How Spectrum Health achieved a $64.3 million margin improvement
In late 2017, Spectrum Health was ripe for transformation. Despite struggling with several major issues, the integrated, not-for-profit health system in Western Michigan saw potential for better things to come. The optimism, in part, was due to a newly implemented electronic health record (EHR) system, making it a perfect time for change.
Key issues that had to be overcome included:
- The organizational structure in the revenue cycle department was fragmented and did not have clear accountabilities.
- Accounts receivable (AR) days had spiked to 70 days, with discharged not final billed (DNFB) accounting for almost 12 of those days.
- Denial rates for claims were well above the industry median at 13%.
- Patient collections were lagging.
- A lack of confidence in the revenue cycle on the part of the physician organization had led to a fractured relationship.
What transpired was an ambitious initiative that included leaders from across the organization and garnered Spectrum Health a $64.3 million margin improvement and an HFMA MAP Award.
Opportunity analysis and program setup
To start, the health system initiated a comprehensive current state assessment of the revenue cycle, both hospital and professional, to understand the operational, business process and technology opportunities to improve the overall program, and the associated financial improvements that would result. A data-driven assessment analyzed 12 months of claims to understand where net revenue opportunities existed. Additionally, the study reviewed opportunities for improvement in organizational structure and staffing, the EHR module footprint and configuration and the current business processes and workflows.
The assessment identified $58 million to $102 million in recurring net revenue benefit and $59 million to $83 million in one-time cash acceleration across 10 priority opportunity areas.
The organization prioritized revenue cycle optimization among competing organizational initiatives and embarked on a two-year transformation program beginning in June 2018, targeting $25 million in net revenue improvement for the first 12 months of the project. The targeted nature of the assessment allowed Spectrum to be strategic in the implementation priorities and capitalize on the areas with the highest return first. The opportunities touched the front, middle and back of the revenue cycle and required intense collaboration among leadership across the organization.
Next, revenue cycle leadership, assisted by the change management advisers, conducted stakeholder and impact analyses for each opportunity area, looking more closely at what it would take to drive adoption and a successful transition from a people perspective. The analysis enabled the revenue cycle leadership to reach a common understanding of the change management effort required, how each opportunity area would impact different stakeholder groups, and the best engagement tactics and messaging for each group, given their unique goals and concerns. Heat maps and other visuals were created to keep track of the various moving parts from a stakeholder point-of-view, helping to ground the team in key information, such as who should be engaged earlier versus later and more heavily, and on what topics.
A dedicated communications team helped create standard presentations, talking points and FAQ documents so that leaders could efficiently and effectively speak with one voice as the work ramped up. Also, special emphasis was placed on articulating the “why” for significant changes so those affected would have a strong understanding of the rationale for the change and expected benefits.
Spectrum’s change management approach, adapted from a strategy described in the book, Change Rx for Healthcare, focused on leaders being active and visible in three key roles: story teller, barrier buster and spark of energy.
According to the book, a storyteller uses relevant and impactful stories to manage change and transformation. Stories can illustrate the importance of an initiative and inspire people to join the change mission by creating awareness and connecting the change to what they desire most. A barrier buster resolves conflict, removes barriers that hinder impactful change and effectively manages resistance by building trust and rapport through engagement and collaboration. Lastly, a spark of energy inspires and motivates people to embrace change by championing change, exhibiting positivity and modeling transparency and consistency.
Following are a few examples of how Spectrum put those roles into action.
1. Storytellers
One workstream focused on improving patient access through an evolution of the current operations of an existing patient access service center. The idea was to incorporate centralized authorizations for priority specialty areas, starting with case-based procedures, which the process brought under control elevated denial levels and avoidable adjustments.
The changes positively impacted both revenue and patient experience.
At the beginning of the initiative, 42 decentralized medical group practices were responsible for obtaining authorizations for their own cases. Surgeries and other high-dollar services were scheduled without an authorization. The lead time from scheduling to date of service did not always allow enough time to secure an authorization, and there was no process to identify the services that could be medically deferred to allow more time for the account to financially clear. Implementing a case-based authorization center of excellence as a part of the patient access service center with changes to technology, processes, staffing and patient experience was a heavy lift due to the number of stakeholders that had to be engaged. Storytelling was an important way of getting all stakeholders — leadership, physicians and staff at 42 locations — aligned quickly.
Two leaders within the patient access area developed a plan to conduct a communications and engagement blitz. A case-for-change presentation was prepared and included statistics and data on the extent of the problem, the solutions desired and the plan to make the transition. The duo set off to tell their story over a period of several months, visiting most of the locations for face-to-face meetings, a few on multiple occasions. Their perseverance paid off as they were able to transition staff from clinic locations to a centralized team and launch the associated process and technology changes successfully within the planned time frame. Most important, visiting the clinics personally to champion the solutions helped to build trust at the various locations with operational and clinical staff, building the foundation for future collaboration to drive improvements together.
2. Barrier busters
Changes in the middle revenue cycle were complex and difficult to explain to busy physicians across the organization. Multiple workstreams were driving improvements to coding accuracy, clinical documentation and practices driving DNFB, all requiring physician understanding and cooperation. Multiple teams that support physicians daily with coding, documentation and revenue cycle education issues needed to be on the same page and understand the big picture so they could guide physicians in a coordinated fashion. It was imperative that they were prepared. A clinical documentation integrity (CDI) center of excellence was created to allow CDI personnel to collaborate with clinical stakeholders to share key performance metrics and recommend action plans focused on people, process and technology. Transparency in data sharing to monitor progress and maintain a complete line of sight into whether CDI activities were achieving goals was critical to staff, provider and leader engagement. Leveraging technology and process changes to capture documentation needs at the point of origin allowed for optimization of the CDI staff and provider rounding experience. The goal was to focus on as much real-time technological assistance and CDI education as possible, while reducing the need for coding queries that contribute to DNFB. Members of several teams were surveyed to gauge their understanding of key aspects of the desired future state.
3. Sparks of energy
The patient liability management workstream, also driving change in the front of the revenue cycle, required hundreds of patient service representatives to begin collecting co-pays at the point of service with the aid of new technology. The changes also involved improving the referral of patients to financial counseling early in the process with the help of a new financial assistance module in the EHR.
Patient service representatives are entry-level hourly staff, making consistently effective engagement difficult for changes that impact them. Talking about money is not natural for most of these representatives, but they needed to become comfortable having financial discussions with patients and families on a regular basis. Because of the difficulties those changes represented, leadership worked to involve patient service representatives to help them buy in to the process.
Amid a series of trainings, with participation averaging 75 to 100 people per session, a workshop was also held where representatives from the patient service representative staff helped to analyze impacts on their role and their day-to-day work, provided feedback on scripting and messaging to patients and weighed in on training programs and job aids. The spark of energy provided by dialogue in the workshop buoyed the staff as they learned new processes, technology and abilities for communicating with patients on challenging financial topics.
Results
The result was active engagement between information services, operations and the physician organization as was required to implement and sustain the desired changes. Organizational and leadership changes were made across the revenue cycle to support the transformation efforts and improve the culture. Due to the joint effort of all the different stakeholders, Spectrum Health was able to see financial gains as early three months from the launch of implementation efforts.
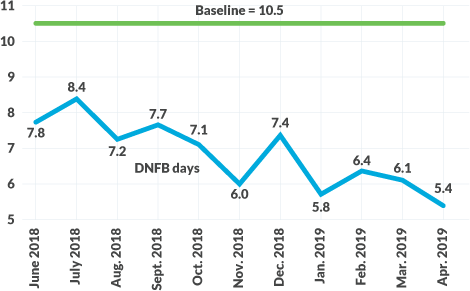
Since the beginning of this project, Spectrum Health has seen a steady decrease of DNFB days and AR days, as shown in the exhibits below. The decrease in DNFB days from 10.5 to 5.4 can be attributed to a daily monitoring program that promotes improved visibility and accountability across organizational stakeholders.
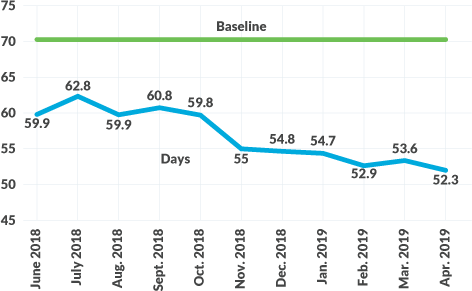
The large decrease in AR days for hospital and professional billing (70 days to 52.3 days and 47 days to 38.9 days, respectively) can be attributed to several key interventions, including reorganization of the billing and follow-up staff, optimization of the EHR work queues, leveraging of automation for account follow-up and strategic outsourcing of certain functions.
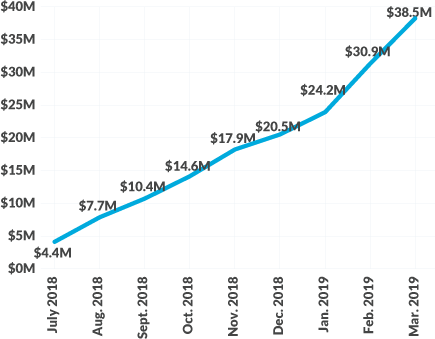
On the net revenue improvement front, results have been well above expectations. For FY19, the effort yielded $64.3 million in margin improvement versus the original projection of $25 million, as shown in the exhibit below. Through the combination of its 10 priority initiatives, Spectrum Health has enjoyed almost $64 million in net revenue improvement on an annual basis, which will only grow over the coming months as the initiative continues.