COVID-19 pandemic continues to have adverse impacts on hospital performance improvement efforts, survey says

Supply chain disruptions, labor shortages and rising expense costs signal the need for transformative change.
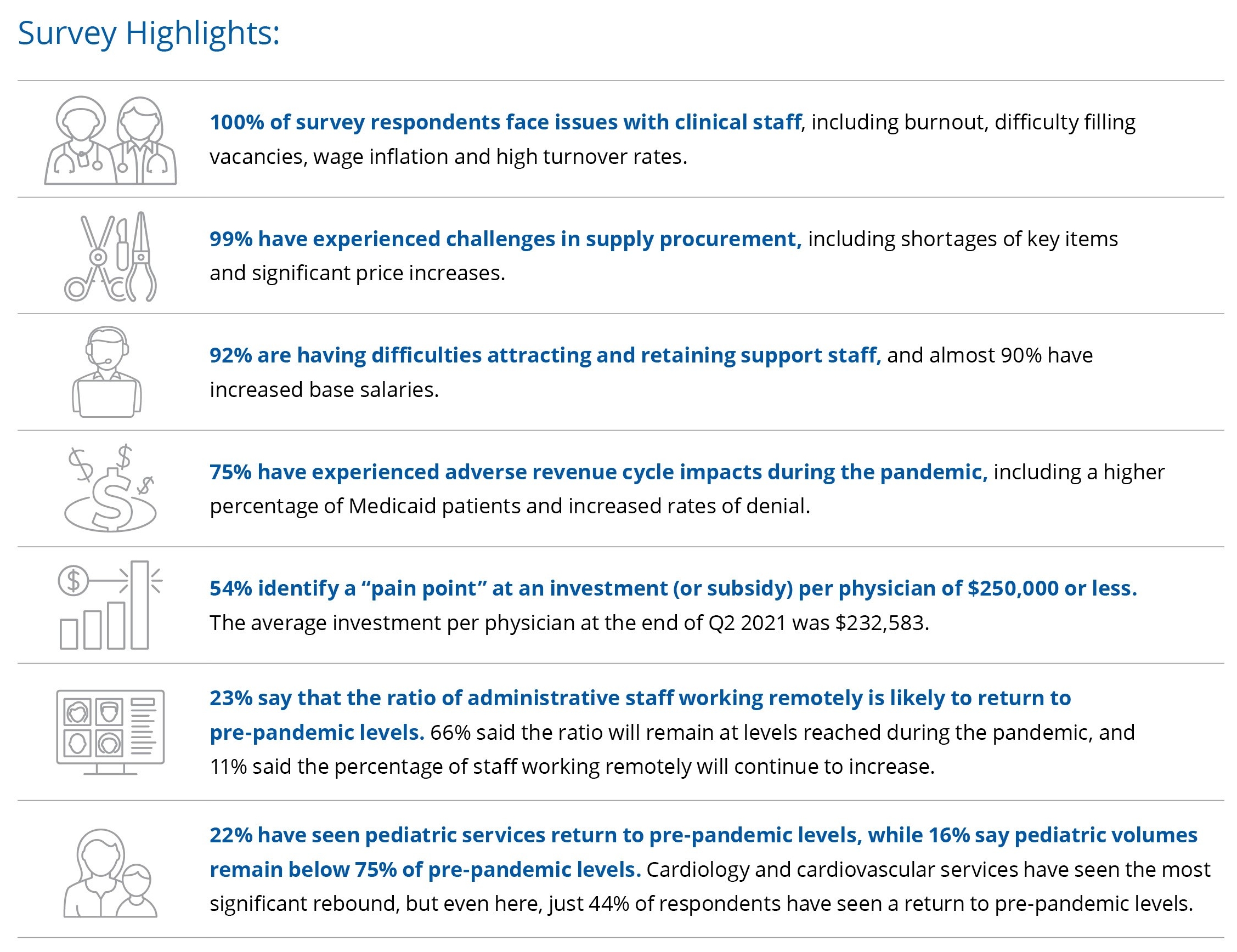
The COVID-19 pandemic continues to undermine performance improvement efforts at hospitals and health systems across the country, according to findings from Kaufman Hall’s 2021 State of Performance Improvement in Healthcare survey.
Supply chain disruptions and shortages have driven up prices and forced a return to the costs of carrying larger inventories of needed supplies. Labor shortages and high employee turnover are pushing up base salaries and recruitment costs and have led many organizations to implement retention bonus programs. Volumes in many service lines remain below pre-pandemic levels, putting downward pressure on revenues. Clinical staff shortages make recovery even more difficult.
Source: Kaufman, Hall & Associates, LLC, 2021
Signs of longer-term change are evident in responses to the survey by hospital and health system leaders nationwide. A strong majority of respondents predict that the pandemic will result in permanent changes to the workforce, with 66% saying that the ratio of administrative staff working remotely will continue at levels reached during the pandemic and another 11% predicting that the percentage of remote workers will continue to increase. Almost half of respondents say the pandemic has driven their organization to adopt new processes, positions or departments that will be continued going forward.
Hospitals and health systems have had little reprieve from the pandemic as new surges in infections have continued to stretch their resources. Yet as a result of the changes that have occurred to date — workforce realignments, a rapid push into telehealth and digital care delivery and shifts in utilizations and volumes — they also must contend with a need for transformative change that touches most facets of operations. Hospital and health system leaders will need to address questions of access to care, supply chain management, patient throughput, workforce deployment, service line development and physical footprint.
Few health systems will have the resources to take on these challenges alone. Many will benefit from forming strategic partnerships — with independent physician groups, payers, retailers, third-party vendors, community organizations and others — that enable them to focus on their core business strategy while expanding the services and optimizing the efficiency, accessibility and affordability of care they provide to their communities. A fundamental question will be what elements of their business they need to control and where they can look to their strategic partners for their support.






