Electronic Claim Processing Can Save Millions of Work Hours
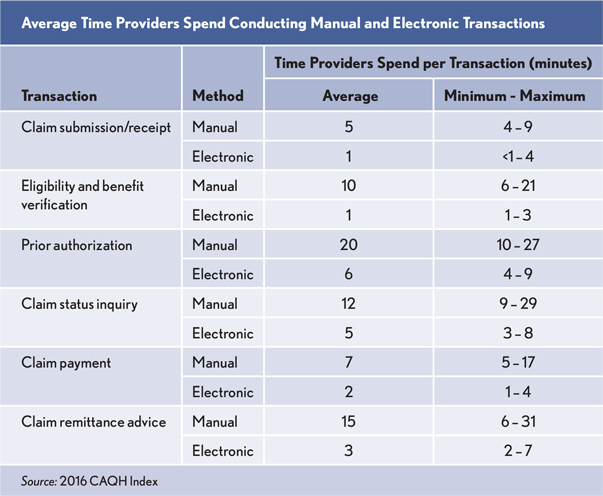
If providers fully adopt automated processes for claim transactions reported in the chart (see exhibit), a minimum of 1.1 million hours of administrative work could be saved per business week each year, according to a 2016 CAQH study.
Providers spend an average 8.5 more minutes conducting manual transactions compared with electronic transactions. This time difference can be as high as 29 minutes, depending on the transaction type. Processing for a single claim that required one of each of six transactions electronically instead of manually could save a minimum of 51 minutes.
For eligibility and benefit verifications and claim status inquiries, the time estimates include both transmission of the transaction and receipt of a response. For the other transactions, the time does not include additional follow up, such as managing claim denials, responding to health plan requests for additional information, or sending attachments.