How U.S. healthcare can play a larger role on the world stage

The invasion of Ukraine by Russia has commanded the attention of the world, and rightly so. The war and its resulting humanitarian crisis is not only a threat to global peace and security. It also adds to one more layer to the pressing problems plaguing many of the world’s populations, including escalating health inequity.
Health inequity, suffered especially by ‘those left furthest behind’ in low resource settings and fragile states, is high on the list of the world’s most urgent problems, but the war in Ukraine reminds us that the conditions that cause such inequities and desperate healthcare needs are not reserved for only underdeveloped countries, said Judy Kuriansky, PhD, adjunct professor, Department of Clinical Psychology, Teachers College of Columbia University, New York.
The need to “reach those furthest behind” who are “at the last mile” of health is a priority in the United Nations 2030 Agenda for Sustainable Development, explained Kuriansky, referring to the phrases which the U.N. uses in reference to efforts to make healthcare accessible to people most in need.
Kuriansky, also an NGO representative to United Nations and trustee of the United African Congress, hailed the efforts and commitment of those actively working to address the problem of lack of access to essential healthcare services in many parts of the world. Sadly, the pandemic arrested progress, leaving us with a long way to go to truly meet critical needs of underserved populations. But hope is still alive, Kurinasky said, noting that success depends in part on active engagement of the United States and stakeholders in the U.S. healthcare system, in multilateral partnership with the global community.
Q
Can you tell us about your involvement in addressing health inequity on the world stage?
Kuriansky
I wear a number of different hats related to shaping the future of global health and relevant to HFMA. One role is as member (and prior co-chair) of the Global Council on Health (SDG3 GC) of the “SDGs in Action” initiative of the United Arab Emirates [UAE] — a country that is a world leader in innovation — aimed at achieving the goals about good health, mental health and wellbeing of the United Nations 2030 Agenda.
The global councils are teams aligned with the 17 SDGs on the U.N. Agenda, which governments committed to achieve by 2030.These include SDG 1 (end poverty), SDG 4 (education for all), SDG 5 (empower women and girls), SDG 11 (make cities sustainable), SDG 16 (promote peace), and, of course, SDG 3 (good health and wellbeing for all).a
The global councils were mandated to come up with innovative initiatives to address the relevant SDGs.
For our SDG3 GC, I and my co-chair, Dr. Shariha Khalid Erichsen, a surgeon-entrepreneur, and team members, developed a platform on the internet, called Health in Your Hands, which showcases innovators around the world who are addressing health problems in order to reach those furthest behind, and create more partnerships that can “ upscale” their efforts (another commonly used U.N, development phrase). At one of the World Government Summits, our platform won the award for the most innovative project at that time.

Source: United African Congress/Hope and Health Vision. Used with permission.
Our team involves multi-stakeholders — which are always important for success — including representatives of diverse fields (U.N. agencies, academia, foundations). Recently the Minister of Health of the Republic of Sierra Leone joined, to represent government, essential to identify country needs, insure policy and partner in projects.
Our new GC3 co-chairs, distinguished global health leaders, are taking this forward. They are Dr. Mohammed Paté, former Nigerian health minister and global director of health, nutrition and population at the World Bank and now professor at the Harvard Chan School of Public Health, and Dr. Zsuzsanna Jakab, deputy director-general of the World Health Organization.
We also recently created a partnership between the Health in Your Hands platform and the Health Innovation Exchange platform led by Pradeep Kakkattil, director of innovation and partnerships at UNAIDS (a U.N. agency). In the COVID-19 recovery phase, we are focusing on hybrid innovations, which integrate technology with in-person community health outreach. The World Health Organization’s Global Strategy on Digital Health 2020-2025 outlines useful guidelines, to integrate financial, organizational, human and technological resources.b
Q
Can you describe how innovations get on the platform and give an example?
Kuriansky
Initiatives are vetted according to various criteria: Do they access people in need? Is there a viable business model to allow them to be sustainable? What is their capacity to expand to other regions and with other partnerships?
A good example is VillageReach, a nonprofit organization that reaches out to people in remote villages with limited health resources and distant from healthcare facilities in major cities. Their teams of community health workers assess people’s health needs and determine how that need can best be met.
This type of effort is extremely important now as a result of COVID-19, which exacerbated health needs, with more people who lack access and have become even poorer and more unable to afford any care. There also are fewer health force workers able to serve those people. Many programs had to adapt and pivot to carry out their work. We have to build resilient health systems and scale them up.
The solution is threefold: integrating technology, using the hybrid model that combines community outreach, and creating multistakeholder partnerships, especially with the private sector and government. In the case of VillageReach, while community workers go door to door to serve people where they live, their private-sector partner, called Swoop Aero, sends drones to fly over communities and collect medical data.
And governments play an essential role — their core countries being Malawi, Mozambique and the Democratic Republic of the Congo, which are countries with many people in need living in very remote communities. The multistakeholder partnership model makes it more possible to optimize the supply chain and implement the innovation to make the services available to those in very remote underserved communities.

Q
Is that something that can work here, in the United States?
Kuriansky
Yes. This is relevant to America because we have remote communities here, too. For example, Spanish-speaking farm workers in California have limited access to healthcare. Innovating ways to connect them to services, as on handheld devices, can be very useful. A technology platform like Proximie, with a U.S. office, uses machine learning and augmented reality to deploy tele-surgery to remote places. Also, having the U.S. government participate would allow programs like these to be funded to be sustainable.
Most of the innovations on the platforms I mentioned are in countries in Africa, India or other parts of the world. We need more of them that are U.S.-based.
Q
That makes me think of what’s happened recently with the omicron variant of COVID-19, which underscores the fact that this is a world problem. It seems to boil down to this point: If you don’t have health equity across the world, and if you don’t have the resources to help people address the impact of the coronavirus in their own areas of the world, then that problem eventually can come back to us in the United States. We can’t look at ourselves as being completely isolated. It seems we have gotten through omicron, but if we don’t address these problems on the world stage, we still leave ourselves open for potential future challenges.
Kuriansky
You’re exactly right. This is where the bridge can get made between what is being done in the United States and what we are doing on the international stage. The COVID-19 pandemic and its variants highlighted how the United States is not insulated from the rest of the world, since essentially, the whole playing field of health was leveled. This is an ongoing issue, where, as the United Nations Secretary-General António Gutteres emphasizes constantly, we must all work together in “multilateral” efforts to create universal health coverage and better health systems for our own population and that of other countries, since we are inter-related.
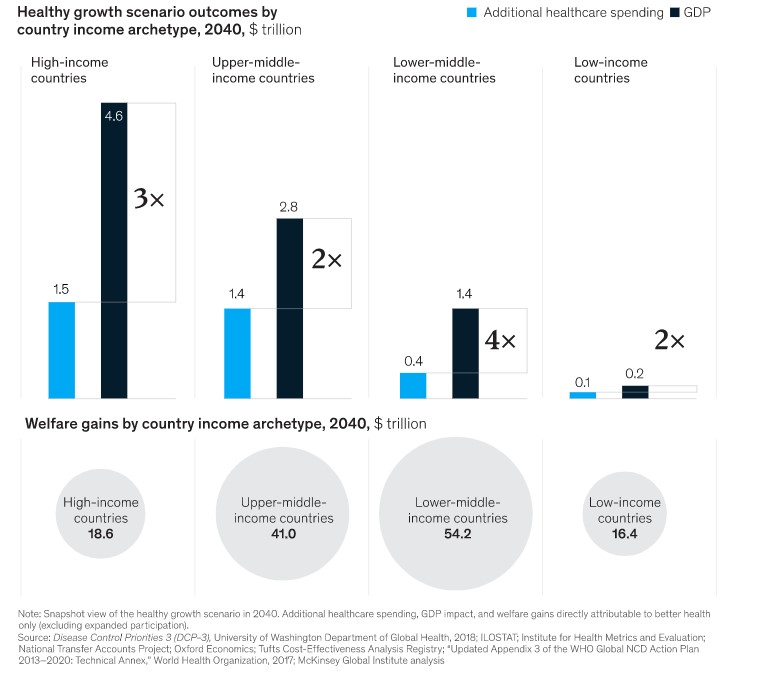
I’ve been at the United Nations representing NGOs for 18 years, and now well-being has been stepped up in the entire agenda of the U.N., so that the Secretary General has been really focused on multistakeholder partnerships and multilateralism to approach the serious healthcare gap, because none of us are alone in this — even though we have to take care of our own county, of course. Working together is SDG 17. All sectors must come together for joint solutions to health problems. Governments have to be open to working with NGOs, who need supportive policy, and funding, to do their work. Shockingly, less than 2% of national budgets are allotted to health, yet research shows across developing countries an economic return of between $2 to $4 for every $1 invested in health.c
Such multilateral cooperation is essential to achieve progress in recovery from the COVID-19 pandemic and to rebuild communities and societies better for the future.
For each $1 invested in improving health, an economic return of $2 to $4 is possible
Q
What is the takeaway from all of these activities for senior finance leaders of hospitals and health systems in the United States? What message do you have for them regarding how they could be involved in this effort and what they should be thinking about?
Kuriansky
I would like to see the United States more involved in initiatives we are talking about. I understand that U.S. health systems have to focus on their immediate financial challenges and sustainability, but we have populations in our country similarly marginalized and without health and mental health services that are affordable and accessible, especially as more migrants enter our country. U.S. health systems can benefit from adapting models being developed and implemented in other countries as on the platforms I mentioned, and even participating in multistakeholder partnerships being formed for developing countries. We also have a need to build more resilient health systems as we tackle the challenges of the long-term COVID-19 recovery period in health, including mental health, that we are facing.
I can imagine a forward-thinking hospital system leader who reads this and says, “I think I can benefit from such partnerships. I can build my own business with profits, as well as contribute to humanity and benefit collectively.”
I would like to see U.S. hospitals participating more with other countries. Take Africa. The First Lady of Sierra Leone, a friend, is rebuilding the military hospital from the ground up, as a state-of-the-art facility. I would like to see U.S. hospitals partnering there, with materials and training, from the start. I would like to see more projects like the one recently when a tanker exploded in the capital city of Freetown and hundreds of people were burned, but there are not burn doctors or skills in the country.

Fortunately, a team of burn physicians from Temple University was deployed, thanks to our relationship with a U.S. company, Global Response Management, which makes these connections. More of these interventions need to happen regularly, not just in emergencies, and be sustainable, not parachuting in and out. U.S. expertise can be sustainably contributed via e-medicine. Also, residency rotations, visas and accommodations need to be more institutionalized and promoted.
I will give you another example. In reaction to the COVID-19 epidemic, my UAC team partnered with local teams of physicians and health workers in an extremely remote community in the Democratic Republic of the Congo. To help stop the spread, we hired local women to make masks and taught the community health practices and psychosocial support techniques. It would be great to be “ready to go” with such interventions, and to keep such a project going, with e-trainings for local staff, funding and partnerships with U.S. hospitals. Hospitals in remote communities like that one desperately need American expertise, for clinical services and even for management and operating practices. Mutual benefits, to meet U.S. health systems’ needs, would be negotiated. It can be financially viable as well as socially responsible.
We have “sister cities.” Now we need “sister health systems.”
Editor’s note: See also the sidebars below for additional insight into activities aimed at improving health equity and mental health across the world.

Source: United African Congress/Hope and Health Vision. Used with permission
Footnotes
a. See Sustainable Development Goals Action Campaign, “18 Goals to transform the world,” and Global Councils, “Global Councils on SDGs 2018-2020 success stories,” Pages accessed March 25, 2022.
b. World Health Organization, Global strategy on digital health 2020-2025, 2021.
c. For a discussion of the economic benefits from investing in health in developing nations, see Remes, J., Wilson, M. and Randorai, A., “How investing in health has a significant economic payoff for developing economies,” Brookings, 2022.
About the United Nation’s work toward achieving SDG 3 good health and wellbeing for all
Since 2013, the United Nations has annually organized a High-Level Political Forum for countries to voluntarily report their progress toward achieving the Sustainable Development Goals outlined in the U.N. Agenda. The 2021 forum included an event that Dr. Judy Kuriansky co-organized, and moderated. The topic of this event was also discussed in our Q&A, which Kuriansky offered as an example of multistakeholder partnership.

Q
In July 2021, you moderated an online international event during the U.N. High-Level Political Forum, which I understand was sponsored by the Mission from Sierra Leone to the U.N., with many other U.N. Missions and organizations, stepping up to show commitment to the values of promoting health equity and mental health.a Can you give HFMA’s readers some insight into what that was about and what has happened as a result?
Kuriansky
Since 2013, the United Nations has annually organized a few-days meeting called the “High-Level Political Forum” for countries to voluntarily report their progress toward achieving the Sustainable Development Goals outlined in the U.N. Agenda. I co-organized and moderated an event for the 2020 Forum entitled “‘Building Back Better’ after COVID-19 through Addressing Health Equity, Mental Health, and Well-being: Contributions of Psychological Science and Practice to Leave No One Behind.”
It was an extremely impressive and historical that 17 governments from regions all around the world, with Sierra Leone as the lead sponsor, joined by Bahrain, Canada, Costa Rica, Ecuador, Iceland, Georgia, Japan, Lebanon, Mali, Nepal, Mexico, Portugal, Qatar,and Sweden – showing you the range of global national interest — as well as the World Health Organization and many NGOs. The presentations proved the importance of health equity as a critical concern in our COVID-19 recovery period, including, of course, equity in access to vaccines as well as in ongoing healthcare required for long-haul conditions.
The event was a perfect display of the importance of approaching healthcare from various dimensions, including government policy, scientific research and innovations. Projects in the field we showcased included the Health in Your Hands platform; iKure, which delivers primary healthcare to people across India; and the Transpersonal Psychosocial Organization Nepal, which partnered with the Nepali government to provide grief counseling and other modules for communities to cope with COVID-19.b
The important goal is to make connections among all these different stakeholders. Here’s some context for HFMA’s members to consider: In November of 2021, the World Health Organization had a three-day meeting to create a treaty among countries as to how they are going to approach the COVID-19 crisis.
That was followed in December by another three-day meeting in Geneva by the WHO, which was the 10th global health promotion conference. That intense meeting focused on wellbeing, bringing together the major stakeholders from the WHO, from the health sector, from the World Bank, from sectors all over the world — all the different regions and from governments and from academia — to discuss how are we going to move ahead with health promotion in this era of recovery.
Footnotes
a. “2021 Session of the High-level Political Forum on Sustainable Development (HLPF),” Moderator, Kuriansky, J., YouTube, July 13, 20.
b. High-Level Political Forum on Sustainable Development, “Concept note,” Page accessed March 25, 2022.
To come: An international perspective on the impacts of COVID-19
The widespread devastation caused by the COVID-19 pandemic has prompted an intensified worldwide focus on prioritizing health equity and mental health and the rapid adoption of digital health tools to complement in-person community outreach. Such efforts are bringing about changes in healthcare, especially in reaching people in remote parts of the world where healthcare systems are fragile, infrastructure is weak and populations are underserved but direly in need.
These and related issues are addressed in a forthcoming book aimed at raising awareness of what is happening and what is possible for the future, which is slated to be published in October 2022 by Elsevier in 2022: Resilient Health: Leveraging Technology and Social Innovations to Transform Healthcare for COVID-19 Recovery and Beyond.
Chapters by noted health experts in the world, (e.g., from WHO, Harvard, the World Bank and other organizations) address the current state of the world in health, the role of varied stakeholders, financing models and various technologies (e.g., artificial intelligence, augmented reality). Innovations are described that hold promise to accelerate achievement of the United Nations Agenda goals of good health and mental health for all – a human right – and Universal Health Coverage.





