Reducing Clinical Variation to Drive Success in Value-Based Care (Part 1)
It is well-known throughout the business world that variation and a lack of standardization lead to poor quality and higher costs. The same is true in health care, whether the issue is an episode of care around a surgical procedure or long-term management of chronic disease.
Standardized care that reduces clinical variation—defined here as the over-, under-, or unnecessary utilization of healthcare services and resources—has been shown to improve quality and outcomes in the ambulatory, acute, and post-acute settings. Thus, care standardization is a vital aspect of organizational efforts to improve care under value-based contracts.
What’s at Stake
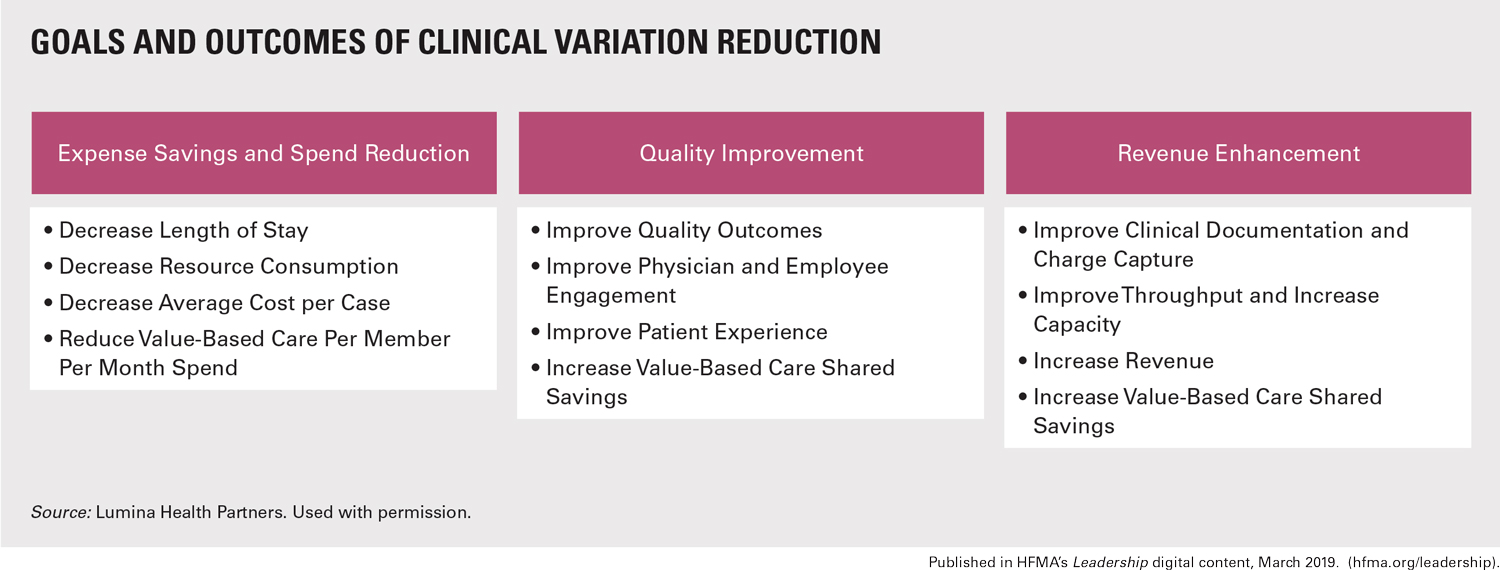
The exhibit below summarizes the wide array of longitudinal improvement opportunities across the continuum of care that are available through clinical variation reduction.
Exemplifying the importance of reducing variation, the use of protocol-driven care in the ICU has been observed to lead to a significant reduction in healthcare-acquired conditions. Although poor performance in this area partially can be attributed to issues with clinical documentation, wide variation in care exists across the continuum—especially for certain serious conditions such as the recognition and aggressive treatment of sepsis.
Clinical variation affects the value of care in other ways, including:
Costs. Unnecessary clinical variation leads to increased costs, as seen in many surgical procedures and the encompassing episodes of care. Factors that influence and elevate costs include the use of unnecessary preoperative testing, physician preference decisions that increase implant costs or extend operating-room time, and a lack of standardized postoperative care that leads to prolonged lengths of stay and inappropriate use of post-acute resources.
This failure to standardize the coordination of care has also led to unnecessary emergency department visits and hospital readmissions. The wasteful and imprudent use of diagnostic and therapeutic resources is also monitored in the ambulatory setting, and at least one vendor is offering insurers comparisons of providers using a value-of-care index.
Patient experience. Standardized care, coupled with strong provider engagement and communication, is a patient satisfier. Patients and their caregivers rely on the healthcare system to provide the “standard of care” with reliable outcomes at reasonable costs. Discussions around evidence-supported treatments allow patients to feel better informed, and such talks create a high level of trust in the proposed therapeutic solutions.
Standardized care may not always lead to desired outcomes or completely avoid complications. But the communication and reinforcement of the appropriateness of therapeutic choices will support confidence in the care team and reduce the chance of frivolous litigation.
Strategies to Reduce Variation and Improve Value
The exhibit below highlights the four essential components of a change program to identify and reduce clinical variation. These four components are prerequisites to successful implementation of changes in clinical processes and provider behavior. They are interrelated and interdependent, each with multiple iterations.

In this article, we examine the ideal strategies for physician engagement and risk-adjusted analytics. Next month, we’ll look at utilization of physician scorecards and evidence-based best practices.
Physician engagement. Value-based care offers new opportunities to engage physicians in clinical performance improvement activities. The Quality Payment Program, Medicare Shared Savings Program (MSSP), and other government and commercial payment initiatives are offering new incentives for physicians to actively engage in efforts to increase value.
Health system leaders should engage and educate physicians regarding these incentives and make sure they understand the benefit to patients and the organization. To drive accountability, physician and executive leaders should communicate their expectations, goals, and related measures, as well as collaborate to ensure that incentives are aligned in support of the clinical variation reduction effort.
Physicians and other providers should participate on interdisciplinary teams to:
- Review risk-adjusted analytics
- Select episodes and populations with opportunities for improvement
- Incorporate evidence-based best practices
- Implement new clinical practices, order sets, and protocols to reduce variation
Senior medical leaders and executives should use a style that is supportive and collaborative when engaging physicians, holding them accountable to their vision. Leadership also should actively participate in celebrations of success and distribution of rewards.
Risk-adjusted analytics. Physicians are data-driven; it is in their DNA as scientists. They must be presented with reliable, accurate, and risk-adjusted data by DRG, clinical cohort, or another relevant patient-population classifier.
Deployment of risk-adjusted analytics reduces physician resistance and increases their buy-in to identifying and reducing variation. For example, the All Patients Refined Diagnosis Related Groups methodology groups patients into four levels each of illness severity and mortality risk. Most physicians will not come to the table to discuss their population without this type of risk adjustment.
Analytics should be deployed to help physicians see how changes in their clinical practice patterns influence targeted measures. Three common categories of variation can be improved through changes in clinical practice and physician behavior: clinical resource utilization, length of stay, and clinical documentation. Improvements in each of these areas can result in significant expense reduction and quality improvement, as well as improvement in per member per month (PMPM) spend, which drives shared-savings opportunities in value-based care.
Part 2:
The authors examine how physician scorecards and evidence-based best practices factor into efforts to reduce clinical variation.





