Budgeting for healthcare technology is not just a numbers game
U.S. hospitals and health systems are eschewing top-down technology budgets in favor of a collaborative, needs-based budgeting approach.
In recent years, the healthcare industry has seen a rapid proliferation of new technologies with promising healthcare applications. This trend has created a challenge for most U.S. hospitals and health systems, given their severe budget constraints, in deciding which of these new technologies constitute the best investment options for their organizations.
Add to their technology investment challenge the need to invest in cybersecurity — a need that the recent cyberattack on the vendor Change Healthcare has made even more compelling — and the decision of where to allocate limited dollars in tight budgets becomes all the more daunting.
It’s also not simply a matter of looking at how much was spent the previous year and then adding X percent to account for inflation. The demands for technology are too variable and are too much in flux to allow for such an approach.
The intricacy of budgeting for technology

The challenge of budgeting for technology is exacerbated by the fact that the needs for specific technologies are intricately connected to the needs of each department or area within a health system.
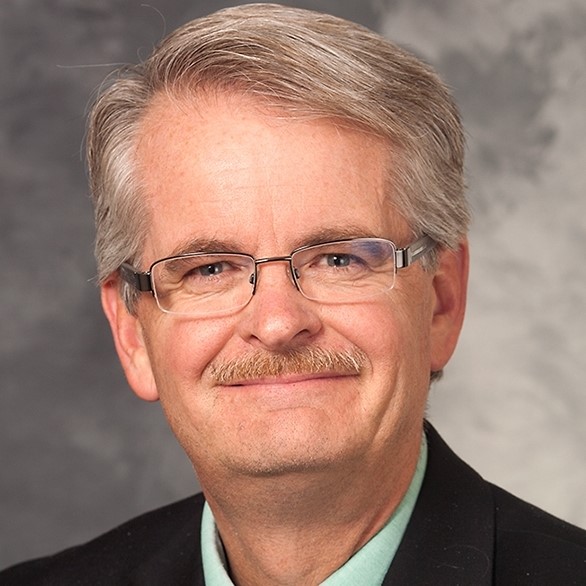
“I don’t know that technology can be a bucket. It’s interwound with everything we’re doing,” said Jim Kanuch, MBA, CHFP, CFO and vice president of finance for Atlantic General Hospital in Berlin, Md. “All pieces of our equipment interplay within some level of connectivity to our network or to the EMR. It’s just a part of life and where we are.”
With growing demand, a team approach is needed
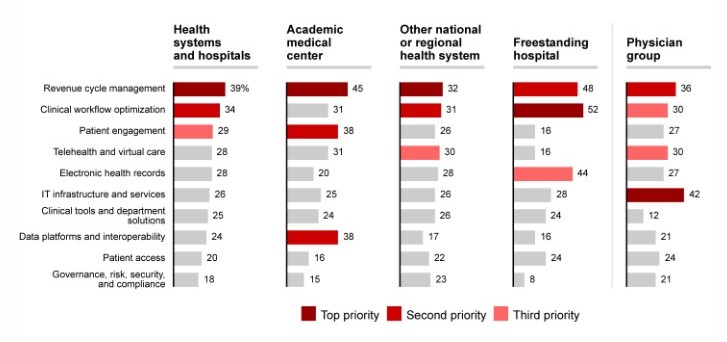
According to a June 2023 survey by Bain & Company and KLAS Research, nearly 80% of hospitals and health systems materially increased IT and software spending from 2022 to 2023, and about 75% expect to make “more” or “far more” investment in 2024.a
Freestanding hospitals and physician groups are catching up in key IT areas
Percentage of respondents citing IT as an area of priority (n = 201)
Surveys tracking such investments may simplify technology as a single investment category, but the reality is increasingly complex.
On top of a refusal to be line-itemed, every technology stakeholder has an opinion, a wish list and a strong sense of urgency. This energy around new technologies can be simultaneously inspiring and intimidating. When every option is presented as a “must have,” how can finance leaders determine which option is best to pursue?
To begin to do so, finance leaders should have a solid objective basis for understanding the needs across the enterprise, and they should approach the assessment of potential options collaboratively rather than try to make the decision alone. Simply put, finance leaders should take three fundamental steps:
- Understand organizational priorities
- Partner with other system leaders
- Promote collegiality by engaging department leaders in an organizationwide approach
1 Understand organizational priorities
For finance leaders, the primary objective should be to ensure every technology investment matches a declared organizational priority. They therefore should start deliberations about each requested technology investment with the question, “Is this strategic?”
Before beginning to evaluate any technology, the CFO must have clear visibility into needs across the organization and fully developed protocols for identifying, evaluating and collaboratively prioritizing those needs.

“We try to stay disciplined in setting priorities and focus our investments on items that align with those priorities,” said Stephanie T. Wells, CPA, CPC-A, system vice president, revenue cycle/HIM, Ochsner Health System, New Orleans.
Examples of priorities Wells listed include promoting patient access, ease of practice, administrative efficiency, remote management and the effective use of data and analytics.
Ochsner’s finance team addresses challenges within those priority areas with the support of the organization’s information systems/digital division, led by Denise Basow, MD, who Wells credited with helping the finance team avoid getting tunnel vision for a single tool.
“Dr. Basow’s preference is that we come to the governance committee with the issue for discussion rather than us coming to them with a vendor,” Wells said. “[Together] we are looking for solutions to identified challenges that we prioritize solving versus getting wowed by products that are a solution looking for a problem.”
A rubric for assessing technology investment options
John Halamka, MD, president, Mayo Clinic Platform and cofounder of the Coalition for Health AI, described the following rubric he developed as a CIO collaborating on technology budgeting with CFOs:
- 1 Is it strategic? It may be really cool tech, but what is the imperative, and is it addressing a current need?
- 2 Is there a quality or safety imperative? Don’t become the healthcare institution of lesser quality by standing still.
- 3 Is there a compliance or regulatory mandate? If something could result in an action against you, pay attention.
- 4 What’s the impact factor? Do what impacts more patients, providers, social workers and other stakeholders.
- 5 Is there a revenue impact? Is there a cost reduction or significant impact to profit and loss [P&L]?
2 Partner with other system leaders
At UW Health in Madison, Wis., CFO Robert Flannery, MBL, meets regularly with CIO Cherodeep Goswami, MBA, who encouraged the health system to think of technology’s role in terms of three buckets: “running the business,” “growing the business” and “transforming the business.”
“When we first started this, a lot of our dollars were in ‘run,’” Flannery said. “But as investments created efficiencies or costs were taken out, those dollars have been shifting to ‘grow’ and ‘transform.’”
Similarly, Carol Olff, MSN, RN, CCRN-K, director of critical care services at Concord Medical Center, John Muir Health, in Concord, Calif., and chair of its cross-campus critical care committee, said the increased visibility of CFOs over the past decade has given her teams greater context to advocate for technologies. Education, transparency and openness about priorities — from both the clinical department and the CFO sides — have facilitated discussions on technology prioritization.

“I would encourage a CFO to remain visible, to be approachable, to make sure their communication is clear, to be open to the ideas that are brought forward from the staff, because some of their cost-containment ideas are fabulous,” Olff said.
3 Promote collegiality by engaging department leaders
Leaders agree it takes collegiality and a willingness to be open to the needs of others to triage technology budgeting decisions.
“Our priorities are not always first in line,” Oschner’s Wells said.
She and her peers advocate involving department leaders in a collaborative budget prioritization process, where each rationale and analysis is evaluated in the context of the entire organization’s needs.
“Some of this ends up being more qualitative than quantitative, and sometimes it’s the wisdom of the crowd,” said John Halamka, MD, MS, president, Mayo Clinic Platform and cofounder of the Coalition for Health AI.
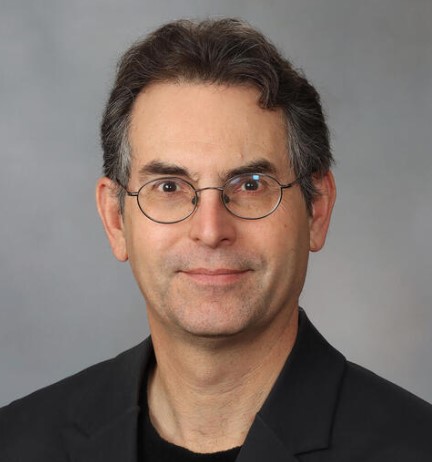
“I have been in organizations where sometimes each department or division looks at its budget in the abstract and says, ‘If my budget’s bigger and yours is smaller, that’s good,’ said Halamka.
Mayo’s collegiality, he said, allows administration and clinicians to come together and ask, “What’s actually for the greater good of the organization?”
UW Health’s Flannery described how a collegial approach with operations leaders can get them on board with a decision for the good of the organization. He said it helps them reach a point where they will say, “You know what, I really want this technology, but after hearing this particular case, I understand that that’s a higher and better use of the limited dollars that we have.
“That doesn’t mean that everybody leaves the table in complete agreement, but it does build toward a general consensus that’s then shared across additional clinical leaders.”
Bringing leaders together to discuss technology investment also can unearth opportunities for improvements.
Departmental energy toward a new investment in technology can be an opportunity for CFOs to ask for reciprocal concessions, Atlantic General’s Kanuch noted.
Should a surgical department be reticent to limit medical device vendors, for example, a request for a technology investment could become an opportunity to reopen discussions about reducing costs in purchasing contracts to find budget for the request, Kanuch suggested.
Make sure promised change actually happens
The process of adopting a new technology does not stop with the decision of which technology to pursue. Internal champions for the technology might also need encouragement to stay energized throughout the process.
Kanuch said that while he encourages creativity and wants department leaders to come with ideas and options, he also looks for advocates who believe in a technology’s promise strongly enough that they’re willing to consider steps like putting some of their own budget at risk — reducing FTE count, for instance — or increasing their caseload estimate to anticipate the return the technology promises.
“If you said you were going to do X, let’s make sure we’ve done that,” Kanuch said. “And if we didn’t do that, how do we adjust? Does that mean we pull back? Do we have to make a further investment? Did we make a wrong assumption? Let’s understand that.”
Mayo Clinic’s Halamka concurs.
“I haven’t seen many organizations do this, but wouldn’t it be wonderful if, four or five years after a project with a demonstrated or claimed ROI made it through the cycle, you would look back and ask, ‘Where were we right and where were we wrong?’ and then hold people accountable. I haven’t seen that so much.”
The path only goes forward
Technology implementation are rarely going to be a line item or a bucket on its own, and financial leaders are learning what it takes to strike a delicate balance in an era of fast-moving pilots, experimentation and ongoing slim revenue margins.
“In revenue cycle, our initiatives are not always at the front of the line. So we must be selective and prioritize what we want to really focus on while there are a lot of great ideas that are always being proposed,” Wells said. “However, we are very excited that it feels like technology is finally going to be working for us and the opportunity to move the needle on quality, efficiency and access is larger than ever.”
Footnote
a. Feinberg, A., Berger, E., and Hammond, R., 2023 healthcare provider IT report: Doubling down on innovation, Bain & Company and KLAS, Sept. 12, 2023 (www.bain.com).
The cybersecurity imperative
No conversation about technology investments is complete without a discussion of cybersecurity investments. Direct written premiums for cyberinsurance are expected to rise to $23 billion worldwide by 2025, from $13 billion in 2022, according to Swiss Re Institute.a And that does not include the costs of proactively investing in protective technology.
“It is a zero sum for sure, but cybersecurity is an imperative, so we are trying to be thoughtful about building a roadmap and sequencing that in an achievable way from a budget perspective,” said Stephanie T. Wells, CPA, CPC-A, system vice president, revenue cycle/HIM, Ochsner Health System. “This helps ensure that it doesn’t cannibalize other initiatives.”
Cybersecurity is an “in parallel” conversation for UW Health in Madison, Wis., and one that relies on close connection among its operating, IT and compliance teams. Those groups have the ability to “press pause” when fast-tracking something that could potentially put the organization at risk.
And while planned for, cybersecurity is also an area where mid-year pivots may be required — and space made for them even if a contingency fund doesn’t exist, said Robert Flannery, MBL, CFO for UW Health.
In addition to their regular meetings with each other, Flannery and Cherodeep Goswami, MBA, UW Health’s CIO, meet regularly with the organization’s audit committee, where a need may come up between budget seasons for additional investment to keep up with emerging cyber and other threats.
“We have a contingency element built into our operating and our capital budgets as well,” Flannery said. “If something comes up that needs funding, then let’s sit down and have the conversation and make sure that we’re protecting the organization.”
Flannery added: “Don’t have a cyber event and say, ‘Well, we knew that we should have protected for this, but we never got it in the budget.’ I never ever want to hear those words. We will deal with variances. I will go back to the board and have a conversation that there’s an addition to the capital or operating budget needed because of X, Y or Z. It’s not an excuse to say, ‘It wasn’t in the budget.’”
Footnote
a. Swiss Re, “What you need to know about the cyber insurance market,” Aug. 28, 2023.





