How Orlando Health improved its bottom line by optimizing observation services





Bringing together clinician “huddles” for quick reviews of the status of patients under observation was just one step that enabled the Florida health system to substantially reduce length of stay among observation patients, thereby reducing costs and increasing revenues by tens of millions of dollars.
Effective management of patients in observation status is important for ensuring a health system’s profitability. By optimizing length of stay (LOS) among patients in observation, a health system can free up capacity for care of patients with higher-acuity conditions. These benefits will remain elusive, however, if the organization lacks a clear strategy and approach for addressing observation management inefficiencies.
Orlando Health in central Florida offers a case example of how one health system has successfully pursued such an effort. As a private, not-for-profit healthcare system comprising eight community and specialty hospitals with over 1,800 beds, Orlando Health was struggling with rising observation rates and associated capacity constraints. The executive team was challenged to reduce observation rates by optimizing the process for determining patient status and shortening LOS for these patients.
To achieve these goals, they designed and launched a multifaceted initiative aimed at improving management of their observation patient population at each of its hospitals.
7 ways to ensure optimal observation rates are established and observed
Broadly, the initiative encompassed the following seven areas of focus deemed essential to the health system’s efforts to establish and maintain optimal observation rates.
1. Create dedicated observation units
A lack of bed availability to move patients from the emergency department (ED) created throughput issues for observation patients, with the result that they ended up scattered throughout the hospital. By developing dedicated observation units, a hospital could create cohorts of observation patients while opening up inpatient beds for higher-acuity patients.
The specifics of each observation unit vary by hospital, depending on the space available. Dedicated units range from 15 to 25 beds. Some facilities use clinical decision units that interacted closely with ED staff to help patient placement or the decision to discharge.
Initially, only patients who met selective criteria were placed in observation units. Such criteria applied, in particular, to patients experiencing cardiac-related symptoms. This approach allowed hospitals to pilot the functioning of the observation units and address common barriers before expanding to the entire observation patient population.
With dedicated units, the system achieved synergies in treating patients. The units helped create a culture where it was understood that observation patients had relatively low acuity and should have a short LOS. As such, the care teams were better able to prioritize observation patients for ancillary testing, thereby contributing to a decrease in the LOS. Hospitals were also able to vacate beds on higher level of care units, including intensive care units.
2. Implement observation huddles
Observation patients who were not placed in the dedicated observation units also required attention. Taking a lesson from its success in managing inpatients through multidisciplinary rounds, the organization implemented daily observation huddles in an effort to achieve similar results with the lower-acuity population.
The huddles are 15-minute calls in which the care management leader, the utilization review team and physician advisors discuss each observation patient. The huddles have two goals:
- Assign and communicate follow-up tasks.
- Convert or discharge observation patients.
Participation of physician advisors in the huddles was key to their success. (The role of physician advisors is discussed in greater detail at step six below.) A physician advisor can directly indicate whether to convert a patient or schedule follow-ups with physicians who might have disagreed with the outcome of the secondary level review.
To be effective, huddles also require a strong facilitator, who can bring clarity around assignment of follow-ups and reiterate the plan of care for the patient.
Orlando Health saw the observation rate decline immediately after it implemented the huddles, with a 15% decline in the number of observation patients staying greater than 48 hours, and a 25% decline in Medicare patients with long LOS.
3. Educate staff on effective observation patient management
To sustain results achieved, Orlando Health needed to ensure all members of the care team were knowledgeable of observation patient management. The health system developed and delivered specific education to the care management team and bedside nursing, in particular, because these departments were identified as critical to the success of the process changes.
Bedside nurses typically have the most frequent interaction with patients and often are most attuned to when patients are ready for discharge. These staff members were presented with an overview of:
- The meaning of observation status
- Documentation requirements for billing
- Circumstances when inpatient status may be appropriate
- The role of care management
- The need for collaboration to improve patient satisfaction, achieve the correct admission status, and reduce LOS
In addition to these topics, education for the care management team focused on:
- Application of the Two-Midnight Rule
- Observation billing rules
- When observation is appropriate after a procedure
- Status implications for the patient
4. Redesign the care management function
A review of the organization’s care management department disclosed an opportunity to combine the role of care managers and utilization review nurses and establish care management teams to manage caseloads of similar units. Shifting to an integrated dyad model improved collaboration across the continuum of care while serving patient needs in a quality and timely manner.
Orlando Health: Integrated dyad model for care management
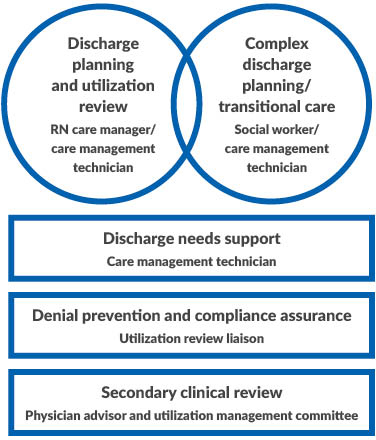
Source: Claro Healthcare, 2020
Orlando Health implemented the integrated dyad model, which combines the roles of care managers and utilization review, to improve collaboration across the continuum of care.
This redesign reduced silos and redundancy of efforts while improving patient flow by centralizing teams responsible for cohorts of patient populations. Care management teams consisting of registered nurses (RNs), social workers and technicians now cover similar units. Staffing for each team is determined based on projected daily census by unit.
A new role, the utilization review liaison, was created to manage denial prevention and ensure timely compliance. Freed of these responsibilities, RN care managers can focus on utilization review and simple discharge planning. Social workers focus on complex discharge planning and coordination of care. The team leverages technicians to support clerical and post-acute care coordination efforts.
Education and hands-on cross-training also were required to clarify new roles and responsibilities.
5. Optimize the ED care manager role
Orlando Health already had care managers located in the ED, but it wanted to improve collaboration between physicians and care managers in the admissions process. To accomplish this objective, the health system identified workspaces within the ED where care management would be visible and could interact with physicians as status decisions were being made. Care management coverage in the ED was altered to focus on times with historically high volumes, resulting in increased coverage hours of up to 24 hours a day at the largest facility. This change helped bring about the desired collaboration and improved documentation of medical necessity for admissions.
6. Revamp the physician advisor program
Physician advisors are instrumental in promoting a health system’s financial health. The stringent financial constraints under which health systems must operate in today’s complex regulatory and compliance landscape can leave physicians confused, with patients often caught in the middle. Physician advisors bridge the gap between physician partners and the care management team while supporting the revenue cycle.
To fulfill this role, Orlando Health hired dedicated physician advisors to support these demands. The health system’s initial goal was to have one physician advisor per site, to be available to provide care management for all secondary reviews during business hours. An additional physician advisor was made available on call for the entire system after 5 p.m. to support portal-of-entry care managers. For weekends, the health system instituted a rotating call schedule where one physician advisor would provide coverage remotely systemwide.
Because the physician advisors possess not only leadership skills, but also people skills, they have been well received by medical staff, nursing staff, executives and revenue colleagues. Essential characteristics included:
- Ability to educate colleagues in a non-confrontational fashion.
- Strong communication skills to explain complex medical issues to physicians, medical directors of health plans, nursing and executives.
- Strong written skills to appeal denials with payers.
- ·Strong clinical skills, preferably boarded in their specialty, with the ability to formulate strong rebuttals to support medical necessity for hospital care.
7. Institute metrics and reporting to monitor LOS and observation rates
Orlando Health recognized the need for metrics and reporting to advance and sustain the initiative. The key purposes for reporting are to:
- Aid in completion of daily duties.
- Provide visibility into performance metrics.
Targeted reporting for observation huddles and utilization reviews at the point of entry has been particularly beneficial for these areas. An observation scorecard dedicated to care management also was developed to enable the team to monitor performance of the new processes.
Observation huddles. Although the observation units helped create cohorts of patients in a single space, observation patients could still be found on other units within the hospital at times of high census. Therefore, participants in the observation huddles needed a synchronized worklist to be successful. The health system therefore needed to create an observation census report, listing observation patients within the hospital and additional detail such as current LOS, initial diagnosis and payer source to aid discussion during huddles. The report is automatically created every morning to support care managers’ efforts to prioritize assigned observation patients at the start of the workday.
Portal-of-entry reviews. The portal-of-entry team reviews cases in the ED for timely and appropriate status determination at the beginning of the patient stay. An indicator of the team’s performance is the rate of admissions for observation. To reduce this metric, a system-generated report is sent to portal-of-entry in the morning and afternoon. The information identifies which patients require an admission review, providing the team with a process to perform a concurrent review process that can have a real-time impact on the status determination process, instead of having to work a backlog of retroactive reviews.
The report alone does not ensure patients receive timely reviews. Incorporating it into the daily workflow, however, has resulted in an increase in patients whose utilization reviews are completed in a timely manner. The observation rate at admission decreased by nearly 10% over the course of four months.
Scorecards. Each facility also has a scorecard for its own metrics for the current month’s performance and trends over time. The most prominent indicators of performance in the scorecards are observation rates and observation LOS, viewed from both a hospital-wide and payer class perspective. Additional metrics included inpatient LOS and patient satisfaction scores.
Results
By improving its process for determining patient status and reducing LOS, Orlando Health has achieved a total benefit exceeding $40 million. The initial 12-month period yielded additional revenue of $13 million from status determination improvements and $4 million from LOS improvements. At this level of performance, Orlando Health expects to continue achieving $27 million in annual benefit relative to the baseline period.
Looking at observation rates, the observation-to-inpatient ratio has decreased by 7% for all payer classes. Medicare observation rates decreased by over 10% at most facilities. Observation LOS decreased by nearly 10 hours across the system. Reduced LOS created additional bed capacity, enabling Orlando Health to backfill the newly available beds with additional patients and realize an increase in incremental revenue.
Orlando Health: Trend in observation-to-inpatient ratio for traditional Medicare
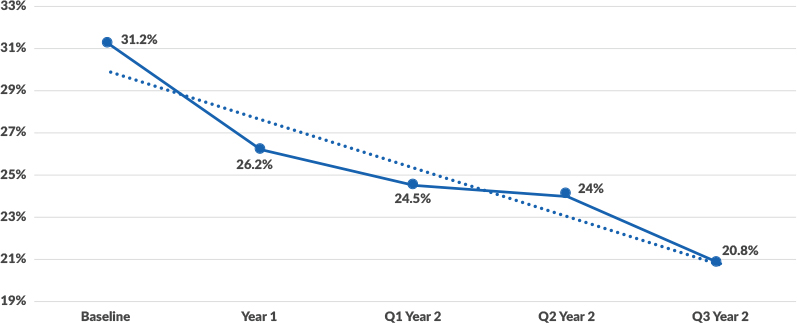
Source: Claro Healthcare, 2020
Orlando Health: Trend in observation length of stay in hours
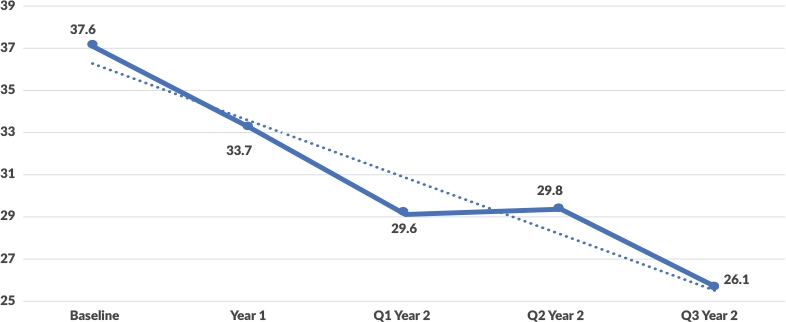
Source: Claro Healthcare, 2020
4 lessons learned from Orlando Health’s observation improvement initiative
Any time organizations undertake initiatives impacting the existing culture, there are lessons that can be applied for future change management ventures. Four takeaways from Orlando Health’s experience in seeking to optimize observation services are applicable to almost any hospital change management endeavor:
- Communication is key. Change in hospitals touch many stakeholders and coordination needs to begin with communicating why the change is needed.
- Strong leadership and messaging to staff will have a profound impact. In times of change, staff will look to their direct leader for guidance and observe their actions. Management’s reaction to changes is the first impression team members see and the basis for attitudes that develop.
- Data tells your story. Sharing data is to your advantage when trying to attain buy-in or show progress.
- Physician leadership via a physician advisor program can bridge the gap between clinical and financial departments. A physician advisor can be an invaluable resource through established relationships with both the care team and the business office.
The importance of improved observation after COVID-19
Healthcare systems are under pressure from numerous external forces including COVID-19 and increased regulatory burdens, creating substantial financial challenges for leaders across the United States. A recent Fitch Ratings report finds that the median hospital operating margin had improved year over year, largely attributed to clinical and operational improvements from prior years.a Now, in the face of a sudden economic crisis, the need for effective operations management to organize, plan and execute strategies to ensure the stability of healthcare systems has never been higher.
Sustainable financial transformations in healthcare organizations, particularly in the face of a crisis such as the COVID-19 pandemic, require both revenue enhancement and cost management. In clinical operations, revenue enhancements can be realized by managing medical necessity and increasing hospital capacity through length of stay improvements. Effective cost management strategies in clinical operations are often achieved by applying evidence-based protocols to reduce variation, reducing excessive testing, and streamlining patient discharge processes. For organizations struggling with capacity management or looking to improve their financial standing through clinical operations, focusing on improving care in a lower acuity population such as observation patients can prove to have an immediate impact for the financial health of the organization. Lessons learned from standardizing care for a lower acuity population, such as observation patients, can then be applied to expanded patient populations.
Footnote
a Holloran, K., “Smaller U.S. NFP Hospitals Lead Turnaround in Margins,” Fitch Ratings, Sept. 3, 2019.





