How CFOs can bring the rigor of finance to the call center
A health system’s call center can provide a powerful revenue impact if it is accessible to patients 24/7. But health systems need to address many strategic considerations when planning for such a function.
Health system call centers are universally acknowledged as significant cost centers. Too often, however, they are viewed as non-revenue-generating cost centers. In fact, a call center’s performance also affects revenue growth factors such as clinician utilization and patient loyalty.
Despite the multiple ways that call centers affect both the bottom and top lines, there is no universal rule among health systems regarding which C-suite executive should be directly responsible for the oversight of the call center. Even if the CFO is not directly responsible, the finance leader’s involvement is imperative to balance the fixed and variable cost and associated revenue to maximize the ROI.
For the CFO, the primary concern is to make sure the center optimizes the trade-off between access and cost. Access has three primary components:
- Call center hours of operation
- Wait time for a patient to connect with an agent
- The center’s ability to handle all the relevant functions (e.g., scheduling, insurance verification, authorization) in a single call
To verify the center provides an optimal cost/benefit to the organization, the CFO must measure operating and capital costs against the direct and indirect revenue realized. To do so, the CFO must understand the financial and strategic impacts of a call center in general in three areas:
- Revenue
- Operating expenses and capital deployment
- Patient experience
Revenue impacts
The call-center function can drive revenue by optimizing clinicians’ schedules. One widely cited estimate from 2017 suggests that missed patient appointments cost provider organizations $150 billion in revenue annually.a A system that helps patients schedule and, perhaps more important, reschedule appointments improves utilization and adds incremental revenue.
Health systems miss an opportunity to maximize available provider schedules when there is a high number of no shows. Higher than normal no-show rates directly result in quantifiable lost revenue. Poor call center performance — typified by long wait times and unanswered calls — can drive patients to competitors.
A high-functioning call center also helps improve a health system’s revenue performance by having agents consistently walk patients through a preregistration process in which all necessary steps, including insurance confirmation and prior authorizations, are completed before the appointment. Agents can make patient financial responsibility clear upfront and help ensure the health system is being compliant with the No Surprises Act.
Operating expense and capital deployment
A health system’s call center has direct and indirect expenses. The specific costs are determined by the call center model the health system chooses to adopt. Options include:
- A fully owned-and-operated (O-and-O) call center
- Outsourced management of an O-and-O call center
- A hybrid model that adds outside capacity to an O-and-O call center
- A fully outsourced call center
An initial step in assessing the costs associated with any of these models is to establish uniform measures. The most common approach is the cost per one minute of call time.
To calculate the cost per minute, it is necessary first to ensure that all the expenses associated with the call center are accounted for. For an O-and-O model, these expenses include:
- Agents’ wages and benefits
- Recruiting and training costs, including the cost of turnover
- Management (whether salaries and benefits for in-house management or the cost of outsourced management)
- Call center technology platform, IT and telecommunications fees
- Real estate and other overhead
Outsourced models factor in the fee paid to the outsource partner, in addition to any of the O-and-O costs the health system retains.
Dividing the total cost for one month by the number of calls or call minutes serviced in the month yields a unit value. Calculating the unit measure this way provides a basis for assessing the cost of adding an hour of service to handle additional calls.
Patient experience
A call center’s ability to effectively assist patients in accessing appointments, preregistering and addressing billing and collections issues will affect patients’ perception of their overall experience with the health system.
Patients enjoy the convenience of digital communication tools — e.g., self-scheduling, reviewing test results, receiving appointment reminders, researching specialists — when those tools can effectively solve their problems. But even digitally savvy patients often need human assistance to help them navigate the widening array of care options. They also need answers to myriad questions about their financial responsibility, insurance coverage, pre-authorizations and other complex issues.
By answering these questions, reducing friction in the scheduling and rescheduling process, and avoiding billing surprises, a call center helps patients get the care they need, improves their care experience and builds loyalty.
Key factors to consider
Health system CFOs should consider the following three factors when assessing the potential efficiencies of their organizations’ call centers.
1 Optimized staffing. Matching staffing levels to patient call demand is the foremost operational challenge for a call center. Call-center agents, naturally, prefer to work in a schedule that approximates local business hours. Most agents want to work on a fixed schedule, arriving and departing from the call center at roughly the same times each day.
With some variations in start times, a physical call center with these limitations on scheduling flexibility can readily provide some level of coverage between 7 a.m. and 7 p.m. But it may struggle to find enough for the peak call times of early afternoon and early evening. This situation often results in the call center being overstaffed during less-busy morning hours.
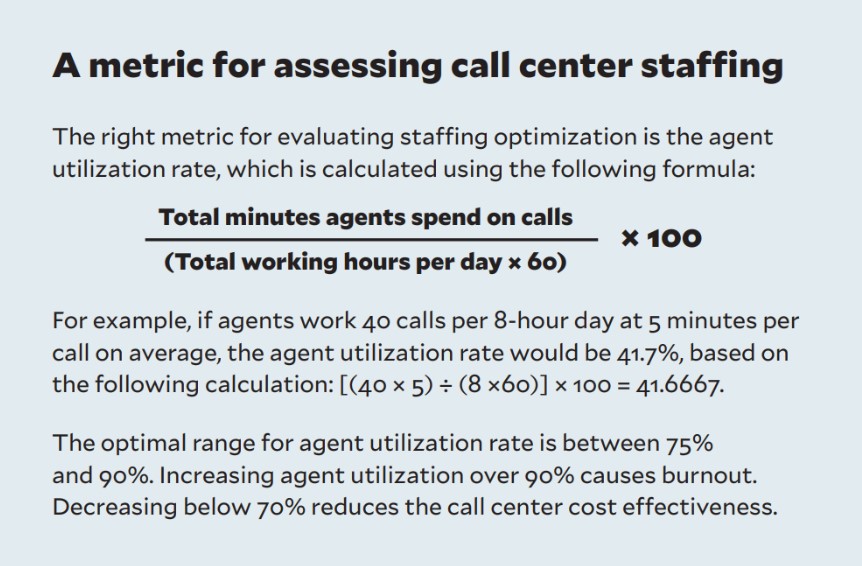
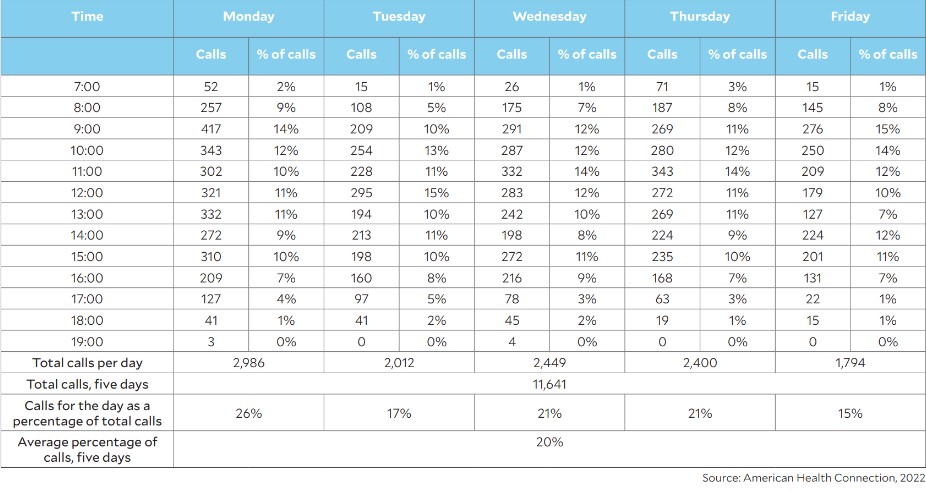
The problem is that inflexible schedules don’t account for variations in call volume across a single day or between individual days of the week, as exemplified in the exhibit below.
Call volume hourly distribution for a typical week
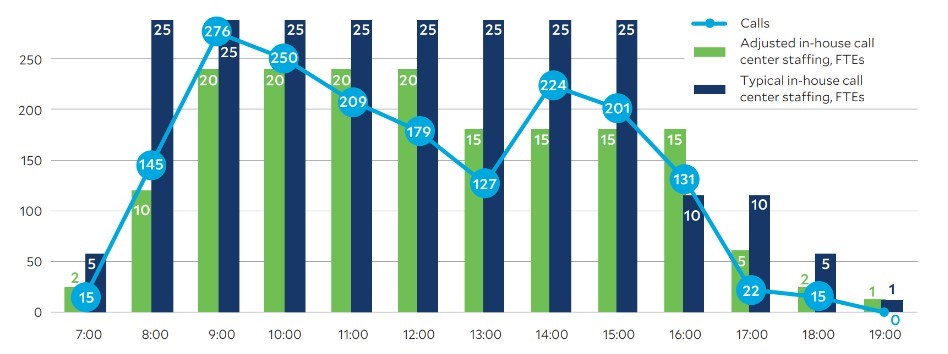
To illustrate the benefit of using adjustable staffing versus the more typical approach, the exhibits below compare the adjustable approach with the more commonly used approach based on the health system’s actual Monday and Friday call volumes presented in the previous exhibit. The adjustable staffing figures in the exhibit are based on an industry-standard formula known as Erlang C.b
Comparison of Friday staffing: Flexible varied daily staffing approach versus the fixed daily approach
2 Recruiting, training and retaining talent. A call center with hours extending beyond local business hours will face competition in recruiting and retaining qualified agents from call centers that are only open during normal business hours (e.g., 7 a.m.to 5 p.m.).
CFOs whose organizations are intent on owning and operating a call center should keep in mind the following potential pitfalls associated with recruiting and training new agents:
- Once trained, agents may be tempted to move to other call centers.
- Highly qualified agents may chafe at having the constant responsibility to train newcomers, potentially increasing the turnover rate, which can be as high as 38% annually.c
- The requisite skill set for a call-center manager may not be readily available in-house or from the health system’s primary talent sources.
The first two pitfalls can be addressed through appropriate incentives. In the latter case, a talented call-center manager could be recruited from outside of healthcare, although the person would have a tight learning curve on the healthcare world.
3 Capital investment/expense assessment. As an important part of planning for an O-and-O call center, CFOs will need to evaluate the call center function’s capital needs, including office space and furnishings for any in-person call centers, equipment and software for both in-person and remote call capacity, and other capital costs.
Setting up remote call capacity may eliminate or lessen the need for office space. On the other hand, with hybrid work arrangements taking up a greater share of office work even in health systems, a health system may have office space readily available for the call center function that otherwise wouldn’t be occupied.
These capital needs are avoided if the call center is outsourced, but in such instances, the CFO must factor in the ongoing annual expense of paying for the outsourced solution.
Other factors in optimizing ROI
Two other factors that weigh on performance must be evaluated.
1 Scale of call volume. Before building an O-and-O call center, the CFO should verify that call volume will be sufficient to justify the investment. For example, scale can make it easier to deploy call agents efficiently, as there tends to be a wider variety of projects that agents can be deployed on when there is a larger patient base. Fixed costs for equipment, software and management also are more efficient when spread across more patients and more call demand.
2 Agent readiness to respond appropriately to calls. The CFO should confirm that the call center can provide the right training, scripts and call escalation procedures to ensure that patients are preregistered properly. The best way to do so is to analyze revenue cycle data to find root causes for claim denials or surprise bills for patients and then trace those root causes back to ways the call center is set up to address such issues.
A vital strategic asset
Even as digital tools expand and improve a patient’s experience, there will always be a need for direct and personal patient-to-provider interaction. Financial leaders should track scheduling call center performance metrics just as they do for revenue cycle billing and follow-up functions.
Simply put, by providing a point for human connections between patients and a health system, a high-quality call center can help in realizing the following important objectives:
- Drive increased provider utilization rates
- Improve preregistration processes to help avoid denials and improve collections
- Build patient loyalty
Footnotes
a. Gier, J., “Missed appointments cost the U.S. healthcare system $150B each year,” Healthcare Innovation, April 17, 2017.
b. For an explanation of the Erlang C formula, see Awati, R., “Erlang C,” TechTarget, page last updated March 2022.
c. SQM Group, “Call center attrition rate – is it now the most important KPI?” March 30, 2023.
3 essential call center staffing solutions
The improved efficiency from adopting an adjustable approach to call center staffing stems from three solutions.
1 Flexible capacity. Having a more varied hourly capacity depends on allowing for more flexibility in staffing. An owned-and-operated call center may be able to augment its in-person agents with remote capacity by enabling agents to take on short remote stints from their homes. A health system also can plan on bringing in outside agents to help cover peak demand times and off hours.
2 Redeployed morning capacity. With lower inbound call volume in the morning hours, agents could be redeployed to later hours or use the less busy times to complete ongoing training.
3 Incentives for staff to work off-hours. Such incentives might include, for example, additional pay or promotion opportunities.





