Healthcare 2030: Restoring Trust In Healthcare
With accelerated erosion of faith in the system, healthcare leaders see an urgent need to reconnect with patients.
By JENI WILLIAMS, HFMA CONTRIBUTING WRITER
|
As consumers’ confidence in healthcare organizations falters — whether due to access challenges, opaque pricing, missteps in responding to the pandemic, misinformation, healthcare inequities or some other reason — a large proportion of organizations are working to deepen connections with their communities. Since the COVID-19 pandemic emerged, the level of trust in the healthcare ecosystem has grown more volatile, research shows, with race and ethnicity, income level and gender impacting the level of trust. Now, there is evidence that declining trust affects health outcomes — intensifying the need for leaders to restore trust in care systems, services and teams. “It’s important for us to be thinking about how we build better trust with consumers and our patients,” said Niyum Gandhi, CFO and treasurer, Mass General Brigham, Boston. “If we let trust erode, it will play out through worse health outcomes; because if we can’t earn their trust, we won’t be able to do as good of a job in providing the best care we can for those who need it.” |
How trust issues affect healthcare organizations
A breakdown in healthcare trust runs deep and includes the following ramifications:
- Those with lower levels of trust in the healthcare system are less likely to engage in preventive care or to receive COVID-19 vaccines.
- Nearly 80% of patients said they will not return to the same provider if an experience causes them to lose trust.
- Lack of trust is associated with nonadherence to patient treatment plans.
- Consumers with higher levels of trust are more likely to accept changes in experts’ recommendations for their care, such as when scientific discovery calls for a new approach to treating chronic disease.
Sources: Brown School of Public Health and Microsoft AI for Health; Deloitte; 2022 Edelman Trust Barometer; and International Journal of Environmental Research and Public Health, April 18, 2021.
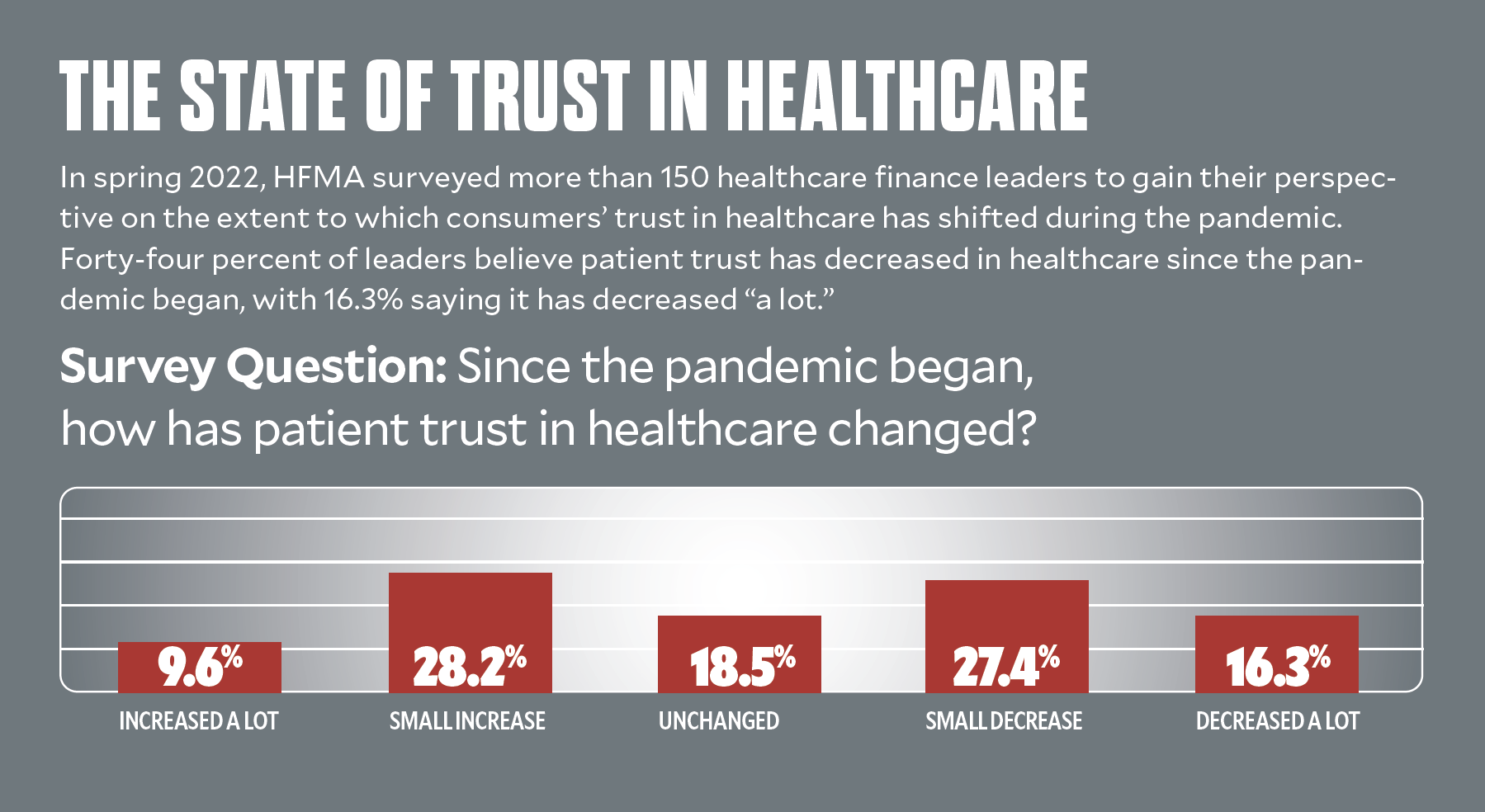
| To secure higher levels of trust, healthcare leaders must consider the extent to which trust may have eroded during the pandemic, the areas where breakdowns in trust exist and the steps their organizations should take to maintain or restore trust.Nearly half of U.S. consumers say they are less confident in the healthcare system’s ability to manage major health crises than they were before the pandemic, according to the 2022 Edelman Trust Barometer. Fifty-five percent say a negative healthcare experience caused them to lose trust in their healthcare provider, another survey found, while more than a third of respondents had skipped care because they did not like the way they were treated by a healthcare provider. |
Side effects from the pandemic
“During the pandemic, patients began to raise greater concerns about whether their expectations were being met at some of the most emotional points in their lives,” said Jason Wolf, president and CEO of The Beryl Institute, which is committed to transforming the human experience in healthcare. People’s expressed comfort with healthcare — and by extension, their trust in healthcare — has been challenged.
Nearly one out of four consumers surveyed by The Beryl Institute in March 2022 said the pandemic had changed their perspective of hospitals for the worse, Wolf said

Consumers aren’t the only ones to change behavior patterns or preferences in response to broken trust. A 2021 poll found one-third of physicians did not trust their healthcare organization’s leadership. Among nurses, 46% either do not believe their employer values their mental health or are neutral on this point, an American Nurses Association survey indicates.
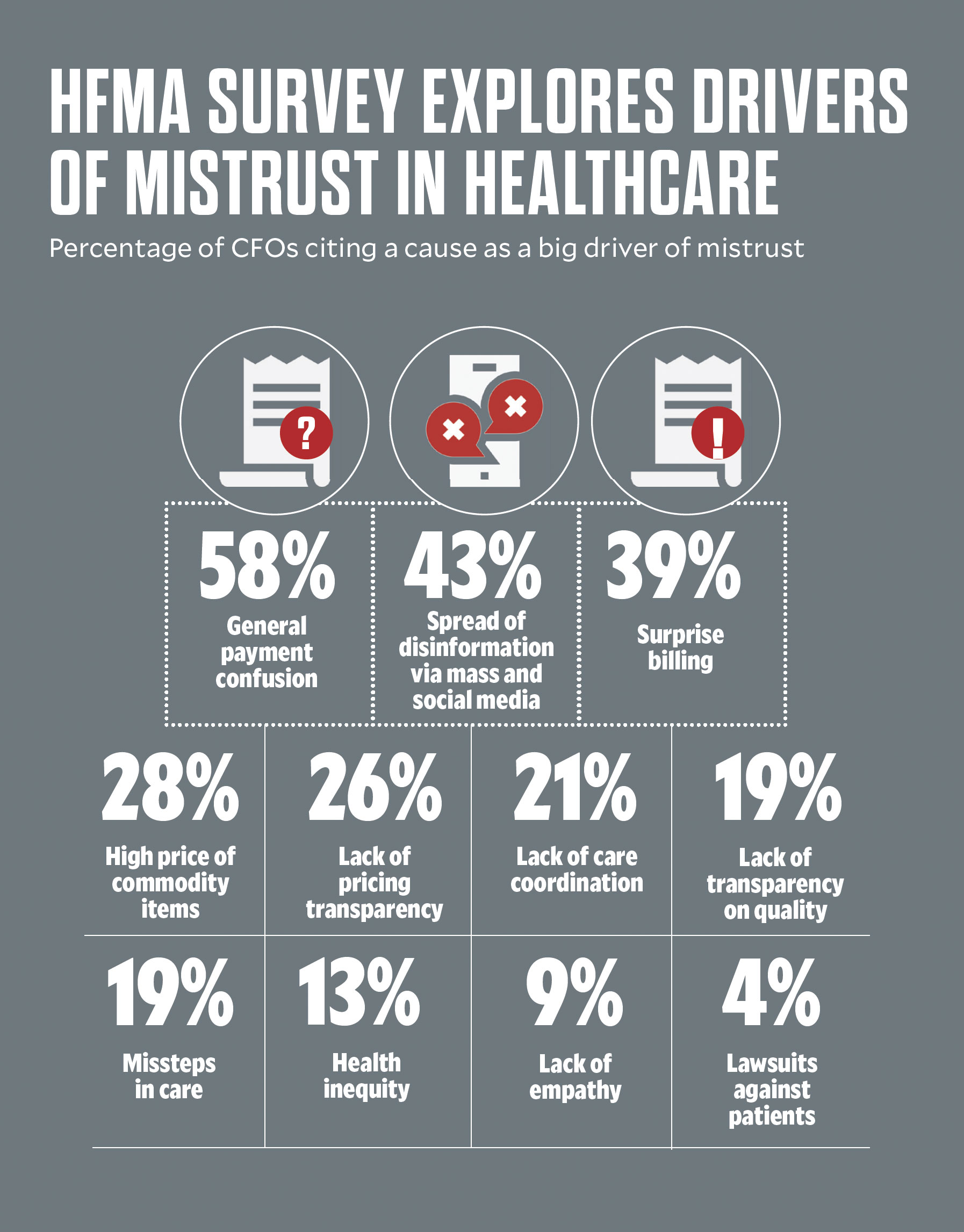
Among the biggest drivers of consumer distrust from healthcare leaders’ point of view are financial concerns: general payment confusion (58%), surprise billing (39%) and lack of price transparency (26%).
“We’ve certainly made affordability the burden of the consumer,” Gandhi said. “Healthcare is the largest component of [non-housing spending] for most families, and yet, while most industries moved rapidly toward a consumer orientation — where consumers know what to expect and how much a service will cost at each point in their journey — healthcare has been slower to adapt.”
Breakdowns in information sharing undermine the trust that patients have in their physicians, hospitals, health plans and other key stakeholders.
“There is frustration over the lack of a consumer orientation in healthcare and an inability to get consumers the information they need, including around cost, in a timely manner,” Gandhi said.
Misinformation lingers, inequities questioned
Healthcare organizations also continue to feel the impact of health misinformation during the pandemic. Four out of 10 leaders surveyed by HFMA cited the impact of the spread of disinformation on consumer trust. It’s an issue that affects not only whether consumers seek care, but also the morale of care teams and the efficacy of health interventions, including the public health response to the pandemic.
Evidence of health inequities, too, has sparked tough conversations about equity in care. A survey by the American Board of Internal Medicine Foundation found 59% of U.S. adults believe the nation’s healthcare system discriminates “at least somewhat,” and 49% of physicians who took the survey agree.

Mark Rukavina, program director for Community Catalyst
Meanwhile, an increasing number of women and patients of color are sharing stories of medical gaslighting or times when their conditions are dismissed as either minor or psychological in nature. They point to studies that show women wait longer for an accurate diagnosis than men and that people of color receive less care and poorer-quality care.
“For many people — people of color and historically excluded populations in particular — the pandemic brought to light disparities in care and structural racism that led to higher rates of COVID-19 infection and poor health outcomes from the virus,” said Mark Rukavina, program director for Community Catalyst, a consumer health advocacy organization. “This fueled huge trust issues among specific populations. While conversations around how to address these disparities are occurring across the country, solving this challenge will take time and input from multiple stakeholders.”
The individual’s role

Steven Edwards, former president and CEO of CoxHealth, headquartered in Springfield, Missouri
“Relationships of trust are built between individuals. In healthcare, trust has a lot to do with reliability: Whether we follow through with what we say we’ll do,” said Steven Edwards, who retired as of June 1 as president and CEO of CoxHealth, headquartered in Springfield, Missouri. Even when consumers question the reliability of science — such as whether to trust in the COVID-19 vaccine — or of the nation’s healthcare system, opportunities to strengthen care connections at the community level remain.
“I was at the hardware store recently when a man came up to me and told me the story of how he was able to get in to see one of our cardiologists within a day,” Edwards said. “He doesn’t believe in the COVID-19 vaccine or in healthcare in the broadest perspective, but he respects us deeply because we took care of him when he needed us most.”
For Some, Not A Problem
Still, nearly 40% of HFMA survey respondents believe consumer trust increased during the pandemic. Another 18% believe it remained unchanged. Among the comments received:
- “I do not agree that the mistrust is directed at healthcare, but mostly toward government, the CDC, politicians and media. Of course, this does not help us.”
- “I am not sure I agree with the distrust assertion, especially given our patient satisfaction scores. I do believe high cost to consumers (magnified by the shift of costs to the commercial markets due to below-cost government payments) and poor communication of why things are costly [are dissatisfiers].”
- “None of the above [possible reasons for declining trust] are true to our organization. Patients are actively and aggressively seeking care, and our organization is busier than ever.”
To reach the point where the bulk of consumers believe in their care teams and the systems that employ them, “we have to get back to that human, relational aspect of care,” said The Beryl Institute’s Wolf. “This means listening to patients, communicating with them in ways they understand and treating them with respect.”
So much of health outcomes achieved are driven by the personal connections that are created at the point of care, Wolf said.
Changing the trust outlook

Niyum Gandhi, CFO and treasurer, Mass General Brigham, Boston
Moving the needle on consumer trust requires leaders to rethink the ways they engage with their communities, said Rukavina of Community Catalyst.
“It starts with understanding the factors that stand in the way of trust and engaging organizations that help form the fabric of the community, from community organizations to faith-based groups to design solutions,” he said. “This helps ensure that underrepresented populations are carefully considered and represented in the types of innovations that are explored to improve access to care and community health.”
For example, at Trinity Health in Livonia, Michigan, the system created “social care hubs” to try to connect people in need with food, housing, financial assistance and primary medical care prior to the pandemic. When COVID-19 hit, Trinity directed more than $500,000 to these social care hubs to meet pandemic-specific needs and launched initiatives for mobile testing and vaccine outreach and education in underserved communities.
Leading organizations also draw on data from community health needs assessments in determining where to focus and what resources are needed for success, Rukavina said.
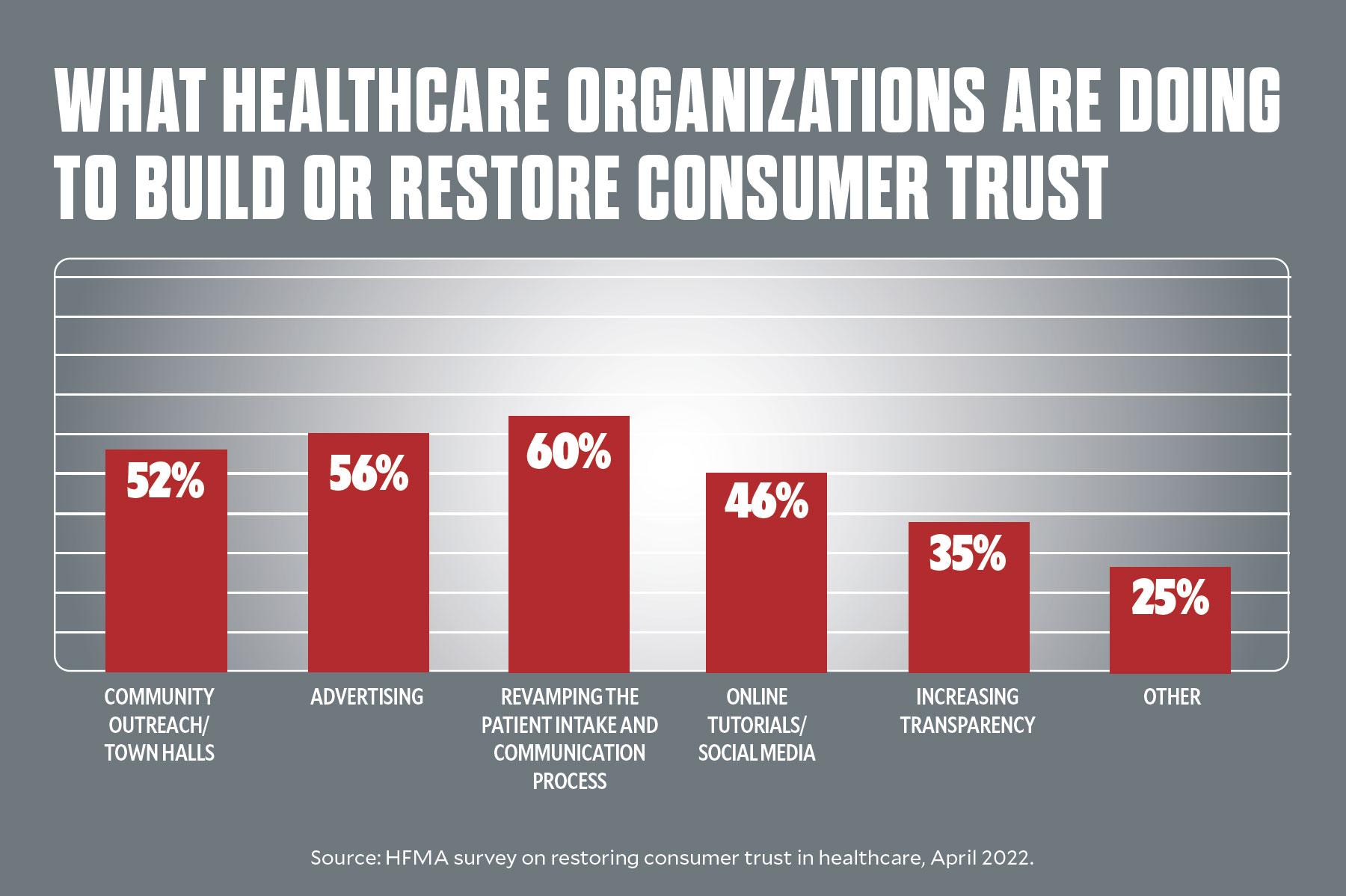
In that vein, healthcare organizations are ramping up initiatives to build or restore consumer trust, the HFMA survey shows. Initiatives run the gamut from community outreach and town hall meetings to redesigning the ways in which patients are communicated with and engaged. Also of strategic focus: increased transparency, including around healthcare costs.
Eliminating language barriers is an important part of this work as well. At Mass General Brigham, all patient-facing materials are translated into seven languages based on the needs of the population the health system serves.
“Ensuring that we can communicate with patients in an effective manner not only builds trust, but also helps patients get what they need,” Gandhi said. “Patients with whom we don’t communicate effectively tend not to advocate for themselves, and that leads to poor healthcare outcomes.”
For CoxHealth, the use of expanded communication formats during the first months of the pandemic established the health system as a trusted source of information. It also reminded the community of the health system’s purpose while providing greater clarity at a time of confusion.
“In healthcare, people’s motivations are so woven into the fiber of who they are that we’re best served to remind [our communities] why we’re here,” Edwards said. “It gives people a better understanding of why we do what we do, which helps restore trust.”
5 WAYS TO RESTORE CONSUMER TRUST
For hospital and health system leaders, maintaining or restoring consumer trust starts with foundational aspects of patient engagement, communication and access. Here are five actions to consider:
1. COMMUNICATE WITH CONSUMERS IN THEIR PREFERRED FORMAT
“Start by asking, ‘In what language would you like to be communicated with?’” said Jason Wolf, president and CEO of The Beryl Institute. Then, dig into consumers’ preferred communication vehicles — from text to email to paper-based communications — as well as how frequently they wish to receive communications and from whom (for example, from the health system or a primary care provider).
2. HELP PEOPLE BE WELL OUTSIDE THE FOUR WALLS OF YOUR ORGANIZATION
The year 2021 marked a breakthrough in digital health funding, and experts predict it will propel transformation in care access and chronic care management and a rise in nontraditional entrants in the healthcare space. On the one hand, disruptive providers hold the industry more accountable, said Steven Edwards, recently retired president and CEO of CoxHealth. They also make healthcare better by acknowledging why a different approach to care could improve value for patients.
3. COMMIT TO CARE TEAM WELL-BEING
“We cannot isolate the patient experience from the workforce experience from the community experience,” Wolf said. By focusing on ways to effectively manage burnout and build resilience among care teams, hospitals and health systems ultimately will create a better atmosphere for patient care and also retain some of the 50% of care team members who are considering leaving the profession due to unrelenting stress.
4. TAKE ACCOUNTABILITY FOR FINANCIAL COMMUNICATION BREAKDOWNS
“When a patient complains about something related to a healthcare bill, it doesn’t matter whether the issue is the health plan’s fault or the hospital’s fault or a provider’s fault. Collectively, we have let the patient down,” said
Niyum Gandhi, CFO at Mass General Brigham. “While the natural tendency might be to say, ‘Oh, based on this technicality, this isn’t a covered service, and you need to pay a copay,’ this doesn’t help to build trust.” A better approach is to focus on solving the problem, such as by coordinating with the health plan in a different way. This assures consumers that you are taking accountability for the solution. It also provides consumers with the level of service they have come to expect from other industries — and that they deserve from their healthcare provider.
5. PAY ATTENTION TO THE PERCEPTION OF ACCESS — TO CARE PROFESSIONALS, SERVICE REPRESENTATIVES AND THE ORGANIZATION ITSELF
“As health systems have gotten larger, some of the control of hospitals and health systems has moved from the community to other places,” said Mark Rukavina, program director with Community Catalyst. “This makes it challenging for people to understand who to contact when they have questions. It leaves residents feeling as if they have lost control of their community hospital, and that’s a real issue for some people.”










