The Vitalic Health movement: HFMA initiative pursues affordability, financial sustainability in U.S. healthcare
As demand grows to address healthcare’s biggest challenges, Vitalic Health jumpstarts collaborative solutions for change.

PHOTO ILLUSTRATION BASED ON PHOTOS BY MARSHALL CLARKE
Growing up in rural Iowa, miles away from a paved road, instilled in C. Ann Jordan a deep appreciation of the struggles rural communities face around healthcare access, delivery and affordability.
The farming community of Boone, Iowa — Jordan’s hometown — features a 25-bed critical access hospital. The hospital offers a range of services that aren’t always available in rural facilities, from family birthing to hyperbaric oxygen therapy for wound care to pain management. Given that more than a quarter of Iowa hospitals eliminated obstetrics units from 2010 to 2022, the availability of maternity services alone distinguishes the hospital among rural facilities.a
But when residents face complex health issues like cancer, heart disease or mental health challenges, they typically must travel to another county for specialized care. It’s the type of scenario that HFMA President and CEO Jordan, JD, thinks of when she considers the depth of the challenges facing U.S. healthcare and their impact on access to care, affordability of care, care decision-making and health outcomes.
“There are some things that you learn best in calm and others in storm, as the novelist Willa Cather once said,” Jordan said. “That’s very true to rural America. That’s very true to healthcare right now. It is having to learn in the storm.
“If you look at small communities and rural communities in general, their entire mentality and unique fortitude is based on the concept of doing more with less.
“Stakeholders in these communities must collaborate to solve problems like, ‘How do you make healthcare work when you have a smaller population and workforce base than large metropolitan areas?’ The mentality of solve-based convening is very prominent in those situations.”
The concept of solve-based convening holds strong appeal for Jordan, who brings extensive experience in systems design to her role in leading HFMA. Jordan says she is passionate about the science and discipline of quality assurance and enterprise risk management and their connection to sustainable systems. In her view, the extent to which organizations and industries excel in these areas influences both performance and trust.

It’s one reason she was drawn to HFMA — and why she’s compelled to advance solve-based convening in healthcare through Vitalic Health. The initiative is designed to move the needle on healthcare affordability and health outcomes by bringing together diverse stakeholders to work toward meaningful action.
“If you’re a systems design expert, this is the ultimate problem-solving opportunity for good to impact lives,” Jordan said. “Vitalic Health is not about improving performance metrics. It’s about aligning competing stakeholders around a shared commitment toward affordability, access and wellness to ensure the vitality of our communities.
“Through the lens of system design and solve-based convening, we can collectively find ways to eliminate fragmentation and variability, which threaten outcomes, increase costs and erode public trust.”
Uniting multi-stakeholder groups for transformative change
Vitalic Health, powered by HFMA, is designed to lead stakeholders toward revolutionary payment models and business practices that rein in healthcare expenditure growth while increasing Americans’ health span. Its goal: to achieve a more financially sustainable and affordable system that drives healthier lives.
Affordability of care and concerns around the ROI of the healthcare dollar have become major sources of frustration for purchasers of all types, from consumers to employers to health plans.
“We’re not delivering on the promise of health or healthcare outcomes at a sustainable cost,” said Susan Dentzer, MS, president and CEO of America’s Physician Groups.
Today, administrative complexity is “the single biggest component of excess U.S. spending,” according to The Commonwealth Fund, a private foundation focused on promoting a high-performing, equitable healthcare system.b An analysis by Strata Decision Technology estimates that administrative complexity alone contributes to more than 40% of the total costs hospitals incur delivering care.c
Meanwhile, as consumers shoulder increasing responsibility for the costs of their care, concerns about affordability factor into their decisions about whether to seek care. A Gallup poll found one in 10 American adults have been unable to access or afford healthcare in the past year.d This proportion is even higher among black and Hispanic adults surveyed (14% and 18%, respectively), as well as among adults with a household income of $90,000 or less. Across the board, these numbers are climbing year over year.
“We all have to recognize that affordability of care is an imperative, and it’s an imperative that everybody has to have ownership in,” said Robin Damschroder, FACHE, president of value-based enterprise and CFO for Henry Ford Health, based in Detroit.

Breakdowns in care coordination, care delivery and care management also plague the U.S. healthcare system as we know it, resulting in fragmented care experiences that frustrate consumers, add unnecessary expense and result in poor outcomes and care complications. These are scenarios that further erode relationships with consumers as well as employers, health plans and even clinicians, with 45% of frontline clinicians saying they don’t trust their organization’s leaders to do right by patients.e
“One of the main issues that we have to confront as a healthcare industry is that our systems around care delivery are predominantly not designed around the needs of a patient or a consumer,” said Deepak Sadagopan, value-based platform business lead for Risant Health, a nonprofit organization based in Washington, D.C., that works to accelerate adoption of value-based care.
In a non-patient-centered system, access to primary care and specialty care becomes harder to achieve, Sadagopan said. While there are examples of entities that do this well — such as accountable care organizations and clinically integrated networks that broaden multimodal access to primary care — the need for a model that is more affordable and sensitive to the needs of the whole population remains strong.
“It will take multi-stakeholder collaboration, especially as we move into multi-payer, multi-provider types of markets, to make such a design possible,” he said.
Until then, the strain of navigating a healthcare system that feels designed without the consumer in mind will continue to weigh on patients, widening the gaps in care between healthcare’s “haves” and “have-nots” described in the Gallup study.
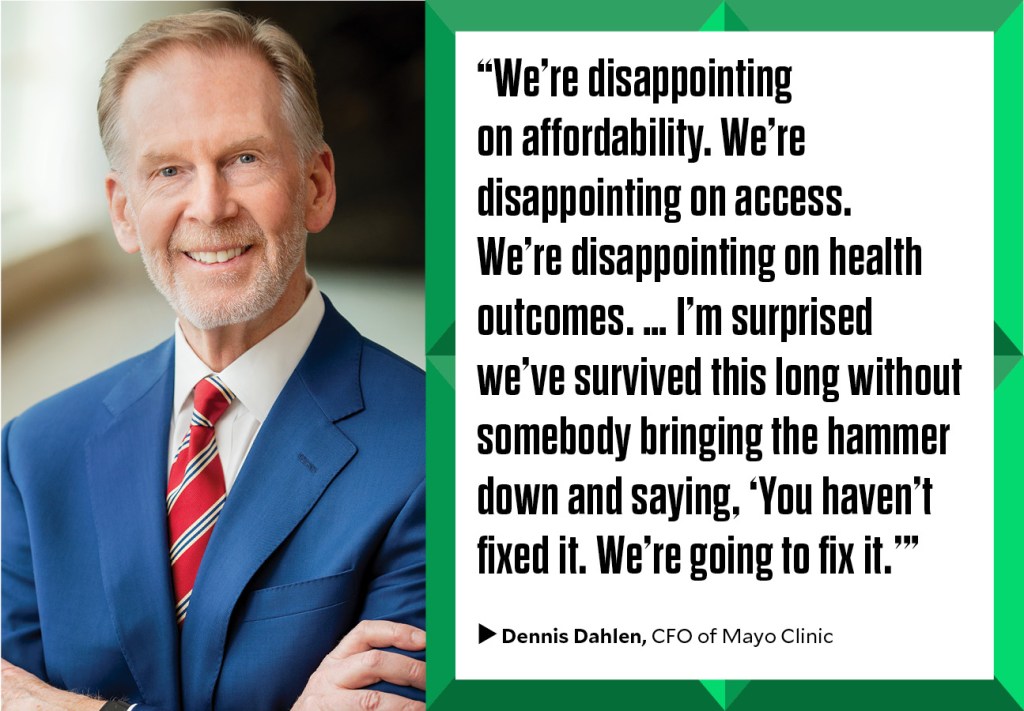
“We’re disappointing on affordability. We’re disappointing on access. We’re disappointing on health outcomes,” said Dennis Dahlen, CFO, Mayo Clinic. “No industry can survive that for too long. I’m surprised we’ve survived this long without somebody bringing the hammer down and saying, ‘You haven’t fixed it. We’re going to fix it.’”
Now, the healthcare industry is at a tipping point that demands that stakeholders come together to create a healthcare system that is more affordable, more equitable, more sustainable and more human.
“If the industry does not collaboratively convene and intentionally solve these problems, then the government will do so in a very clumsy way,” said Marcus Whitney, CHFP, founding partner of Jumpstart Health Investors, a healthcare venture capital firm focused on early-stage investments.
It’s an environment where aspirational talk about how to chart a better course for U.S. healthcare is no longer enough, Jordan said. Vitalic Health’s approach to solve-based convening — emphasizing the need for a multi-stakeholder fix — both acknowledges the complexity of the systems behind U.S. healthcare and seeks to optimize them.
Said Dahlen: “Ideally, it will allow us to use what we’ve been taught and what we know about the way the system works, and what we know is suboptimal or worse in healthcare, and say, ‘How might we fix that? What might a better design look like, and what’s the path from here to there?’”
At its core, Vitalic Health will address what David Johnson, CEO of 4Sight Health and an HFMA author, calls “a reverse tragedy of the commons in healthcare.”
To describe this idea, Johnson said: “Our very public good is investing in pro-health activities. When we do it, it generates a huge return for society. But providers don’t do it because when they invest in pro-health activities, they lose volume, they lose money. And payers don’t do it because when they invest in pro-health activities, their premiums go up, and their members switch plans.
“We need to come up with payment models and metrics that enable both payers and providers to invest in pro-health activities to specifically address this reverse tragedy of the commons problem we all live with,” he said.

A movement toward collective innovation
Since the December 2024 murder of UnitedHealthcare CEO Brian Thompson, who grew up in a community not far from Jordan and her brothers, Jordan has seen more diverse stakeholders advocate for change in healthcare.
Innovations around population health management, value-based care and payment model transformation — areas where such divergent views existed that some stakeholders were waiting to see which ideas would stick before making a move — are now accelerating, backed by health plans and federal resources and dollars. One recent example: the Rural Health Transformation Program, where states may use funds in part to develop projects that test innovation around value-based care and payment.
“To see unity around payment model transformation, I think that’s a big win,” Jordan said. “That means there’s common ground to discuss things.”
Through Vitalic Health, Jordan envisions a bold, constructive space where healthcare is “no longer a fragmented battleground of conflicted stakeholders, but rather a mosaic that is diverse by design and united in purpose.
“The reality is that no single stakeholder can solve the challenges of affordability, care delivery and quality outcomes,” Jordan said. “No one stakeholder can bend the curve. This needs to be a united effort, and that starts with a collective mindset for change.”
In 2025, Vitalic Health worked to advance its first output with the development of the first measurement tool for grading the healthcare industry’s performance based on affordability, financial sustainability and health outcomes.
Known as the “U.S. Healthcare Vitals Tracker,” the tool leverages 25 universally accepted metrics in examining the state of healthcare affordability and the health span of the American population. The Vitals Tracker scores affordability and health span dating back to 1997, the last year of a federal budget surplus.
Jordan describes the Vitals Tracker as “a single source of truth that will tell us the state of healthcare affordability and outcomes in this country.”
“We have the largest economy in the world, and we’re spending trillions of dollars on healthcare, yet there had never been an effort at the macro scale to measure and understand the components of the U.S. healthcare system economically, year over year, to state, ‘Are we getting better or worse, and why? What does all this mean?’” Jordan said.
Having spent most of her career outside healthcare, she found this reality surprising.
“That was eye-opening to say the United States healthcare industry did not have a measurement or index device to grade its own performance,” Jordan said. “We wanted not only to inform this national dialogue on healthcare affordability and sustainability that very much needed to occur, but also to monitor whether the U.S. healthcare system was meeting present and future demands for care. From there, we would take those learnings to build solutions for the future.”
Released for public comment in fall 2025 and shaped based on industry feedback, the Vitals Tracker found the healthcare industry is in a state of “serious condition.” Year over year, affordability has declined while health outcomes have remained stagnant, despite continual investments in innovations meant to strengthen efficiency and quality of care.
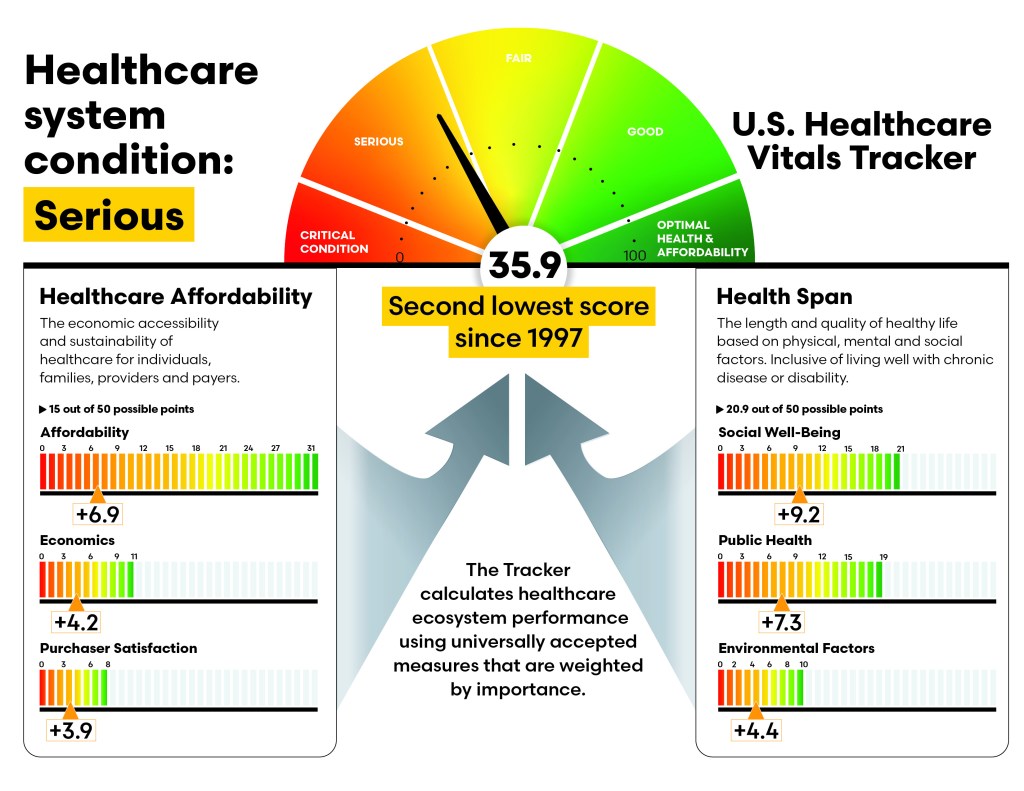
“One thing for me that was very enlightening is when you step back and you look at all the emotion and division that has occurred because of healthcare policy, there has not been a policy that has truly moved the needle on healthcare affordability, sustainability and health outcomes in a meaningful way,” she said. “As we look to build solutions for the future, we need to ask ourselves, ‘What are the lessons that can be learned from that?’”
Zeev Neuwirth, MD, a long-time physician executive and author, views the Vitals Tracker as a tool for bringing organizations and stakeholders together to collaboratively generate solutions.
“It would be one thing to put out another report on the state of healthcare. It’s something different to actually say, ‘This is just a measuring stick for the state of healthcare. The real work is in convening to solve these issues,’” he said.

Neuwirth says he believes true transformation in healthcare will start at the business model level, examining how the existing model impacts healthcare operations and how operations could be adapted to new business models.
For Damschroder of Henry Ford Health, the value of the Vitals Tracker comes from its ability to effectively draw connections between healthcare cost, quality and affordability. From there, conversations can focus on the need to attain greater value from healthcare investments.
“My hope is that it will be used not as a mechanism to blame people, but to urgently try to gather people across the industry to help solve these problems together,” Damschroder said.
The national release of the Vitals Tracker is set for January 2026. Other Vitalic Health initiatives designed to address the industry’s most complex challenges include:
- Impact Measurement Institute: The Vitals Tracker is its first output
- Swarm Studies: Will bring together diverse stakeholders to explore new solutions for pressing issues
- The Payment Model Consortium: Will seek innovative payment models to test and scale
- The Solutions Studio: Will focus on developing transformational products and services
In a multibillion-dollar, complex system, the success of Vitalic Health will ultimately be measured by the extent to which Americans spend less of their income on healthcare while living longer, healthier lives, said Lisa Eyer, vice president, healthcare market strategy and innovation for HFMA, who was hired to oversee the Vitalic Health Initiative.
That’s a state she hopes to see in the next decade.
“In the near term, success means the U.S. Healthcare Vitals Tracker becomes the standard reference for healthcare system performance — cited in policy debates, earnings calls and board meetings,” Eyer said. “Success means our first swarm studies produce validated interventions that providers and payers actually adopt, not just read about. And success means our payment model consortium proposes at least two concrete changes to payment models that get piloted by major health systems or payers.”
The advantage Vitalic Health brings to the healthcare ecosystem is that it provides a safe space for disruptive thinking outside traditional healthcare organizations, according to Whitney of Jumpstart Health Investors.
Whitney compares the type of disruption likely to be stimulated by Vitalic Health to the approach Jeff Bezos took in giving team members the space to create the Kindle. Bezos knew the Kindle would disrupt the core business of Amazon — shipments of physical books — and so he sent the team charged with designing the Kindle to a location away from Amazon’s core facility.

Traditional healthcare organizations “are in no shape to really innovate within themselves. They’re just not. There’s no track record that proves it,” Whitney said. “Initiatives like Vitalic Health offer a safe space for brave leaders to put some of their smartest people in a room with some of the other smartest people in the industry to get something done that Amazon could never get done within their four walls because their culture just would not support it. And that’s no knock on their culture. It’s just the reality of how organizations that scale work.”
One factor Vitalic Health has in its favor is that there’s a growing appetite for collaboration among healthcare stakeholders, Neuwirth said. He says he believes HFMA is uniquely positioned to convene stakeholders to uncover practical solutions for addressing financial sustainability and better health outcomes.
“It’s a national organization, and it’s not limited to one type of stakeholder in the system because of its financial roots and core,” he said. “That lends a reality base to this effort that I think is vital.”
Navigating a path forward for sustainability
The challenges facing the healthcare industry are daunting, but change is inevitable, Jordan said. She believes the vitality of American communities depends on collaborative, solve-based convening to deliver reliable and sustainable solutions.
“There is a growing public sentiment to see all of us in healthcare do better,” she said. “There’s a movement toward wanting to get behind solve-based convening for improved affordability and outcomes. And I think there’s opportunity here.”
Footnotes
a. McDill, V., “Hospital-based obstetric care declines across US, hitting rural states hardest,” University of Minnesota School of Public Health, July 7, 2025.
b. Turner, A., Miller, G., and Lowry, E., “High U.S. health care spending: Where is it all going?” The Commonwealth Fund, Oct. 4, 2023.
c. “Skyrocketing hospital administrative costs, burdensome commercial insurer policies impacting patient care,” American Hospital Association, September 2024.
d. Witters, D., and Maese, E., “In U.S., inability to pay for care, medicine hits new high,” Gallup, April 1, 2025.
e. Janisch, A., Gerhardt, W., and Shukla, M., “2025 U.S. health care outlook,” Deloitte, Dec. 12, 2024.





