Why cost effectiveness of health should be the prime point of focus for healthcare
Achieving cost effectiveness of health will mean that high-quality care with optimum outcomes will be available to all patients and consumers in the United States at the lowest possible cost. This statement alone underscores why it should be embraced by all healthcare stakeholders as the most fundamental goal for our nation’s healthcare system.
Although this goal has been elusive, the healthcare industry is making headway toward realizing it through many different types of initiatives both large and small in both the public and private sectors. All of our nation’s efforts at healthcare reform over the past 20 years have been focused on cost effectiveness of health at their core. And the simple truth is we, as a society, cannot afford to lose sight of this goal or abandon either hope or determination to make it the hallmark of the U.S healthcare system.
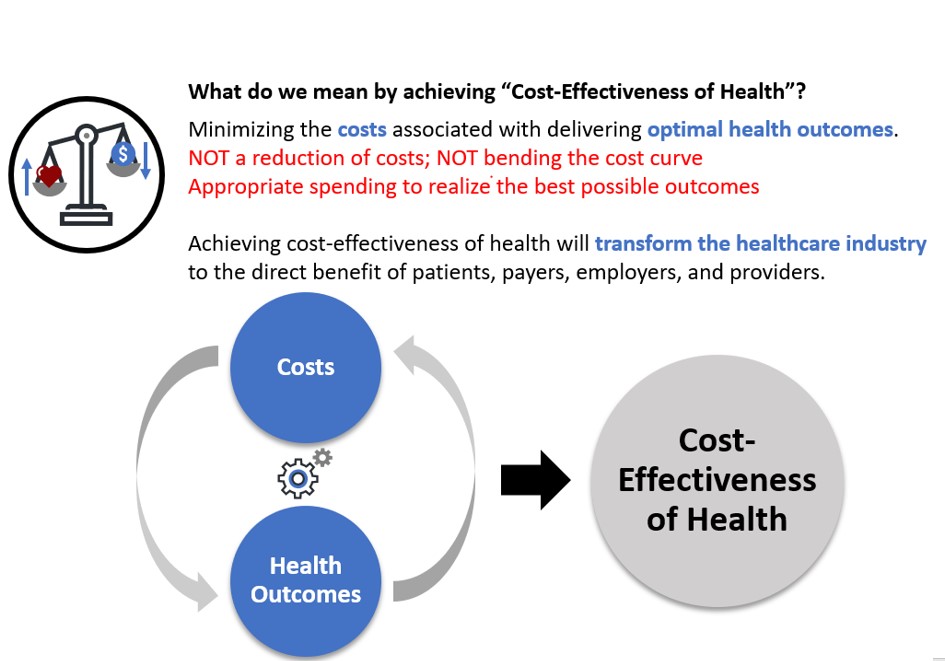
This newsletter aims to inform this effort with thought-provoking discussion, practical insights and real-life examples of applied principles. Throughout this journey, we also will seek to more deeply and richly define this concept and all of its parameters. But to start, we offer the following infographic to provide a foundation for this effort.