Creating a Consumer-Centric Healthcare Delivery System: A Report from HFMA’s 2018 Annual Conference
Click here to download the full report
Emerging best practices can help healthcare organizations improve the patient experience from beginning to end, thereby enhancing customer loyalty and fortifying market share.
The evolution of the healthcare industry to a consumer-oriented model continues to accelerate. With a wider variety of choices and greater financial incentives to be selective in where they get their care, consumers are forcing healthcare organizations to rethink how they can best serve current and prospective customers. This trend affects all aspects of a healthcare organization, from the revenue cycle to clinical operations to administrative decision making. Viable strategies incorporate everything from patient engagement to price transparency to marketing tactics.
These strategies and more were detailed as part of a cohort track, Creating a Consumer-Centric Healthcare Delivery System, at HFMA’s 2018 Annual Conference in Las Vegas. The cohort was sponsored by Simplee and Change Healthcare. In six sessions over two days, attendees heard from a variety of industry experts on ways to become more attuned to the demands of healthcare consumers.
Consumerism from a Medical Perspective
The conversation that needs to start taking place between physicians and patients is about cost of care, said Orly Avitzur, MD, a board-certified neurologist and medical editor and writer. “Patients care about this as much as they care about their health,” said Avitzur, formerly medical director at Consumer Reports.
At many meetings she attends, Avitzur said, she asks assembled physicians how many of them know the cost of any test, drug, or treatment at the time they recommend it.
“Very rarely is there even a single hand raised,” she said. “Physicians are blind to it. It’s an opaque system unless you work for an organization that’s closed, like Kaiser, where they can bring that all to the dashboard.”
The dearth of knowledge is why healthcare finance leaders need to help “create interfaces and conversations so that clinicians can do a better job of having these questions.”
Medication costs particularly pose a challenge. Too often, Avitzur noted, patients find out their out-of-pocket cost only upon arriving at the pharmacy.
Potential solutions can be derived from smartphone technology, she added. Imagine a phone app that allows patients to scan their insurance card and see their out-of-pocket cost for a drug while they are sitting with a clinician.
Such technology would be a vast improvement over the current situation, where physicians generally don’t know where to turn for answers. In a recent physician survey that Avitzur helped conduct with Consumer Reports, fewer than half of respondents were aware of online resources that can provide information about drug costs.
“The thing that I found very optimistic was that two out of three said they would go to a workshop on understanding, incorporating, and discussing cost of care,” Avitzur said. Healthcare finance leaders can have that conversation with the physicians in their organizations, she suggested. “They want to know, and I think what they would learn would bring back great value to their conversation with the patient.”
Physicians should provide names of specific medications, tests, and treatments to allow patients to explore their out-of-pocket costs and additional costs, such as the price of traveling to an appointment or lost wages from missing work, Avitzur said. “These all play a role in how the patient feels about that physician-patient encounter.”
Recommendations at the organization level include routinely screening patients for financial sensitivity through practices such as pre-visit questionnaires, consultations with financial counselors, screenings for social determinants of health, and leveraging of the electronic health record.
See related sidebar, From Our Sponsor, below.
Organizations also should prod patients to initiate cost-of-care conversations. The same sort of posters that encourage patients to ask clinicians whether they have washed their hands also could be deployed to embolden patients to raise the cost issue. Patients may be reluctant to bring up the topic for various reasons, including not wanting to take up the limited time they have with their physician, Avitzur said.
Cost of Care: What Physicians Say
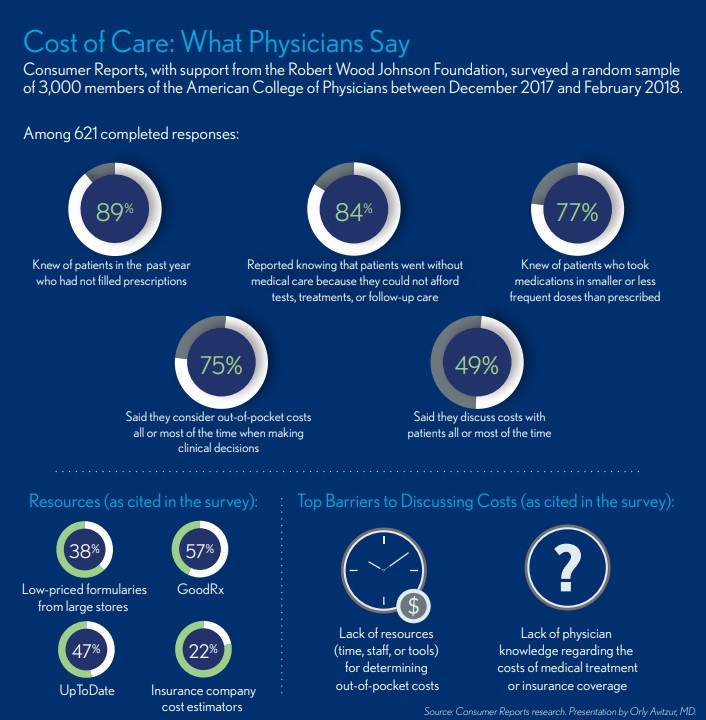
“We need to provide education to all clinicians and staff on the cost of care, how to have those discussions, and where the resources are,” Avitzur said. “It needs to be provided with easy access for both patients and clinicians, whether it be links to websites or posted in portals.”
But consumer-advocacy initiatives will do little good, Avitzur said, as long as physician burnout remains pervasive in health care. Characterized by emotional exhaustion, cynicism, and decreased efficacy at work, physician burnout can negate an organization’s efforts to become more consumer-friendly.
“Any interaction that was suboptimal can likely be explained by this syndrome of physician burnout,” Avitzur said. “It’s not just a syndrome that occurs on an individual level. It’s a problem with institutions. It’s a problem with the system. It’s a problem with the requirements that are placed on physicians that they never expected to encounter.”
The consequences for patient care are profound, Avitzur said. She cited several studies, including one that linked burnout of emergency physicians with a prolonged waiting time for patients who visit the emergency department. “We all know what happens when people line up in the emergency room and don’t get service expeditiously,” she said.
Burnout is costly to organizations, especially given that it leads to higher turnover rates. The cost to replace a physician is two to three times higher than the physician’s annual salary, Avitzur said, citing a study. “Those are high costs,” she said. Other financial implications include productivity decreases, poorer performance on quality metrics, and costly follow-up care and possible legal ramifications when a patient is harmed by care from a burned-out physician.
The adverse effect on consumer engagement cannot be overlooked, Avitzur said. “When physicians are working at their optimal best and not burned out, they are often asked many questions by patients,” she said. “That’s what makes good care—an open conversation between patients and their physicians.”
Guiding Principles of Patient Experience Excellence
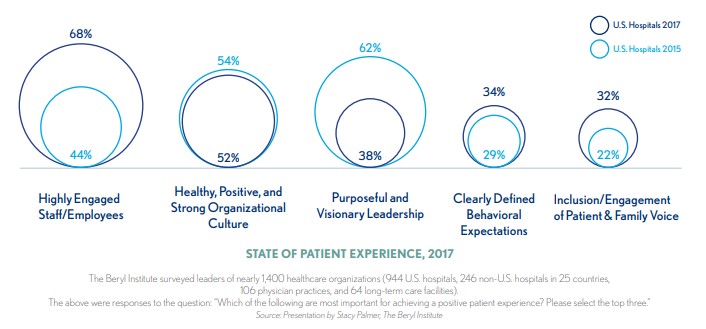
Patient experience is about choices, specifically the ones that healthcare leaders make for patients and for their organizations, said Stacy Palmer, senior vice president with The Beryl Institute, a global community of practice and thought leadership on improving the patient experience.
Surveys conducted by The Beryl Institute show that patient experience is fast becoming a central focus of healthcare organizations, starting in the C-suite. That is where organizations can begin in their efforts to optimize the patient experience, said Palmer, who offered eight guiding principles as developed by The Beryl Institute.
Identify and support accountable leadership with committed time and focused intent to shape and guide experience strategy. “The organizations that are truly succeeding in patient experience efforts have put someone in place—either an individual or in many cases a department—to address patient experience from a holistic viewpoint,” Palmer said.
Titles that are becoming more common in healthcare organizations include director of patient experience, manager of patient experience, and chief experience officer. “The most important thing is that they have the access to the leadership team or a leadership champion to help them be successful in this work,” Palmer said.
Establish and reinforce a strong, vibrant, and positive organizational culture, and all it comprises. This principle is arguably the most important of all, Palmer said, yet also the most difficult to implement.
Keck Medicine of USC, in Los Angeles, undertook an initiative to improve the organizational culture for the sake of the patient experience. Palmer had the opportunity to visit the organization and report on its progress.
The academic medical center instituted a training curriculum, rewards and recognition programs, and had significant physician onboarding. “One of the most interesting things to me in what they did is the programs person who is responsible for patient experience at Keck is also responsible for employee engagement,” Palmer said. “She’s actually part of the HR department. That synergy has worked incredibly well for them.”
Develop a formal definition for what experience is to your organization. Organizations cannot hold employees accountable for the patient experience without making clear what the term means, Palmer said.
The Beryl Institute’s definition is “the sum of all interactions, shaped by an organization’s culture, that influence patient perceptions across the continuum of care.” This definition goes beyond customer service to include quality, safety, outcomes, and cost.
Implement a defined process for continuous patient and family input and engagement. Implementation of this principle is becoming more frequent in health care, Palmer said. “Getting the input from the people you’re serving is critical.”
Palmer shared the example of Lurie Children’s Hospital, Chicago, which contracted with a well-known German artist to design stained glass windows for a new chapel. When hospital administrators took the end product to their patient and family advisory council, the feedback was unexpectedly negative. The stained glass was too reminiscent of death and sorrow, especially for a chapel in a children’s hospital.
“They suggested something more uplifting and inspiring, and almost a little bit whimsical,” Palmer said. The modified design set a more appropriate tone.
Engagement leaps to top for achieiving positve patient experience
Engage all voices in driving comprehensive, systemic, and lasting solutions. Healthcare organizations should not overlook vendors as a resource for sparking vital improvements.
For example, Palmer said, Phoenix Children’s Hospital partnered with its imaging provider when building a new emergency department. The goal of the resulting design and the accompanying staff training was to reduce patient anxiety during tests.
Look beyond clinical experience of care to all interactions and touch points. Boston Children’s Hospital mitigates the strain of trying to park in downtown Boston by providing guidance and tips before patients and families come to the hospital. Attendants on-site offer further direction.
Finally, if a family makes it all the way to the top of the parking garage and still cannot find a spot, a valet is on hand to park the car. “What a relief that would be versus having to drive all the way back down, find another place to park, and then make it over there,” Palmer said.
Focus on alignment across all segments of the continuum and the spaces in between. This aspect of strengthening the patient experience is easily overlooked, Palmer said. “It really speaks to transitions of care,” she said. “Finding ways to help manage those transitions and make it simpler for patients will build their confidence in your care, their comfort, and will lower their anxiety levels.”
That approach should be applied to transitions not only between facilities, but between departments.
Encompass both a focus on healing and a commitment to well-being. Hospitals and health systems are making significant strides in this area, Palmer said. Many organizations host health and wellness fairs, sponsor runs, and provide training classes for their communities. The goal is to “be partners within their care before they even arrive to you for services.”
Reimagining the Revenue Cycle
The revenue cycle intersects with a healthcare organization’s brand identity arguably more than any other aspect of the operation, said Andrew Gwin, a regional revenue cycle director with Ascension Health.
“Outside of medical care, the number-one reason patients will return to an organization is revenue cycle—the billing experience, the financial experience,” Gwin said. Improving the consumer experience by improving the revenue cycle involves three areas, Gwin said:
- Scheduling
- Registration
- Bill payment
Those areas do not touch on all aspects of the consumer experience, “but they’re the three areas of the revenue cycle where we have the most intersections and the most opportunities to improve your brand loyalty and experience with your patients,” Gwin said.
To optimize scheduling, Ascension implemented a technological solution for diagnostic scheduling and order facilitation, seeking to ensure patients can self-schedule and receive the appropriate resources in the appropriate setting—acute or ambulatory—at the appropriate time. Self-service also applies to physicians, allowing them to make referrals without having to go through a call center.
“The other thing we’re taking advantage of with the online scheduling is it allows us, when patients are leaving the ER, to book primary care appointments for those that don’t have a primary care physician and have been using the ER as primary care, as well as with follow-up appointments,” Gwin said.
“We’re also using it in the inpatient acute-care discharge setting to help around readmissions so that we can help patients who have a high risk of readmission book appointments for follow-up care before they leave the hospital. It gives you additional value in the organization from a clinical perspective.”
Ascension sought to streamline registration and preregistration by allowing patients to self-register and complete the preregistration process digitally for acute and ambulatory appointments.Crucially, patients also receive an interactive estimate that accounts for their insurance benefits and apprises them of the portion of the cost that will be their responsibility. Providing this information is a vital step in helping an organization improve its collection yield.
Ascension modernized its billing processes by allowing patients to enroll in an online platform. For patients who need financial assistance or long-term payment plans, options can be customized through the platform.
The platform also allows for the integration of all bills from an episode of care.
“One of the things we’ve talked about as an organization is progress before perfection,” Gwin said. “We’re trying different things at different times in different locations, so we can get it out there and move forward. Sometimes, historically, that challenge has been trying to perfect it, and we slow down the innovation.”
Avoiding that pitfall is “something we really focus on within our organization,” Gwin said.
Innovation in the revenue cycle will become even more important as the healthcare industry transitions from an inpatient to an outpatient model of care, Bob Broadway, who spent 24 years in administration with Bethesda Health in Palm Beach, Fla., said during a separate presentation. That’s because cost-to-collect is significantly higher on the ambulatory side.
“Collecting that 90-day copay or a $50 deductible after a visit, and they’re gone, is so much more costly compared to a $10,000 DRG from another payment source,” said Broadway, managing executive with Strategic Advisory HC. “Our industry is going to have to take down the cost of that transaction with a number of different technologies that are available to us.”
Blockchain and cryptocurrency are examples of emerging technologies that could make a profound difference.
“Imagine if an outpatient setting goes from the billing of today to a blockchain type of delivery where things are recorded,” Broadway said. “It’s secure, so no PHI issues. Then what if you had a crypto benefit where the benefit was out here in the cloud, and that payment was made simultaneously?”
The industry’s transition to an ambulatory care model does not account for the possibility of even greater disruption from totally new approaches, such as the Amazon-Berkshire Hathaway-J.P. Morgan joint venture.
Traditional healthcare organizations will have to innovate to retain their foothold with consumers.
“What we’ve seen in our enterprise is every time I’ve added a new technology, a new solution, we’ve added three people in IT,” Broadway said. “That’s because we don’t have the interoperability that’s needed, such as in a banking transaction. I predict we are going to get interoperability, and not just the old HL7 interface transactions.
“Can you imagine if a system could take all of that cost out of the administrative side, which we’ve been working on? You talk about a disruption to the world. What a positive disruption it would be.”
From our sponsor

John Dwight, vice president of marketing and partnerships at Simplee, on the company’s role in helping organizations establish a consumer-centric healthcare delivery system:
“Our company was founded by our CEO who came up with the idea because he, himself, had a really broken experience in receiving medical bills for his family’s visit to a hospital.
“As a company, we approach this problem of consumerism as people who have been in health care, and as people who have been in technology. We believe that there’s a way to give consumers and patients what they want through technology to make these experiences better—more information in the hands of consumers and putting them more in control through self-service.
“Through that, we can turn the healthcare experience into one that looks a lot more like the types of experiences that consumers have in all other parts of their lives. The common thread is that when a patient has more information and is having a better experience, it’s better for the patient and better for the health system. It’s a better conversation with the physicians and a better conversation about how to pay the bill and manage the financial part of it.”





