Why PAC discharge choices are key to success under risk-based payments
Two health systems with well-developed and well-executed post-acute care (PAC) strategies share key insight on how they ensure patients are discharged to the appropriate PAC setting.
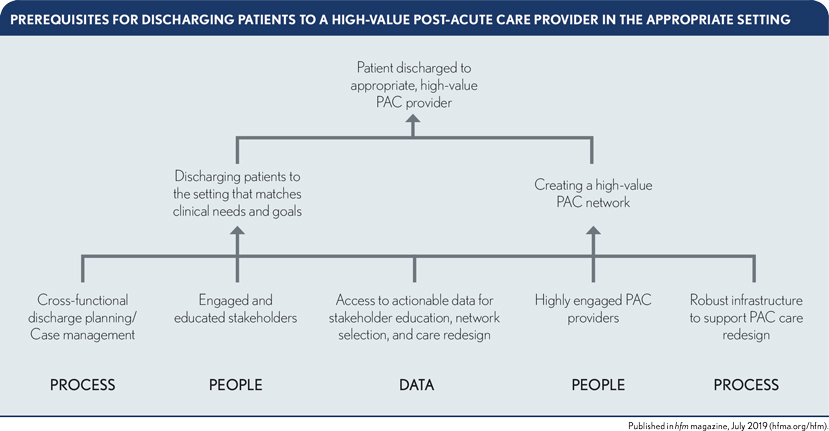
Managing spending on post-acute care (PAC) effectively is a critical success factor in risk-based payment models. Such efforts have the potential to yield substantial improvements in outcomes while reducing the total cost of care under risk contracts. Successfully managing PAC spending requires that provider organizations have the capability to consistently discharge every patient to the high-value PAC setting identified as being most appropriate based on the patient’s clinical need and goals. As shown in the exhibit below, there are important prerequisites to building this capability.
Based on the experiences of health systems such as LifePoint Health, headquartered in Brentwood, Tenn., and Lovelace Health System in Albuquerque, N.M., which have developed effective PAC strategies, addressing these prerequisites requires a focus on three areas in particular:
- The discharge planning process
- Stakeholder engagement
- Data and tools to promote stakeholder awareness
Cross-functional discharge planning and case management
Not surprisingly, expanding the scope of who is involved in discharge planning is a common element in the strategies progressive organizations use to ensure the patient is discharged to the appropriate setting. Because this step represents a cultural change for many organizations, it should be supported with clear, consistent communication.
LifePoint uses daily interdisciplinary team rounds to plan all medical and surgical discharges. The rounds bring together hospitalists (or surgeons), other primary care physicians, nurses, clinical documentation improvement (CDI) specialists, physical therapists, pharmacists and others at the bedside to determine the appropriate PAC setting.
Chris Frost, MD, national medical director of hospital-based providers for LifePoint, stresses the need to hardwire this process for consistency, stating that it needs to become a “sacred part of the day.”
Beyond assessing the patient’s clinical condition, this decision-making process needs to consider the patient’s immediate and long-term goals of care and home environment and identify any adverse social determinants of health (SDOH) that might affect the patient.
Involvement of case managers in these discussions is essential for ensuring continuity as the patient moves across the care continuum. The case managers have a granular understanding of the patient’s preferences and clinical situation, resulting from multiple interactions with the care team and family over the course of the hospital stay. Although LifePoint, like many organizations, has a rubric in many of its facilities that helps guide site selection based on a patient’s clinical condition, the case managers often override this recommendation based on their more direct knowledge to help ensure the optimal initial PAC site is selected.
An underappreciated aspect of the team-based discharge planning process is the need to have an operational understanding of each PAC partners’ capabilities (discussed in detail in part two of this series). For example, within a market, different home health agencies can have widely different capabilities for taking complex patients. A home health agency that has a strong community case management capability (e.g., employs in-home social workers and has deep relationships with local community service providers), for instance, can present a viable alternative to a SNF for patients who have adverse SDOH, allowing the patients to be safely discharged to their homes — the preferred setting — with the necessary incremental support. Yet if the discharge planning team lacks a granular understanding of PAC partners’ capabilities, patients will continue to be discharged to higher-level settings of care than are clinically necessary.
Engaged and educated stakeholders
Developing an effective PAC discharge planning team requires not only expanding the types of stakeholders involved but also effectively engaging them. Different approaches for engagement are required for different stakeholders, depending on their roles.
Patients and caregivers. Historically, patients have been engaged in the selection of PAC sites only at the very end of their stays. Typically, case managers would give patients and their caregivers a list of PAC providers and leave the room. And in some cases, the recommendations may have come as a surprise to the patient, often resulting in suboptimal choice of PAC provider and a dissatisfied patient. providers’ assumptions that most patients do not want to be discharged home.
Second, health system management teams are emphasizing that patients should go the most clinically appropriate PAC setting, not the first available discharge setting for which patients are qualified based on their conditions.
Third, progressive health systems are providing care teams with cost and quality data to help them understand the financial implications of referral decisions on both episode outcomes and costs and to reassure them that patients are benefiting from high-value care post discharge.
Finally, these health systems are setting the expectation that hospitalists and surgeons, including community physicians with privileges in the organizations’ hospitals, provide informed, meaningful advice to help patients select PAC settings.
Internal compliance and legal representatives. The Centers for Medicare & Medicaid Services (CMS) has historically prohibited hospitals from recommending PAC providers to their Medicare patients. CMS now allows providers participating in certain APMs to provide data on PAC providers that beneficiaries can use to identify high-value sites of service. Further, CMS suggested in a 2015 proposed rule that it may become a condition of participation in Medicare for providers to furnish Medicare beneficiaries with information that will help them make “informed decisions about their post-acute care.”a This policy is expected to be finalized this year. However, many organization participating in qualifying alternative payment models have been slow to embrace this opportunity due to concerns of their compliance and legal staff. (See the sidebar.)
Organizations that are actively engaging patients to ensure they receive their PAC services from high-value providers have addressed compliance and legal team concerns by incorporating members of the team into the care-redesign process. This measure helps them understand the steps the care team takes to understand patients’ goals as well as educate and provide data to patients to help them make informed decisions. Once compliance and legal staff understand that, in every step, communications among staff, physicians and patients are hardwired to facilitate wellinformed patient choice, they become comfortable with process.
Owned PAC assets. Health system leadership should commit to ensuring that patients are discharged to the most clinically appropriatesetting of care by setting the expectation that if a patient needs to go to a SNF, that’s what will happen. Inpatient rehabilitation facilities and long-term acute care hospitals should accept only those patients that require that level of care. To these ends, PAC providers should prepare for volume shifts among varying provider types because referral patterns may change, potentially affecting staffing levels, financial budgets, capital planning and competitive strategy.
Access to data to support stakeholder education
Both LifePoint and Lovelace regard sharing quantitative data with providers in a clear, compelling way as foundational to success. And both share scorecards monthly with hospitalists, proceduralists, clinicians, discharge planners and health system administrators. They both also recognize that being able to monitor the performance of patients discharged to the PAC network helps identify opportunities for care improvement and reinforces desired care patterns.
Physicians say they value this information because it informs their recommendations regarding the best PAC providers for patients and enables them to explain to patients why the recommended PAC providers present the best options..
Although monthly PAC scorecards diff er in many ways, they do have common elements, including:
- Case counts by episode
- Episode-specifi c discharge location compared with the national average or by provider peer group
- Readmission and infection rates for each facility
- Estimated net payment reconciliation amount for each episode compared with target
To supplement the monthly dashboard, the health systems furnish discharge planners with PACprovider lists that identify participants in the high-value network. They also provide scripting to enable the discharge planners to explain how providers are selected to participate in the network, why a specifi c PAC setting was chosen for a patient and to help answer patients’ questions.
PAC discharge planning fits into a larger strategic picture
Taking steps to ensure patients are discharged to the most appropriate PAC setting is a fundamental part of developing an eff ective PAC strategy. Another essential part of the strategy is the ongoing task of creating and managing a high-value PAC network, a topic to be addressed in the August 2019 issue of hfm.
Footnotes
a. CMS, “Medicare and Medicaid Programs; revisions to requirements for discharge planning for hospitals, critical access hospitals, and home health agencies,” Federal Register, Nov. 3, 2015.
Acknowledgements
The author would like to thank the following individuals for their generous contributions of time and insights that were instrumental in developing this series:
- Chris Frost, MD, national medical director of hospital-based providers, LifePoint Health, Brentwood, Tenn.
- Devin Griffith, vice president of regional development, Advanced Home Care, Greensboro, N.C.
- Craig Tolbert, principal, DHG Healthcare, Birmingham, Ala.
- Gary Whittington, CFO, Lovelace Health System, Albuquerque, N.M.
- Michael Wolford, senior manager, DHG Healthcare, Cleveland





