Health plan data helps physicians, but additional insight would improve outcomes
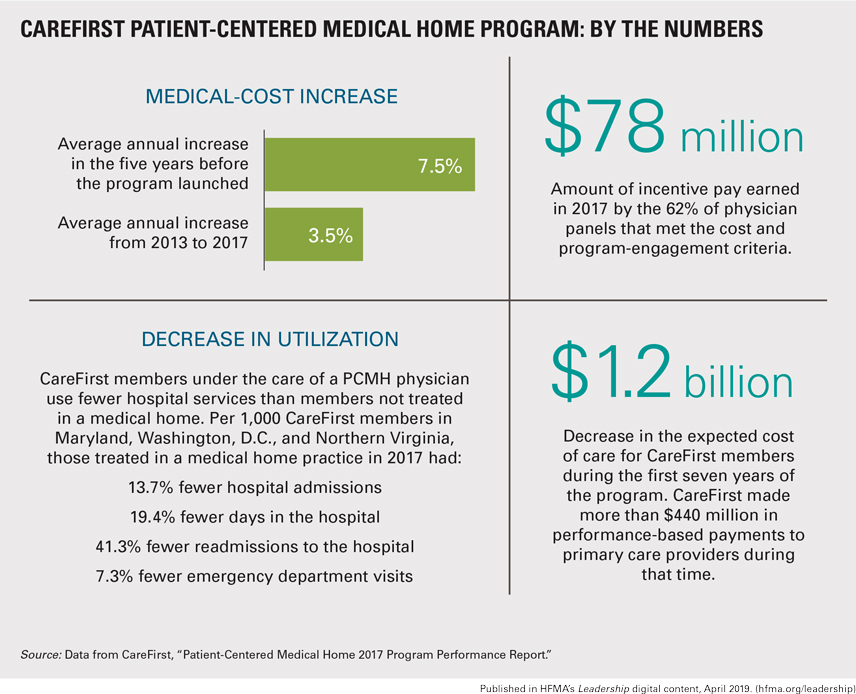
As health plans experiment with an array of value-based contracts, one of the first such models, the patient-centered medical home (PCMH), has proven itself over time. Among many PCMH success stories, CareFirst BlueCross BlueShield in Baltimore reports that its program helped save $223 million against the expected cost of care in 2017.
Nearly 4,400 physicians and nurse practitioners — approximately 90% of all primary care providers that are part of the health plan’s Mid-Atlantic service network — took part in the CareFirst PCMH in 2017. They are grouped into “panels,” typically with between five and 15 providers per panel, as part of their participation.
The panels are organized to coordinate the care of patients with the most complex needs. Panels can earn financial incentives based on quality metrics and savings against projected costs for attributed patients.
Rockville (Md.) Internal Medicine Group has participated in the CareFirst PCMH program since its inception in 2011. “Overall we’ve had a great working relationship with CareFirst through this program,” says Shishir Khetan, MD, a partner in the practice. “It’s evolved over the years, so it seems like they’re listening to providers, and that’s good news for us and our patients.”
Rockville Internal Medicine Group is part of Privia Medical Group, which has about 425 providers participating in the program.
How data supports care delivery
Because each provider panel is evaluated on the total cost of all healthcare services a patient receives, providers have a financial incentive to encourage their patients to make high-value choices. Khetan shared two examples of how providers at Rockville Internal Medicine help patients select low-cost, high-quality options.
Reducing pharmacy costs where possible. Khetan and his colleagues review patient information to identify those with high drug costs. Patients who need medication for chronic conditions, for example, might benefit from using a mail-order pharmacy, which will lower their costs.
When it is clinically appropriate, providers may also encourage patients to try a generic drug as an alternative to a higher-cost brand-name drug. For high-cost drugs without a generic equivalent, providers may be able to recommend trying a lower-cost alternative.
Ranking specialists on cost. CareFirst provides a color-coded list of specialists to make it easy to see which ones rack up the highest expenses. Some specialists are high-cost for a valid reason, Khetan says, but he and his colleagues consider other factors.

“They could be working at a hospital that is more expensive compared with other options in the area, or the specialist could be one who prescribes a lot of expensive drugs or orders a lot of tests that aren’t always necessary,” he says. “We look at that data to see if it’s appropriate to educate our patients about lower-cost, high-quality options.”
Rockville Internal Medicine Group combines CareFirst’s specialist cost rankings with its own quality assessments to identify preferred specialists. CareFirst does not provide data on the quality of clinical care provided by specialists, so Khetan and his colleagues consider three factors:
- Outcomes as reported by patients. “If it’s a surgeon, we consider how often our patients are having complications,” he says. “We generally have a feeling of that information based on feedback from our patients.”
- Communication. If the specialist does not communicate promptly and thoroughly with the primary care physician who made the referral, that’s a red flag that patients may encounter problems if they need to contact the specialist with follow-up concerns or questions.
- Specialists’ practice habits. “With the information provided by CareFirst, we have the ability to compare utilization patterns, such as how often other providers in the same specialty order certain tests or procedures,” Khetan says. “This insight helps us select specialists who best align with our patients’ care plans.”
Limits to the usefulness of data
Khetan and his partners appreciate getting data from a health plan. But the CareFirst program performance reports, like data received from other health plans, are not immediately actionable for three reasons (CareFirst did not respond to requests to comment for this article):
The time disconnect. Given the time needed for the health plan to process claims and analyze the data, providers may lack the information they need to make adjustments that could improve their performance for a specific time period.
“When the data is delayed a minimum of three to four months, it becomes hard to use that data when you’re being measured on a calendar year,” Khetan says. “We’re always lagging a little bit behind.”
Uncertainty about data details. Providers are accountable for all costs their patients incur, but because the reports from CareFirst are summarized, it’s hard to make a direct correlation between a physician’s decision or recommendation and the total cost of a patient’s care.
Uncertainty about risk adjustment. Each provider panel receives a budget target that is supposed to reflect the number and relative medical complexity of patients for whom they are responsible. But the providers don’t know how a patient’s risk score is calculated, so they are not confident that the risk adjustment — and thus the budget — accurately reflects their patient population.
That disconnect makes it difficult for a practice to predict the amount of performance incentives it will receive from the health plan, and thus to manage its business and devote more time to preventive care. “There’s a lot of variability from year to year in these incentives, and that makes it very tough for practices to plan their budget based on what they think they might get in the future,” Khetan says.





