Leveraging APPs is key to improving a health system’s provider enterprise

While physicians have historically constituted the vast majority of a health system’s providers, advanced practice providers (APPs) are growing in number and importance throughout healthcare.
The tectonic shift in the number of APPs has been leveraged by many high-performing health systems intent on managing costs while sustaining the quality of care they provide their communities. What if the age-old challenge of effectively operating a physician enterprise has slowly but steadily expanded its focus to operating a provider enterprise that includes more than just physicians?
APPs are commonly defined as non-physician providers — most commonly nurse practitioners (NPs) and physician assistants (PAs) — who often take on medical activities that have historically been performed only by physicians.
According to a Kaufman Hall analysis of 2020 data from professional societies, 63% of providers are physicians, with the remainder comprising APPs, including NPs (22%), PAs (10%) and certified registered nurse anesthetists, or CRNAs (4%). For hospital-based providers, the trend is even more pronounced, with physicians constituting only 51% of providers. Today, there are more than 234,000 NPs, nearly 44,000 CRNAs and almost 133,000 PAs working in the U.S., according to the Bureau of Labor Statistics.
This shift is particularly noticeable in areas such as primary care and hospital services, where many high-performing health systems now engage more APPs than physicians.
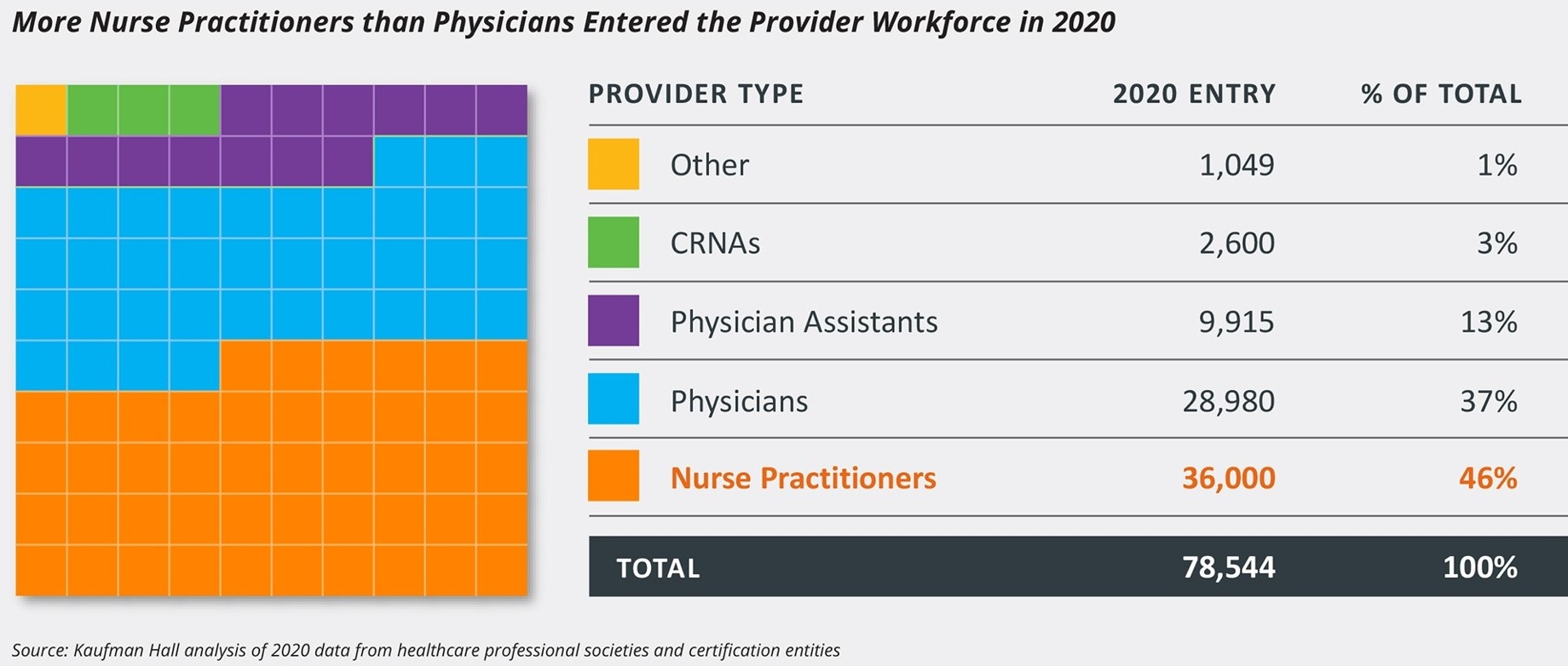
The shift is even more noticeable when taking into consideration clinicians who are just beginning their careers in healthcare. More than 60% of providers entering the workforce in 2020 were NPs (46%), PAs (13%) or CRNAs (3%), while only 37% were physicians, according to a Kaufman Hall analysis of data from professional societies.
Providers entering the workforce in 2022
Organizations that embrace APPs are increasingly outperforming their peers on both productivity and compensation metrics. According to the data used in Kaufman Hall’s Physician Flash Report, high performers are effectively using a higher percentage of APPs in their workforce than those with low APP representation.
One high-performing academic health system in the Southeast now employs four APPs for every physician in its hospitalist and intensivist services. With labor costs that are about a third as much per APP (versus per physician), the system is able to save on labor costs by staffing its intensive care units with APPs, while having physicians oversee clinical delivery from a centralized systemwide e-command center.
In addition, as part of efforts to address clinical shortages, the U.S. government and many states have taken steps to remove practice restrictions on APPs. For instance, the U.S. Department of Veterans Affairs (VA) has granted full practice authority to advanced practice RNs within the scope of their VA employment since 2016, except for applicable State restrictions on the authority to prescribe and administer controlled substances.
In April, Kansas became the 26th state to adopt full practice authority for NPs. The American Association of Nurse Practitioners defines full practice authority as “the authorization of nurse practitioners (NPs) to evaluate patients, diagnose, order and interpret diagnostic tests and initiate and manage treatments — including prescribing medications — under the exclusive licensure authority of the state board of nursing.”
The pace of change in the make-up of providers at a typical health system has been gradual. As a result, many healthcare leaders have not necessarily perceived the significant shift in the clinical workforce. But as early adopters adjust their strategies and separate themselves from the rest of the industry, the time for leveraging the promise of APPs is now. Ultimately, health systems focused on delivering high-quality care while controlling costs in the future must transition from a physician enterprise to a provider enterprise to achieve their long-term goals.






