Key takeaways from HFMA’s latest Outlook Survey: Healthcare finance professionals anticipate technology-driven changes
- HFMA’s most recent Outlook Survey of healthcare finance professionals highlights the potential of technology to usher in big changes in upcoming years.
- The possibility that reimbursement will be further restricted is a key area of concern.
- Among the likely permanent impacts of the COVID-19 pandemic is a shift in the traditional workforce model.
Healthcare finance professionals are getting ready for technology to change the way they and their organizations do business, according to results of HFMA’s Outlook Survey.
The most recently published iteration of the quarterly survey was conducted in August 2021, drawing from a cohort of 542 HFMA members. While responses to questions about short-term trends are subject to change based on the course of the COVID-19 pandemic, the survey results also showcase finance professionals’ thoughts about where the industry is headed.
Here are five important insights from the data.
1. AI is spurring transformation
Technology-based changes are seen as the “next big thing” that will revolutionize healthcare finance, according to responses to an open-ended question, with 25% of respondents naming innovations such as machine learning, AI, paperless and cashless transactions, and robotic process automation.
Ben Carter, executive vice president and COO with Trinity Health, was among the survey respondents. In the context of cutting-edge changes, AI is top of mind for his organization.
“It’s in clinical delivery, it’s in administrative spaces, revenue cycle, all of that,” Carter said.
The technology has the potential to “dramatically reduce the cost of healthcare because we’ll learn a lot more about how to effectively treat and where to treat [in terms of] site of care,” Carter said.
In addition, “rather than treat the disease as someone is diagnosed, it allows us to begin to be preventive.”
The ‘next big thing’ in healthcare finance
In your opinion, what is the next big thing that will revolutionize healthcare finance (open-ended question)?
Source: HFMA Outlook Survey, August 2021 (n = 152)
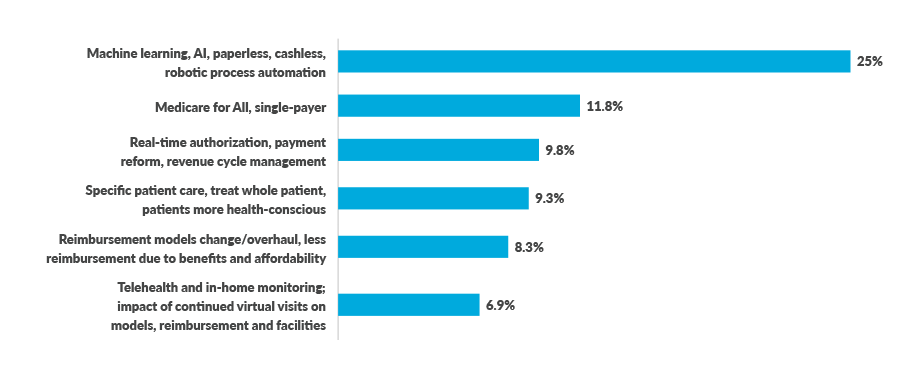
2. Telehealth isn’t the ‘next big thing’ — it’s already here
The emphasis on AI and similar technology represents a shift from the initial Outlook Survey, which was conducted in October 2020 among a different group of HFMA members. At that time, telehealth and in-home monitoring led the way with 17.3% of responses to the “next big thing” question as organizations sought to fill the gaps left by deferred in-person care during the first six months of the pandemic.
That selection was down to 6.9% in the latest survey, likely indicating the extent to which telehealth and virtual care already are part of core operations.
“Telehealth will be part of the care process for patients and consumers,” said Rick Gundling, FHFMA, CMA, HFMA’s senior vice president for healthcare financial practices. “There’s a greater understanding of which clinical specialties — such as behavioral health and primary care — can use telehealth to its full advantage.”
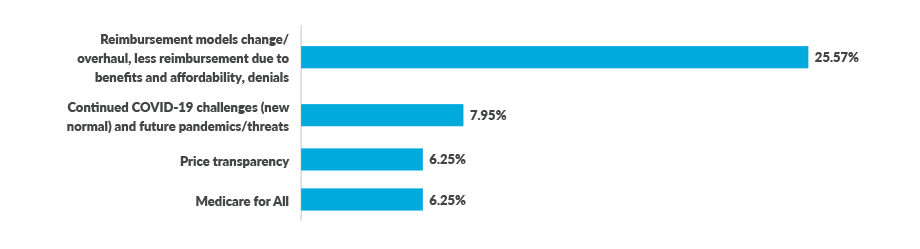
3. Looming challenges include reimbursement constraints
For a question about the challenges that the field of healthcare finance needs to be prepared for, the most frequently cited response was changes to reimbursement models and the possibility of less reimbursement. That issue drew 25.5% of responses in the latest survey, followed by COVID-19 continuing challenges that represent a “new normal” (7.95%).
The reimbursement response has been the most frequently cited in all four HFMA Outlook surveys to date while nearly doubling in share from 13.2% two quarters earlier.
“Under the current operating scenario where we’ve seen this huge step up in functional costs — labor and supplies and so forth — and payers who don’t want to pay, who want to go the other way, we’re really coming into a huge crunch time,” Carter said. “I think we’re going to see the further demise of hospitals, quite honestly. So alternative and lower-cost models of care are becoming more and more acute and critical.”
Trinity is seeking to deemphasize fee-for-service payment where possible, including by shifting more of its payer mix to Medicare Advantage and other value-based payment (VBP) models. But many VBP models aren’t structurally conducive to making a big impact, Carter has found.
Payers “always want to rebase,” he said. “Every time you rebase, you just ratchet everything down. The initial thought about it gets eroded.”
Preparing for challenges and constraints
In your opinion, what does healthcare finance need to be prepared for in the future (open-ended question)?
Source: HFMA Outlook Survey, August 2021 (n = 133)
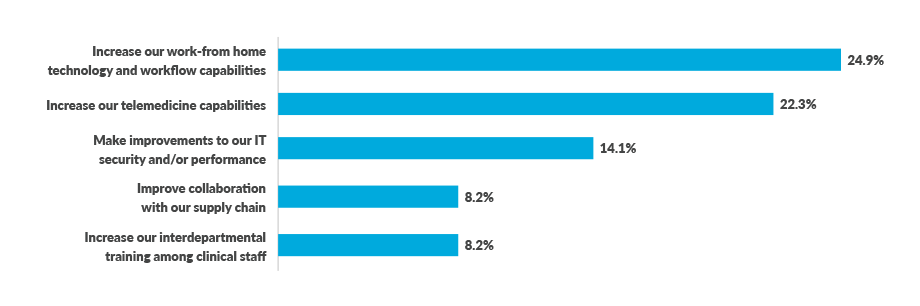
4. Workforce-related changes are rolling along
Regarding permanent changes being made as a result of COVID-19, the two most popular responses continue to be increasing work-from-home technologies and workflows (24.9%) and improving telemedicine capabilities (22.3%). Those have exceeded 20% in all four Outlook surveys.
“Not surprisingly after coping with the impact of the pandemic, healthcare leaders are highly focused on the ongoing efforts around the workforce,” Gundling said. “Coupled with that is the increased need to use automation and robots to perform supplementary tasks. Many healthcare organizations are struggling with recruitment and retention, so automation is a necessity.”
Carter said Trinity Health is moving to a remote model for all administrative functions, while clinical space also will be expendable as more care migrates to home and community settings. With those trends in mind, he said, the health system already has unloaded two “huge” buildings that amount to more than 120,000 square feet of space.
Changes stemming from the pandemic
What are the 3 most important permanent changes your organization will make as a result of COVID-19 (select up to three of 12 choices)?
Source: HFMA Outlook Survey, August 2021 (n = 119)
5. Costing remains a concern
As stakeholders consider how to improve the cost effectiveness of health, a prerequisite is being able to gauge the cost of care in the first place. Relatively speaking, technology is one operational area in which cost measurement has improved, with 29% of respondents saying their organization’s capacity has gotten “much better” or “somewhat better” during the pandemic.
Chaos and confusion in the supply chain have hampered efforts to measure the cost of care in that area, with 29% saying measurement has gotten “much worse” or “somewhat worse.” And 27% said the same about service line efficiency and labor costs.
“There is high awareness that data analytics and information technology capabilities need to be fully developed to truly impact the cost effectiveness of health,” Gundling said. “Many healthcare leaders are confident that they are on the journey, although they know it’s a never-ending process and needs to be a far-reaching strategy.”





