Evidence-Based Practice and the Bottom Line: An Issue of Cost

Healthcare costs are a driver of strategic decisions from the kitchen table to Capitol Hill. In the United States, strategies to improve care effectiveness and efficiency using best evidence began with nurses in the 1970s. In addition to curbing costs, evidence-based care addresses six components of healthcare quality: safety, effectiveness, patient-centeredness, timeliness, efficiency, and equitability.
Capturing the effectiveness of evidence-based practice (EBP) improvements offers a foundation for procuring necessary resources to do the work. Cost savings in our organization are generated by reducing ventilator-associated pneumonia, transfusions, falls, and frequent return visits in the emergency department (ED), among other examples. The bottom line is that EBP is the right thing to do—for our patients and for the organization’s pocketbook.

A Closer Look at EBP Evaluation
EBP is a systematic process designed to make improvements in health care. Once the evidence has been used to design the practice change, trialing for feasibility begins. A key aspect is evaluation of both processes and outcomes.
Baseline data illustrates existing practice patterns and current outcomes. Balancing measures can be used to explain outcome variances or capture unintended consequences of the practice change. For example, in implementing early ambulation of ventilated patients in the intensive care unit, is there an increased risk for falls? Balancing measures are particularly important when practice recommendations conflict or are ambiguous, and may help avoid unnecessary costs associated with abandonment of the practice or improvement that is not sustained.
Although the goal of EBP is to improve health care, the issue of cost must be considered in the value equation.
Practice changes require an upfront investment of time and resources. These investments are designed to create an improvement in outcomes, whether clinical (e.g., reduced infections), organizational (e.g., shorter length of stay), or fiscal (e.g., reduced unplanned readmissions, which helps the organization avoid Medicare penalties). Any of these may have cost implications. Some EBP improvements may not create cost savings but may achieve an equally valuable outcome (e.g., patient satisfaction) that helps fulfill the organizational mission.
Steps to EBP Evaluation
The first investment in EBP involves understanding current practice and the evidence for a practice improvement. From there, designing and implementing EBP requires inter-professional representation on teams to make decisions about how to engage patients and families, adopt practice recommendations, and integrate them into the normal workflow of busy clinicians. Time, resources, and cost analyses are needed.
A key in cost analysis is to calculate the ROI of the EBP, using the following steps (also summarized in the exhibit below):
Formula for Calculating the ROI of EPB
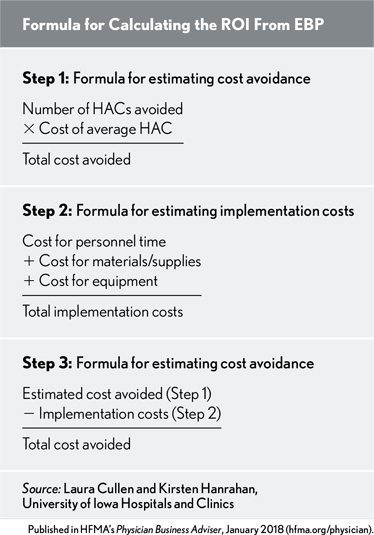
Step 1: Determine the cost avoided. This step entails calculating the volume of undesired events (e.g., hospital-acquired infection) multiplied by the cost of the event. The cost of an adverse event or hospital-acquired condition (HAC) may be most easily determined by the cost of an extended length of stay, but other costs also could 0be captured (e.g., diagnostic work-up).
Step 2: Determine the cost of implementing. Implementation requires investments in time and resources to promote adoption of the EBP. Budgets need to consider start-up and ongoing costs, including personnel, equipment, meetings, training to develop experts, training for clinicians, and resources for evaluation. Capturing such investments may be advantageous for establishing the benefit of the EBP.
Consider the need for establishing leadership support, developing champions, training new hires, and monitoring practice patterns and anticipated impact. Training and reinfusion will be needed to sustain the EBP improvement. Implementation costs often include personnel costs for meetings and training. Strategies such as academic detailing (a specific method for one-on-one education borrowed from pharmaceutical sales) require training and time with clinicians, but may be more effective for reaching clinicians with just-in-time (i.e., when and where you need it) messages and troubleshooting that supports adoption. This time for personnel is an opportunity cost, since clinicians could use the time in other ways for the benefit of the organization (e.g., patient care). These personnel expenses may not directly affect the organization’s bottom line if the position is salaried, but the effort needs to be recognized.
In calculating the personnel costs, compare them to the cost of standard care (e.g., 30 added minutes for transfusion administration and monitoring). In some cases, the change may not have an impact on time (such as in the case of a central-line insertion bundle) once the initial investment in implementation is made.
Add materials/supplies and capital expenses to personnel costs. Supply costs will be recurring. Capital expenses may be incurred if new equipment is needed (e.g., a procedure cart). Be inclusive to account for a comprehensive implementation approach that has a better likelihood of success.
Step 3: Estimate the ROI. This step entails subtracting the implementation cost from the estimated cost avoided. Even EBP improvements leading to marginal cost increases are likely to be beneficial over the long haul. Finally, link the outcomes to the organization’s mission and values.
Additional considerations. Costs or costs avoided should be reported strategically to garner executive support for EBP. Using a a scholarly process to demonstrate cost avoidance for your organization will make the advantage more objective and clearer to stakeholders.
The bottom line is that providing evidence-based care is the right thing to do, and evidence-based care costs lescs.
Read more about this topic in their book: Evidence-Based Practice in Action: Comprehensive Strategies, Tools, and Tips from the University of Iowa Hospitals and Clinics.





