A report from HFMA’s 14th annual Thought Leadership Retreat
Download the PDF of the report
Even amid the COVID-19 pandemic and other urgent day-to-day concerns, the need for healthcare stakeholders to think in terms of cost effectiveness of health (CEoH) is becoming increasingly obvious. To begin developing a road map, HFMA’s virtual 2021 Thought Leadership Retreat examined the importance of addressing CEoH and explored applicable strategies.
Achieving better CEoH can be considered the industry’s overarching long-term challenge. After all, the U.S. in 2019 spent $3,800 more on healthcare per capita than any other OECD country yet settles for worse results: An August 2021 report by The Commonwealth Fund placed the U.S. last among 11 comparable countries in healthcare system performance.
In other words, the healthcare dollar in this country does not bring an optimal return. And solutions need to be more comprehensive than efforts to bend the cost curve.
“It’s not about trying to squeeze out whatever we can from the existing system,” said HFMA President and CEO Joseph J. Fifer, FHFMA, CPA. “It’s about changing incentives to change how the system works.”

Joseph J. Fifer, president and CEO, HFMA
That was among the many CEoH concepts discussed at the Thought Leadership Retreat. Sponsored by AbbVie, Inc., AKASA, Humana and Lumere, a GHX company, the Sept. 30-Oct. 1 event brought together executives from across healthcare. In addition, three follow-up webinars in October featured insights from physician, nurse and health plan leaders.
As stakeholders consider how they can start to tackle CEoH, this report presents 10 foundational approaches that were discussed.
1. Focusing on Health, not Healthcare
Improving the delivery of healthcare is not the ultimate goal of a CEoH strategy because it takes a narrow view of consumers’ well-being.
“If we said healthcare, that would be suggesting that we would organize around ourselves in the industry,” Fifer said. “To organize around health, we have to organize around the consumer.”
Healthcare by definition is “illness-based and illness-focused,” said Peter Angood, MD, the CEO and president of the American Association for Physician Leadership. A better clinical model supports patients’ “true health.”
Peter Angood, MD, CEO and president, American Association for Physician Leadership
“We’re talking care, but we’re also talking health,” added Robyn Begley, DNP, RN, the CEO of the American Organization for Nursing Leadership (AONL).
Such an objective requires incorporating roles that aren’t traditional to healthcare. Begley cited a demonstration project at Chicago’s Sinai Urban Health Institute, which sought a better way to care for patients with asthma. “A really key component of that is the community health worker,” she said. “Their outcomes were incredible.”
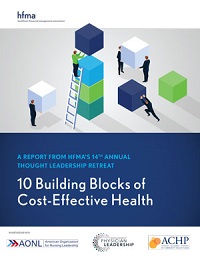
How should the U.S. healthcare system change expenditures for disease treatment vs. preventive health?
Source: 2021 Thought Leadership Retreat attendee poll
2. Gaining Consumers’ Trust
In polling and discussions among Thought Leadership Retreat attendees, a recurring theme was that efforts to make health more cost-effective can’t work unless patients are on board. However, patients are unlikely to play their part if they don’t trust their providers.
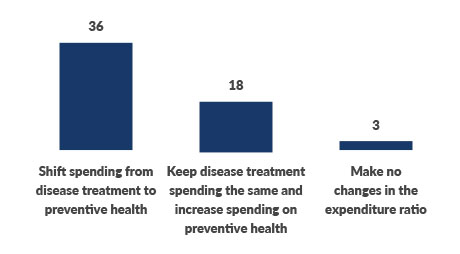
Who is in the best position to drive big shifts toward more cost-effective health?
Source: 2021 Thought Leadership Retreat attendee poll
During the pandemic, for example, a lack of trust among segments of the population has been blamed for holding down vaccination rates. “Many of the consumers in our country don’t trust us as a formal health system, any part of it,” Fifer said. “And in fact, it’s part of a societal [trend] — people don’t trust any system these days.”
The most obvious — yet daunting — way for stakeholders to solidify consumer trust is to make the system work better. Zeev Neuwirth, MD, a physician executive, author and podcast host, noted that cutting-edge healthcare companies bring a “marketing mindset” to their business and operational models.

Zeev Neuwirth, MD, physician executive, author and podcast host
“By marketing, I don’t mean public relations or sales or advertising,” Neuwirth said. “I mean the essence of what marketing is about, which is understanding who your customers are, understanding what your customers need and want and delivering it to them.”
3. Measuring What Matters
To boost CEoH, quality measurement needs to go beyond episodic acute care to incorporate every setting in which healthcare is delivered. It needs to evaluate access, such as whether primary care physicians are available after hours, which can keep patients out of the emergency department.
Providers also need to incorporate processes and expertise to translate data analytics into practical information that drives clinical and operational changes.
“We’re making some improvement in that area, but I think we need to speed up the actionable intelligence that comes out,” said Ash Gokli, MD, chief clinical operations integration officer with Sutter Health.
A key question is how to incorporate data insights into encounters with patients. Anna Kiger, DNP, MBA, RN, system chief nurse officer with Sutter, described an initiative to use the organization’s electronic health record and smartphone app at the point of care to gather information on social determinants of health (SDoH).
The information is taken during a patient’s introduction to the health system and is compiled using a standardized data collection tool by an individual in a population health role. The data both aids in developing individual care plans and contributes to population-level insights.
4. Aligning Payment Systems
The bold moves needed to make health more cost-effective can’t be undertaken unless sufficient financing is in place. And that requires changes to the U.S. healthcare payment system.
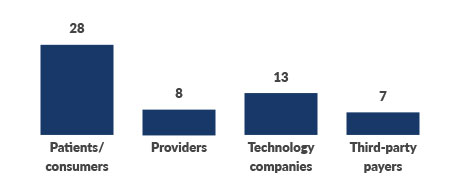
That concept was emphasized in polling at the Thought Leadership Retreat, with more than half of respondents choosing alignment of payment incentives as the most important first step in addressing CEoH.
Source: 2021 Thought Leadership Retreat attendee poll
Neuwirth bluntly criticized the fee-for-service payment system during his presentation, saying it has “decimated the primary care system in our country” and forced hospitals to serve as the de facto public health system during the pandemic.
Successful provider-sponsored health plans illustrate the benefits to be gained by better linking financing with population health management. Gordon Edwards, CFO of Marshfield Clinic, which owns Security Health Plan, pointed out that the insurance side of his organization helps guide care delivery strategy.
“We are so much stronger because of our health plan,” Edwards said. But for patients who aren’t enrolled, he added, “I can’t take all those strategies and apply them because the economic incentives aren’t there.”
Fifer challenged attendees to make sure alignment efforts also account for what would put consumers in position to drive shifts toward more cost-effective health.
5. Developing an SDoH Strategy
Stakeholders need to evaluate their spending priorities when seeking to improve CEoH. For example, healthcare represents 90% of national health expenditures even though it accounts for only 20% of the factors that contribute to health, Fifer noted. Meanwhile, social, environmental and behavioral issues determine 60% of a person’s health profile yet draw only 9% of spending.
The Biden administration hopes to use the federal government’s purchasing power to start flipping the script, said Elizabeth Fowler, PhD, JD, deputy administrator for CMS and director of the Center for Medicare & Medicaid Innovation (CMMI).
“We want to encourage more transformation in behavioral health, social determinants of health and person-centered care,” Fowler said. Advancement in those areas will require CMMI to provide more real-time data to support clinical decision-making and payment waivers to increase flexibility, she added.

Elizabeth Fowler, PhD, JD, deputy administrator, CMS
The traditional concept of an ROI won’t apply as stakeholders work to address SDoH, said Connie Hwang, MD, MPH, chief medical officer and director of clinical innovation with the Alliance of Community Health Plans. “That’s a really hard thing to say, ‘Wow, we did this, and X results and dollars came through,’” she said. Instead, such initiatives are “really about the long play.”
6. Bolstering the Workforce
Addressing administrative burden is one way to both promote cost-effective health and support a healthcare workforce that is reeling from the pandemic. Such steps also are necessary to ensure clinicians and staff have the bandwidth to focus on key elements of CEoH, such as preventive healthcare and social determinants, Fifer said.
The end of the pandemic — whenever that comes — won’t solve the workforce issues. Begley noted that in a recent AONL survey of nurse leaders, 90% said the ongoing challenges would linger. Nursing shortages especially could prove detrimental in upcoming years given an aging population and the increasing prevalence of chronic conditions.
Sweeping changes thus may be required, perhaps even to the basic model of nursing care.

Robyn Begley, DNP, RN, CEO, American Organization for Nursing Leadership
“What is the interprofessional model of care that supports not only our inpatients, but also [patients] throughout the continuum? That’s challenging,” Begley said. “There are a lot of connections that we have to make, but that’s really the future.”
7. Customizing Care Delivery
Although population health management makes sense as an operational model for improving CEoH, generalized care delivery isn’t conducive to improving patient engagement and reducing inequity.
Primary care especially is ripe for disruption, with companies concentrating on segments such as seniors or women or on specific conditions. For example, ChenMed focuses exclusively on caring for seniors with complex chronic conditions. “They hire doctors who love this — that’s all they want to do,” Neuwirth said. “They hire nurses and coaches that want to take care of older, sicker patients. They give them specialized training just in this type of patient care modality.
“Then they don’t say, ‘You’re going to take care of 2,000 patients.’ You take care of 400 to 500 patients. And these patients become like your family, and you are with them 24/7,” Neuwirth added. Patient satisfaction and outcomes such as hospital admissions are significantly better in such models, he said, and costs are lower.
Takeaways from Attendees
Breakout discussions involving attendees, whose roles span administrative and clinical leadership positions with providers and health plans, are an annual staple of HFMA’s Thought Leadership Retreat. Here’s a small sampling of the insights that came out of the discussions on the cost effectiveness of health.
On health and healthcare: For the first time, the public isn’t using medical science as the source of truth, instead looking to alternative sources and facts. Healthcare leaders need to own the loss of credibility and work to repair the issue in their communities.
On the cost of health: The current intent of cost-cutting efforts is to increase margin, not necessarily to lower the cost of care. Having AI just makes it easier to perform the same old tasks, not innovate in the delivery of care or the structure in which it is delivered.
On patients: Offering patients access to pricing data can only do so much given the financial interrelationships between clinicians, hospitals and insurers. Creating incentives for both patients and hospitals to affect social determinants has largely proved elusive.
On the workforce: It’s difficult to discuss cost effectiveness before addressing the nursing crisis. Disruption of the nursing business model needs to be considered within provider organizations.
On aligning incentives: Reducing costs and passing the savings on to consumers is unlikely, at least until alternative payment models actually reduce burden and patients are incentivized to take responsibility for their health.
8. Improving Chronic Disease Management
Even when it’s not the subject of a specialized care model such as the one Neuwirth described, chronic disease management is necessarily a focal point of a CEoH strategy. Although the first goal is to keep patients healthy, those with conditions such as diabetes or COPD still can avoid the need for high-cost acute care and have a better quality of life.
Kiger described a pilot program at Sutter Health to help patients 60 and older with chronic disease thrive outside the healthcare setting. “We talk to them through technology — a lot more health coaching, a lot more care coordination, a lot more checking in with them on a frequent basis, keeping them and their caregiver educated on what they need to do to maintain health,” she said.
Based on results, Sutter plans to expand the program by up to 50 practices over three years. “It’s a cheaper alternative to achieving the health that the patient would like to achieve,” Kiger said.
9. Leveraging Digital Health
Because CEoH depends on helping patients stay healthy without requiring them to appear in high-cost healthcare settings, digital health is a vital component. Industry leaders increasingly are undertaking such initiatives. Hwang said three ACHP member health plans launched virtual-first insurance products in 2021, allowing members to receive primary care, integrated behavioral health and urgent care initially via telehealth. The premiums for those products are almost 20% lower than those for comparable standard plans.
More broadly, consumer interactions across industries have been going digital, and that societal trend will only accelerate in coming years. “Everything in healthcare is or will be digital,” Neuwirth said.
He added that digital platforms need to extend beyond telehealth and virtual care to encompass comprehensive use of databases, artificial intelligence and customer relationship management systems.
Digital health at its full potential “is clearly much more cost-effective and much more scalable than anything else that’s come before it,” he said.
10. Embracing Disruption
For traditional healthcare entities such as hospitals and health systems, the risk of losing business to outside innovators has long been a topic of conversation. Today, disruptors are preparing to bring better approaches to health maintenance directly to consumers.

Ceci Connolly, president and CEO, Alliance of Community Health Plans
Ceci Connolly, president and CEO of the Alliance of Community Health Plans, said the industry should have “a sense of urgency about this, particularly when you look at a lot of the disruptors that are coming to healthcare — frankly, disintermediating many of these legacy players.”
The greatest disruption will be around the general concept of patient-centered care, Angood said. The traditional players don’t move quickly enough in that space, while outside innovators may not grasp the nuances of a $4 trillion industry. The obvious solution is to look to collaborate.
The need to solve the puzzle is why HFMA will “continue to push cost effectiveness of health,” Fifer said. “I strongly believe that we in the industry need to drive this change. I get the complexity, but we have to start to figure it out.”





