Future of Strategic Investment
Ready or not, the long-expected disruption of healthcare is coming, and leaders are preparing in various ways.
By NICK HUT
Hospitals’ role in healthcare is poised to shrink in the coming years, triggering a need for self-evaluation and reflection on how to adapt to the predicted changes.
Most immediately, a shifting of inpatient care to outpatient facilities is expected to continue, with a recent HFMA survey of financial executives projecting that the median percentage of revenue coming from inpatient care will fall to 25% by 2030 from 40% in 2019 and an expected 34% in 2022.
But that shift tells only part of the story. Hospitals in 1980 commanded 40% of national healthcare spending, and since 2000 their share has hovered around 30%, according to CMS actuaries.
At least one healthcare expert sees regulators and insurers pushing that percentage down to about 26% in the foreseeable future, which would translate to a loss of $50 billion per year relative to 2019.

“Hospitals will not be the hub of the wheel. They will be a piece of something.”
Paul Keckley, PhD
independent healthcare consultant
“Hospitals will not be the hub of the wheel,” said Paul Keckley, PhD, a longtime healthcare policy analyst and managing editor of The Keckley Report. “They will be a piece of something.”
To retain a viable slice of the pie, “Inevitably you diversify the operation beyond simply acute, outpatient and physician services,” Keckley said. “I think it does require [short-term] post-acute services to be delivered in homes and digital settings. And you’ve got to develop a set of retail services, targeting employers in other sectors.”
As risk-based, capitated contracts become more widespread, he added, there also will be room for hospitals and health systems to do good business by formally aligning their operations with public-health services.
“If I were running a 200-bed community hospital, and I’m looking at what’s ahead, I’m probably not throwing all my CapEx at conventional inpatient services,” Keckley said.
That hospital instead should be coordinating with local authorities to incorporate public-health programs; entering into direct contracts with employers to provide retail-type services, among other offerings; and launching or co-sponsoring a health plan to justify the level of financing that will be needed to address social determinants of health.
“You’ve got to do all that,” Keckley said. “And you’ve got about three to five years to make that move.”
Such investments will be manifested in various initiatives, starting with a greater emphasis on health equity.
HEALTH EQUITY: A STRATEGIC PILLAR
Healthcare leaders increasingly see investments in improving health equity as central to their mission of advancing population health. The issue is one of fairness and justice but also has practical implications. For example, CMS in October 2021 said it expects all Medicare fee-for-service beneficiaries and most Medicaid enrollees to be in accountable care arrangements by 2030, meaning a provider’s financial performance will partially hinge on better serving customer segments that may have been overlooked previously.
Northwell Health, the largest health system in New York state, has made equity a strategic focus for the last decade and is working to expand those efforts. The organization wants to ensure that its care delivery meets “21st century standards of dealing with the epidemic of chronic disease,” said Jennifer Mieres, MD, senior vice president of Northwell’s Center for Equity of Care.
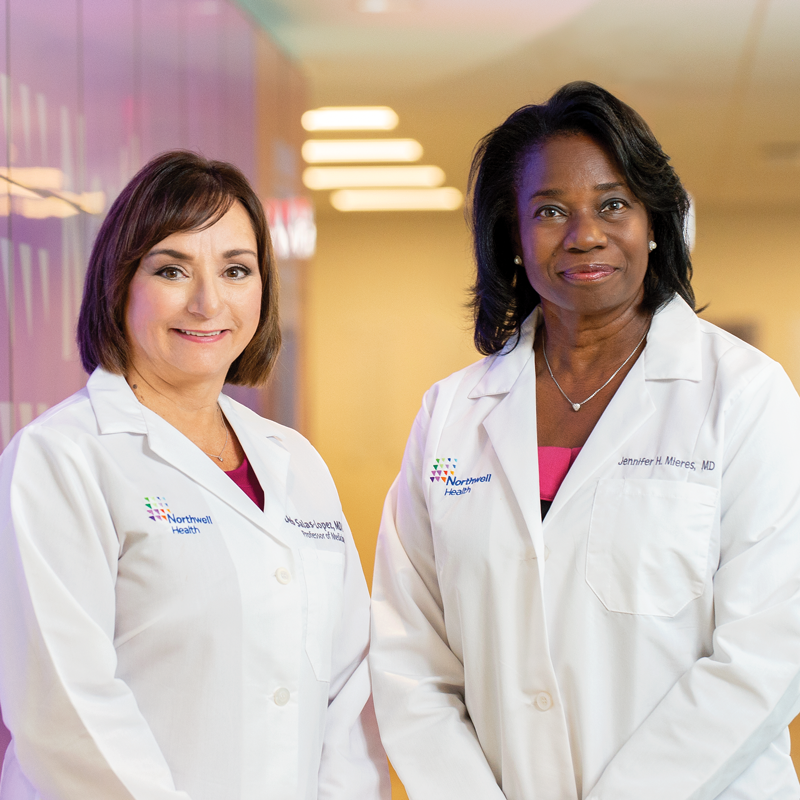
Debbie Salas-Lopez, MD, MPH, and Jennifer Mieres, MD, lead initiatives to promote health equity at Northwell Health.
By 2030, she said, the objective will be “true customized care delivery, with no disparities or discrepancies or differences in health outcomes based on race, ethnicity or preferred language.” In such a scenario, gaps in readmissions, morbidity and mortality will be eliminated.
Best practices in data collection and analysis will be essential for organizations to understand and tackle the causes of inequity. Northwell Health eventually will have equity metrics on its clinician dashboards, Mieres said, including measures that reflect the link between equity and quality and that show the impact of culturally sensitive care.
Formal ties to community-based organizations also will be needed, especially in areas where residents lack virtual access, said Debbie Salas-Lopez, MD, MPH, Northwell Health’s senior vice president for community and population health. A health system “will no longer be an island on its own, but rather a partnership,” she said.
Collaboration will take different forms in different communities. In some places, alliances with faith-based organizations will allow a health system to deliver basic care at religious institutions. Schools and community centers will be among various other options for partnerships. All such associations will serve as vehicles for imparting the type of health and wellness guidance that can keep people out of the hospital.
Partnerships also will help address the link between social determinants and population health outcomes. Northwell is spearheading a nationwide collaborative, with research funding from the National Institutes of Health, to promote gun violence prevention. An organized effort to frame and ultimately tackle the disparate effects of climate change is in the preliminary stages.
“Our swim lane is taking care of the different illnesses that affect our community, but we can’t look away from the symptoms of the bigger societal problems,” Salas-Lopez said.
A futurist’s vision of investment models

Carter Dredge, MHA, lead futurist with St. Louis-based SSM Health, often gets asked about his job title.
“People say, ‘What do you do? Do you have an actual job?’” Dredge said.
In fact, the role was created for Dredge in May 2021. His new position is rare in the hospital and health system industry, but he suspects other organizations will consider adding the title to their C-suites in an effort to keep up with sweeping change.
As a futurist, compared with his time as SSM’s chief transformation and strategy officer over the previous 3 ½ years, Dredge spends more time conceptualizing the types of business models that will be necessary to “shape the future” of healthcare. One of his biggest concerns is that too many investments and innovations across the industry fizzle out because of a lack of scale.
And yet, “We can’t have every hospital merge with every other hospital just to solve a nuanced problem,” he said. “How can we create a financial and economic vehicle to allow for focused yet scalable innovation?”
Dredge’s solution over the next decade is for industry stakeholders to form what he calls healthcare utilities, which would bridge the divide between private-sector competition and government regulation.a An early example is Civica Rx, the not-for-profit manufacturer of generic drugs that was launched in 2018 by leading health systems and philanthropies. (Dredge is a Civica founder and board member.)
Dredge envisions healthcare utilities as 501(c)4 social welfare organizations that are managed by stewards, not owners. Financing comes not from equity but from low-interest, long-term loans put up by the customers that will be buying the goods or services.
The absence of equity stakes means growth is not cashed out by the partners but instead is funneled into business operations. If the entity gets sold, the proceeds go to charity.
“These entities provide services at the same prices for everyone, transparent for everyone,” Dredge said. “And that’s where they get their name as a utility.”
a Dredge, C., and Scholtes, S., “The Health Care Utility Model: A Novel Approach to Doing Business,” New England Journal of Medicine, July 8, 2021.
DIGITAL HEALTH: TABLE STAKES IN EMERGING MODELS
With an expected prevalence of risk-based payment frameworks in 2030, a provider’s success will depend on helping patients avoid hospital visits. Investments that boost primary care access and enhance the ability to check patients’ health from afar will be vital.
That context is why terms such as “digital front door” and “remote patient monitoring” no longer are talked about as futuristic ideals but instead are being incorporated in ongoing strategies.

“Do you have a system to manage all of that information today? How are you organized to respond to the information today?”
Mitchell Schwartz, MD
President of Luminis Health, Clinical Enterprise, Annapolis, Maryland
Health systems need to invest in providing an app-based “bidirectional” experience, said Mitchell Schwartz, MD, president of Luminis Health Clinical Enterprise in Annapolis, Maryland. Prospective patients should be able to type in a question on their phones, receive relevant clinical guidance and self-schedule an in-person or virtual appointment as needed. Behavioral health cases could be triaged in real time.
“The value is the access,” Schwartz said. “The medical information is almost secondary.”
While patients will have an easier time actively engaging with the care delivery system, they also will be more connected around the clock through wearables and mobile technology. Provider organizations should expect to monitor and manage heart rate, blood pressure and blood glucose levels across at-risk patient populations.
The resulting trove of customer data will be difficult to utilize unless providers have made appropriate investments in processes and expertise. When organizations attain the ability to remotely monitor blood pressure across a patient panel, Schwartz said, the question becomes, “Do you have a system to manage all of that information today? How are you organized to respond to the information today?”
Physicians won’t operate as the sole leader of a care team in that scenario but instead will integrate their skills with those of data analysts, advanced medical assistants, pharmacists, social workers, genetic counselors and health coaches.
The increased focus on care delivered remotely and in nonhospital settings “will push the healthcare system to rely less on one-on-one interactions and more on continuous touchpoints with integrated care teams,” said Maureen Sullivan, chief strategy and innovation officer for the Blue Cross Blue Shield Association.

“The healthcare system [will] rely less on one-on-one interactions and more on continuous touchpoints with integrated care teams.”
Maureen Sullivan
Chief Strategy and Innovation Officer for Blue Cross & Blue Shield Association
HOSPITAL IN THE HOME: A VITAL COG
The impetus to move care to lower-cost settings as part of risk-based models will spur an expansion of home-based acute care and disease management programs over the next decade. Home-based care also will be part of a shift from a provider-centric model to a more tailored approach.
“I don’t know anyone who says, ‘I want to go to the hospital.’ Thinking about how much care can be provided in the home, and really stretching that thinking, is going to be important,” said Michelle Conger, chief strategy officer with OSF HealthCare in Peoria, Illinois, and CEO of OSF OnCall Digital Health.

“Thinking about how much care can be provided in the home, and really stretching that thinking, is going to be important.”
Michelle Conger
Chief Strategy Officer with OSF HealthCare, Peoria, Illinois
OSF opened a digital center that can support all levels of remote care, including an acute care hospital-at-home program that is in the planning stages. Conger even sees a day when labs will move from the ambulatory setting to the home.
As with other aspects of transformation, health systems will need to invest in processes and change management. Workflows need to be mastered to ensure that care in the home is performed at the same level as in clinics and hospitals.
To provide acute care in the home, for example, organizations will need to establish:
- An infrastructure that makes care available 24/7, just as it is in the hospital
- A unified medical record that can be accessed by all team members — including outside vendors — and is integrated with wearables and mobile apps
- Coordinated logistics that ensure supplies will be delivered to homes on demand
Organizations like OSF HealthCare, a 15-hospital system that includes several critical access hospitals, also must consider how the home-based care model can be dispersed to more remote areas.
“We can have a digital hub that supports people 24/7 for hospital-at-home, but each of those small rural markets will need to have some sort of capabilities that are distributed,” Conger said.
TECHNOLOGY: THE FOUNDATION OF NEW MODELS
The evolution of care delivery heading into 2030 will be underpinned by targeted investments in technology. Then again, the adoption of technology in healthcare rarely is straightforward.
Vic Gatto, a venture capitalist and the CEO of Jumpstart Health Investors, strives to anticipate the investment strategies that will help organizations adapt to emerging trends. He says technological innovation is tricky in healthcare because factors such as societal demographics and reimbursement policy determine how quickly innovations realistically can be implemented.
With the ongoing transition in the generational power structure from baby boomers to millennials and a federal push for payment innovation in the interest of sustainability, healthcare leaders should plan to see “much more change than you have in the past 10 years,” Gatto said. “You need to create strategies to have your organization be able to try things and adopt technology more quickly.”
There is ample room for technology to transform healthcare over the next 10 years. Artificial intelligence will allow for more precise insights about patients at both the population and individual levels. Robotic process automation will enhance the ability of clinicians to treat larger patient panels in value-based payment models.
But as with the digital front door and hospital-at-home, organizations must establish processes that allow them to capitalize on those innovations.
For example, AI will feed advanced diagnostics that can inform patients they’re at high risk of suffering a heart attack 15 years later. Health systems and health plans thus will need to invest in new forms of disease management, centered on wearables and telehealth but also including clinical roles that specialize in coaching and influencing. “We’re trying to steal from Madison Avenue,” Gatto said.

“We’re trying to steal from Madison Avenue.”
Vic Gatto
Venture capitalist and CEO of Jumpstart Health Investors
SERVICE LINES: A SHARPER FOCUS
Although ICUs, operating rooms and trauma centers will remain core components of health systems, a diminished acute care footprint will be a tangible result of industry transformation over the next 10 years.
One question will be how to respond when the exodus of many services — including an increasing number of surgeries — to ambulatory settings and the home leaves behind excess capacity in some departments.
“For a CFO, that’s a 10-year challenge of, ‘We have all these fixed assets, capital investment. How are we going to fill it as procedures migrate?’ It’s either repurposing [space] or specialization with a much larger catchment area,” Gatto said.
He added, “It’s kind of a reconfiguring of the asset mix across the country, based on: Can you attract the volume from a wider area? Do you have the brand or not?”
A key step will be a rigorous assessment of operational areas in which a hospital or health system can excel. With those insights, the organization can set its course along one of multiple paths.
For organizations that can’t become a destination for specialty care, alternative routes will be available. Keckley said some could develop into regional integrated systems of health with inpatient programs as mere cost centers. Other components would include:
- A professional services organization that goes beyond being a physician network
- A health plan
- A suite of digital and retail services
- Investments in startups that are “targeted to where the puck will be in seven to 10 years”
Smaller, sole-community providers will need to consider focusing on outpatient, emergency and senior health services and getting out of the inpatient business altogether, Keckley added.
“I don’t think where you’re starting predetermines your destination, but there will be advantages to the ones that get there earlier rather than the ones that are late,” he said.
COST-EFFECTIVE HEALTHCARE: THE RESULT OF A SOUND INVESTMENT STRATEGY
When crafting a strategy for the next 10 years, hospitals and health systems should consider whether their investments will improve the cost effectiveness of the processes that go into keeping their communities healthy.
“That’s the North Star for all of us,” said Greg Hoffman, CFO of Providence, the seven-state health system based in Renton, Washington.

“That’s the North Star for all of us.”
Greg Hoffman
CFO of Providence, Renton, Washington
Even the biggest providers won’t make much of a dent in cost-of-health inefficiencies unless a neutral agency or authority leads a national effort to quantify the effectiveness of processes, therapeutics, diagnostics and technologies, Keckley said. From there, pricing models can be applied to the things that work.
“We make a mistake in thinking about affordability and value by defining that in near-term process measures like 30-day readmission rates,” Keckley said. “I can game that system. We have to gear to longer-term results that involve all the touchpoints of care, including personal accountability and personal habits, not just what doctors do and what hospitals do. And then in all likelihood, that’s targeted with capitation.”
Until such a system becomes a reality, hospitals and health systems will do what they can.
Providence’s investment strategy relies on first simplifying and then modernizing before innovating. Only after workflows are streamlined and optimized will new technology such as a state-of-the-art electronic health record system help clinicians operate at peak performance instead of getting bogged down in wasteful practices that increase the cost of healthcare.
Analytics, specifically the combination of clinical data and cost-accounting data, presents a road map to investing in high-quality outcomes at lower costs. The insights can range from “particular suppliers that we use to different processes in an operating room,” Hoffman said.
For healthcare finance leaders wondering how their organizations can thrive in an era of strained resources, Northwell Health’s Salas-Lopez has an answer: “By going upstream and addressing preventable conditions through the right collaborations, the right outreach, the right access, the right education.”
That’s part of why community investment will be a strategic centerpiece in healthcare over the next decade.
“Let’s put on the table that this is a moral imperative,” Salas-Lopez said. “It’s also a business imperative.”