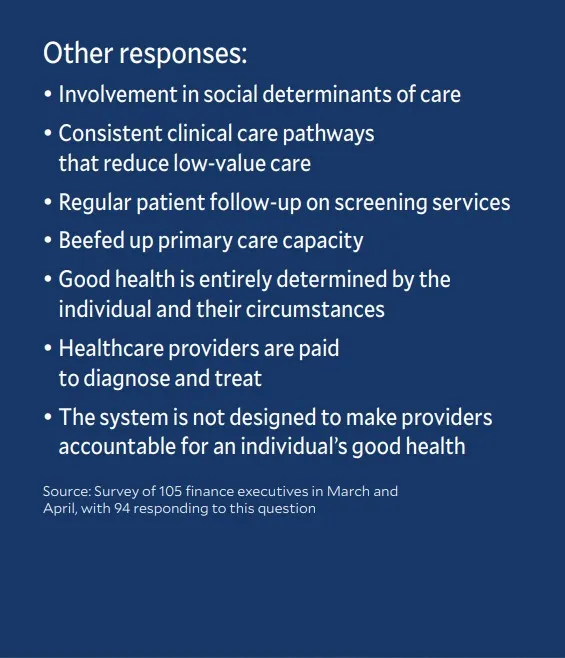
In open-ended responses to a survey question, some respondents cited concerns about gaining the capabilities needed to focus on health. Respondents left both positive and negative comments to the multiple-choice question “What resources, capabilities and competencies will be required to ensure good health that are not necessarily found in legacy provider organizations?” Among multiple answers offered, “care modeled around the patient” was the clear leader, with 70.2% of respondents choosing it.
Nevertheless, expect certain segments of the industry, including CMS, to ramp up their focus on promoting care relationships between providers and patients. The agency by 2030 expects to have: All Medicare beneficiaries with Parts A and B in a care relationship with accountability for quality and total cost of care and the vast majority of Medicaid beneficiaries in the same position.
Atrius Health, which operates more than 30 medical clinics in eastern Massachusetts and is part of UnitedHealth Group’s Optum, gets roughly 80% of its patient service revenue through value-based contracts, and it wants more.
“We’re all in,” said Patrick Holland, Atrius’ CFO. “Risk contracts are fundamental to our business model, and we seek out risk every chance we get.”
The health system SSM Health, based in St. Louis, also is seeking to improve value and is taking a patient-centered approach around care management, which includes a virtual care center that’s open seven days a week.
“The idea is to partner with patients,” said Laura Kaiser, president and CEO, quoted in Part 1 of this year’s Healthcare 2030 report. “If you have a strong care management system from stem to stern, patients and families can partner with their care team and won’t get lost.”





