Strategy, technology and tactics for sustainable performance improvement
Key takeaways from the Kaufman Hall/Axiom third annual state-of-performance-improvement survey of hospital and health system leaders are that incumbent health systems:
- Face a changing business model as care migrates out of the inpatient setting.
- Need to address increasing cost pressures as a tight labor market drives wage inflation.
- Should focus on improving performance and transforming cost to support new strategic investments.
To ensure success, these initiatives must be based on reliable data, enhanced by external perspectives and benchmarking, supported by engaged clinicians and monitored through clear lines of accountability.
Cost transformation now in focus, but targets remain low
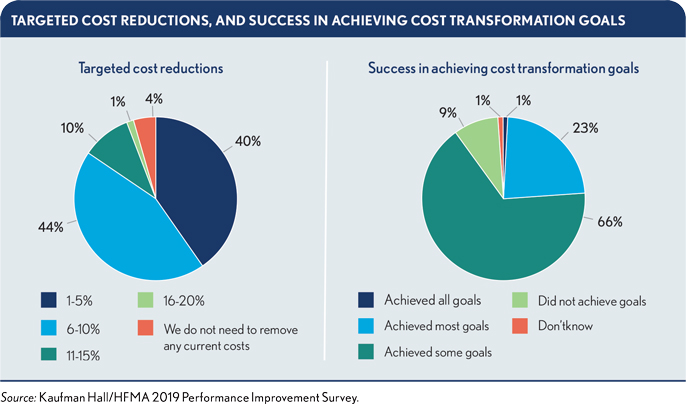
The good news in this year’s survey is that respondents indicate their organizations are taking cost transformation more seriously. Only 4% say their organizations have no need to remove any current costs. At the same time, fewer than one in four respondents say they have achieved “most” or “all” of their cost transformation goals. Targeted cost reductions remain modest, with 40% of respondents saying their organizations’ targets are between 1% and 5% of current costs, far below what most health systems will need to break even on Medicare payments.
Pressures on revenue and expenses intensify; need to dig deeper
Flat or declining inpatient volumes, identified as the greatest pressure on revenues by 30% of survey respondents, are an indicator of the ongoing shift to care provided beyond hospital walls. This is the tip of the iceberg. Health systems must invest in strategies that radically reform their cost structures and enable them to compete on access, convenience and price in a rapidly changing healthcare market.
The pressure to invest in strategic initiatives is acknowledged, but rising labor costs are putting significantly more pressure on the bottom line. Rising salary and wage inflation was identified as the greatest expense pressure by 47% of respondents. This underlines the need to push beyond traditional labor, productivity and supply chain initiatives.
Performance improvement needs
With two-thirds of respondents managing to achieve only “some” of their cost transformation goals, clear needs exist for more reliable processes and better tools in performance improvement. The survey findings indicate that these needs include the following:
- Better data and insights, including comparative insights for peer organizations
- Better information for improved physician engagement
- Stronger culture of support for achievement of performance improvement goals
- Greater accountability for results
Strategies and successful practices for performance improvement
To address the needs identified in the survey, health system leaders should focus on the following four key strategies.
Strategy 1: Refine and improve understanding of costs.
Future growth will occur outside hospital walls, where incumbent health systems face increased competition from new market entrants such as CVS Health and Walmart. Health plans also are positioning themselves to be the organizers of healthcare networks and will use unit price as a key factor in selecting preferred network providers. Effective competition will depend on a more granular understanding of the actual costs required to offer a service or procedure. Three practices are key to success with this strategy.
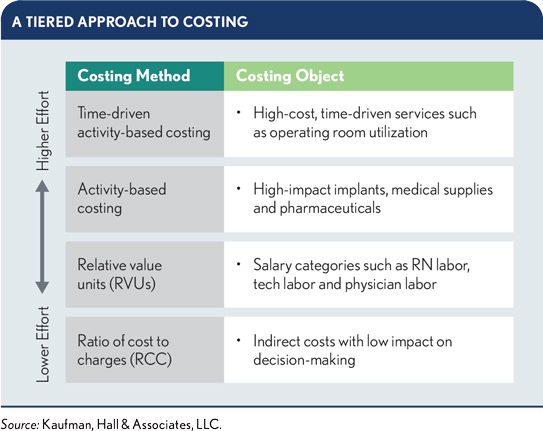
Adopt a tiered approach to costing. Organizations pursuing a more detailed understanding of costs should adopt a tiered approach that matches intensity of effort with items that have the highest impact on decision-making. The most resource-
intensive method — time-driven activity-based costing — is used at the highest tier for high-cost, time-driven activities. At the lowest tier, a traditional ratio of cost-to-charges approach can be used to allocate expenses in areas that have little impact on decision-making.
Adjust calculation frequency. As finance leaders adopt more detailed costing methods, they also should consider the calculation frequency and costing time period. A move from year-to-date to monthly or quarterly costing will improve opportunities for trending and process efficiency.
Improve the cost accounting system. The end goal is a cost accounting system that enables reporting across the care continuum and across multiple financial functions as well as produces information that health system leaders can stand by and act on.
Strategy 2: Deploy external perspectives and benchmarking to identify and drive sustainable cost restructuring efforts.
Competitive positioning requires beating competitors on price and performance. To identify areas that offer the most potential gain and gauge whether they are setting the bar too low or too high, healthcare leaders first must understand how processes can change and how peer organizations are performing. Successful practices with this strategy include the following.
Bring in fresh eyes. Outside experts can bring in new perspectives and provide an objective, consistent third-party view across a system.
Use external benchmarking to establish an outside view. External benchmarking supports health system leaders in setting targets that push their organizations to optimize performance, while also reflecting informed assessment of realistic opportunities. It also provides actionable data to identify and address challenges as they emerge.
Learn from experience. An organization’s own experiences provide an important reference point. As an organization’s experience grows, so too will the value of internal benchmarking data that demonstrate how often and how closely the organization was able to achieve expected returns.
Strategy 3: Engage clinicians with accurate and actionable data on quality and costs.
An organization’s ability to generate consistently high-quality, cost-effective outcomes is a crucial differentiator for consumers and payers alike. Transformative health system change simply is not possible without engaged physicians, but only 14% of respondents indicate their clinicians have access to actionable information to help them address unwarranted clinical variation and other cost-related quality concerns. There are many opportunities to use improved analytics to better engage physicians.
Involve physicians early. Physicians should be involved in selecting the systems, tools and metrics a health system uses to collect and display clinical data in outcomes reports.
Build trust in the data. Be transparent about data sources and what these sources do and do not provide. Seek consensus on sources most relevant for different practice areas and specialties.
Anticipate and address common concerns. Physician concerns include the adequacy of severity or risk adjustments and proper attribution of patients.
Focus on developing a single source of truth for physician data. Focus on developing a clinical analytics solution that can aggregate data from disparate sources and systems into a single source for clinical cost and quality data.
Enable comparisons with peer groups. As trust in the data grows, enable physicians to compare their performance with peers, beginning with internal peer groups. Physicians whose performance is falling below their peers typically are eager to close the gap.
Be consistent with expectations. System executives must establish expectations for appropriate behavior and ensure that necessary actions are taken if performance expectations are not met.
Strategy 4: Establish greater accountability for achieving performance improvement goals.
Forty percent of respondents are targeting cost reductions of just 1% to 5% of overall costs, and most respondents are achieving only “some” of their cost transformation goals. A mixture of moderate goals and moderate success does not result in the transformative outcomes the current healthcare environment demands. Three practices are essential for success.
Build a culture of accountability. Accountability ultimately is a question of culture, defined by an organization’s ability to unite around common goals, and by the willingness of stakeholders organizationwide to take ownership of and responsibility for performance results.
Establish a results management office. A results management office (RMO) establishes a structured approach to accountability throughout the organization, providing a range of change management and support services to performance improvement teams. While an RMO and its staff help facilitate change, accountability remains with the team and its designated operational leaders.
Implement a strategy management solution. An effective strategy management solution should enable stakeholders throughout the organization to easily track progress, and drill down to investigate possible causes when progress stalls or begins falling behind targeted milestones.
Facing the future
To prepare for the future, a commitment to continuous performance improvement is imperative. Opportunities will change and differ from organization to organization, but the strategies discussed in this article are applicable across all organizations. They are designed to help make health system leaders better informed, more accountable and more able to drive change within their organizations. Supported by successful practices that combine performance-improvement tactics and technology, these strategies will help leaders set appropriate goals and build a culture of accountability and engagement that optimizes the chances for success.
Read the full report
Kaufman Hall/Axiom partnered with HFMA in fielding the survey and analyzing the findings described in this article. It was the first time HFMA joined Kaufman Hall/Axiom on this annual effort. Download the full report.






