SDOH initiative reduces readmission penalties in one year
- McLaren Port Huron hospital focuses on patients with some of the most high-cost, high-risk chronic conditions, which account for a significant portion of their readmissions.
- Within 24 hours of admission, McLaren case managers screen patients via a tablet application.
- The hospital expanded screenings beyond COPD and CHF patients to the entire inpatient population.
McLaren Port Huron hospital reduced its Medicare penalty percentage for 30-day readmissions from 2.34% in FY18 to 1.85% as of April 2019. In fact, the hospital’s overall all-payer readmission rate is trending down as well. That is no small task, considering that one of every six discharged patients in the U.S. is readmitted in fewer than 30 days, and a third of those within only seven days of discharge (Binder, L., “Medicare’s Penalties for Readmissions Work, Despite Flaws,” Forbes, 2019).
One major factor in this readmission rate reduction is McLaren’s emphasis on identifying and addressing patient social determinants of health (SDOH). The focus is on educating patients and involving them in their healthcare plan.
Moving beyond penalties
A portion of any hospital’s desire to reduce its readmissions rates is the Medicare Hospital Readmissions Reduction Program (HRRP), which is a Medicare value-based purchasing program that reduces payments to hospitals with excess readmissions. But it’s about more than just avoiding penalties. Reducing readmissions improves patient outcomes and lowers costs in other ways, including fewer trips to the emergency department (ED), fewer acute events and less burden on payers.
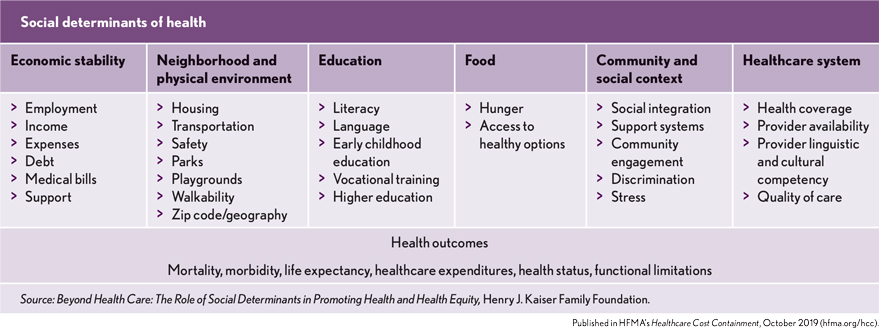
Much of the research concerning how to reduce readmissions keeps coming back to one point — readmissions can be largely attributed to what happens after the patient leaves the healthcare organization. Even with a team of the most dedicated physicians, nurses and other clinicians, we can only do so much to address factors such as healthy eating, medication adherence and the availability of transportation to follow-up appointments after the patient is discharged. And it’s precisely these factors — all impacted by larger SDOH — that influence whether, and how soon, our inpatients become readmission statistics.
See related sidebar: The 4 Cs of social determinants of health
Focusing on high-cost conditions
McLaren focuses on patients with some of the most high-cost, high-risk chronic conditions, including chronic obstructive pulmonary disease (COPD) and congestive heart failure (CHF).
After discharge, 10% to 20% of COPD patients are readmitted within 30 days (Simmering, J.E., Polgreen, L.A., et al., “Identifying Patients with COPD at High Risk of Readmission,” Journal of the COPD Foundation, 2016). Patients who are readmitted following a COPD hospitalization are at greater risk of mortality and have worse outcomes relative to patients who are not.
And the healthcare costs associated with COPD patients are high and growing. National medical costs attributed to COPD were $32.1 billion in 2010 and predicted to reach $49 billion by 2020 (Chronic Obstructive Pulmonary Disease – COPD Costs, CDC). And a study of individual worker productivity and healthcare costs found that patients with COPD incurred costs that were almost twice as high as costs for patients without COPD, after adjusting for comorbidities. Patients with COPD had significantly more than twice the odds of having a hospitalization or ED visit compared with patients in the non-COPD cohort (J.G., Patel, Coutinho, A.D., et al., “COPD affects worker productivity and health care costs,” International Journal of Chronic Obstructive Pulmonary Disease, 2018).
The numbers for CHF patients are no less daunting. CHF is the most common cause of readmission for Medicare patients in the U.S. (Chamberlain, R.S., Sond, J., et al., “Determining 30-day readmission risk for heart failure patients: The Readmission After Heart Failure scale,” International Journal of General Medicine, 2018). The 30-day readmission rates among CHF patients are 9.42% and 9.17%, for derivation and validation cohorts, respectively.
According to the CDC, about 5.7 million adults in the U.S. have heart failure, and the condition costs the nation an estimated $30.7 billion each year. (Heart Failure Fact Sheet, Centers for Disease Control and Prevention)
Heart failure is an important contributor to both the burden and cost of national healthcare expenditures, with more older Americans hospitalized for heart failure than for any other medical condition. (Heidenreich, P.A., Albert, N.M., et al., “Forecasting the Impact of Heart Failure in the United States,” Circulation: Heart Failure, 2013). By 2030, more than 8 million people in the U.S. (1 in every 33), will have heart failure. Between 2012 and 2030, real total direct medical costs of heart failure are projected to increase from $21 billion to $53 billion. Total costs, including indirect costs for heart failure, are estimated to increase from $31 billion in 2012
to $70 billion in 2030.
Faced with these statistics, it was clear that reducing readmissions for these populations was essential for McLaren.
Combining technology and care coordination
My search led me to a patient engagement technology company that helps us identify SDOH factors and coordinates with local community resources in our area to help our patients get the services they need. The results include the following:
- Better health outcomes for patients
- Reduced readmissions for McLaren
- Lower costs across the board
Within 24 hours of admission, our case managers screen patients via a tablet application. The screening asks about food scarcity, transportation, social/family support networks and exercise habits, among other areas. The COPD and CHF screenings include disease-specific education, questions and information in addition to the standard SDOH inquiries. Patients who agree to the screening receive regular text messages with health information, including medication reminders and wellness tips for up to 30 days after discharge.
Based on patients’ individual screening responses, the technology identifies patients who are at high risk for potential readmission as a result of their personal SDOH factors and sends an alert to case managers. As a second step, the technology company reaches out to the appropriate local resources in our community to help ensure the identified SDOH needs are addressed. The company communicates directly with the patient and community resources to coordinate service delivery. If a connection can’t be made, they alert us again to let us know that the patient may now be at even greater risk for readmission.
Based on initial positive results, we’ve recently expanded the use of the screenings from our COPD and CHF patients to our entire inpatient population — our case managers have offered the screening to more than 600 patients in the past year.
Identifying at-risk patients
McLaren’s success can be attributed to identifying patients at risk of readmission and offering education, care coordination and follow up. By reducing readmissions, the hospital is reducing Medicare penalties and providing patients with improved care experiences and outcomes.





