Physician practice performance suffered during the 2020 pandemic year

Cynthia Arnold

Matthew Bates
Volatility driven by COVID-19 rocked physician practices throughout 2020, although some signs of recovery emerged later in the year.
Physician practices performance declined across key performance metrics in 2020 compared with pre-pandemic levels, according to a new report from Kaufman Hall.a
Physician productivity, compensation and revenues for the year all fell below 2019 results, while the average investment required to supplement physician revenues rose.
Even so, physician practices saw some signs of recovery in the second half of 2020, following significant disruption in the early months of the pandemic as nationwide shutdowns and concerns over potential COVID-19 exposure drove declines in physician visits. The median investment (or subsidy) per physician FTE fell 26% from a high of $289,268 in the second quarter to $213,118 in the fourth quarter, indicating the beginning of a return to pre-pandemic performance. The median investment/subsidy per physician FTE for all of 2020 rose 6.8% from 2019 to $239,656, largely due to lower patient volumes earlier in the year.
Physician compensation remained relatively steady, while productivity declined
Physician compensation per FTE declined just 1.6% from 2019 to $303,181 in 2020, as many health systems chose to freeze compensation levels during the pandemic, thereby preventing a greater decrease overall. Median physician compensation per FTE was $306,148 for the fourth quarter of 2020, up 1.4% from the third quarter and closer to the 2019 median of $307,961. Declines in productivity, however, led to a 6.3% year-over-year increase in physician compensation per work relative value unit (wRVU) from 2019 to 2020. From Q3 to Q4, physician compensation per wRVU was up 5.6%, but remained below Q1 and Q2 levels.
Overall physician productivity decreased for the year, with physician wRVUs per FTE falling 8.4% from 2019 to 2020, due to the impacts of the pandemic. This measure improved significantly in the second half of the year after a Q2 plunge, but it remained below prior-year performance for each quarter of 2020.
The effects of the pandemic on physician productivity varied across specialties. Primary care physicians saw the most robust recovery due to a patient-centric approach, including an increase in telemedicine offerings. They face stiff competition, however, from an ever-growing array of companies offering virtual care services. Specialty referrals remained down as patients delayed seeking care for new issues. Recent media reports indicate that initial diagnoses of diseases like cancer dropped in 2020 but could increase drastically as patients return in 2021.b
Pandemic-related volume declines drove down revenue, expenses
Net revenue per physician wRVU rose just 1.4% from 2019 to 2020 due to interim payment plans that increased compensation for COVID-19 cases. Looking back over the course of the year, this measure dropped in early 2020, but increased incrementally each quarter after, including a 0.5% increase from Q3 to Q4.
Net revenue per physician FTE, however, fell 6.3% from 2019 to a median of $566,773 in 2020 due to pandemic-fueled declines in patient volumes. Looking at results by quarter, the measure declined slightly at 0.8% from Q3 to $598,805 in Q4, but it remained closer to 2019 levels after hitting a low of $447,383 in Q2.
Total direct expense per physician FTE, including advanced practice providers (APPs), fell 4.9% — more than $40,200 — from 2019 to $782,518 in 2020. Contributing factors included volume declines associated with the pandemic that led to lower overall expenses, and reductions in staff availability as many clinicians — particularly female physicians and APPs — had to stay home to care for children and others due to school closures and nationwide shutdowns. Total direct expense per physician FTE rose 0.9% from Q3 to Q4. If expenses continue to increase in 2021, organizations may need to increase investments per physician, further straining physician enterprises and the health systems that employ them.
Support staff FTEs per 10,000 wRVUs was up 6.1% from 2019 to 2020. This result likely is due to decreased physician productivity and the fact that many health systems maintained support staff positions despite decreased patient demand.
Patient demand, accountability are key physician strategy factors
Many hospitals and health systems continue to develop and grow their employed physician strategies as older physicians retire and recruitment for new physicians becomes increasingly competitive. Healthcare leaders should take a balanced approach to meeting patient demand moving forward. Rethinking the investment required to pay physicians (after the partial offset by revenue generated through the physician practice) is a critical step in paving the way to robust value-based care.
At the same time, health systems need to set clear clinical quality and economic targets. Establishing a physician management system with accountability for both physicians and administrators is essential to ensuring optimal physician practice performance.
2020 takeaways
- Financial pressures remain high, and systems and their boards will be scrutinizing investments/subsidies per physician FTE.
- Health systems will need to actively understand 2021 physician enterprise investments/subsidies at the clinical cohort level compared to actual benchmarks to set realistic performance targets.
- Management of these factors will require developing individualized business plans to achieve well-defined, shared goals.
- Physicians will need to be actively engaged and participate in managing access for new patients. Their incentives must balance production incentives with initiatives that support holistic patient care within the larger health system’s patient population.
- Organizations should engage physicians (especially specialists) in these activities because physicians are aware of the issues and likely have unique insights on these trends.
The Physician Flash Report is available online, free of charge.
Key performance metrics summary
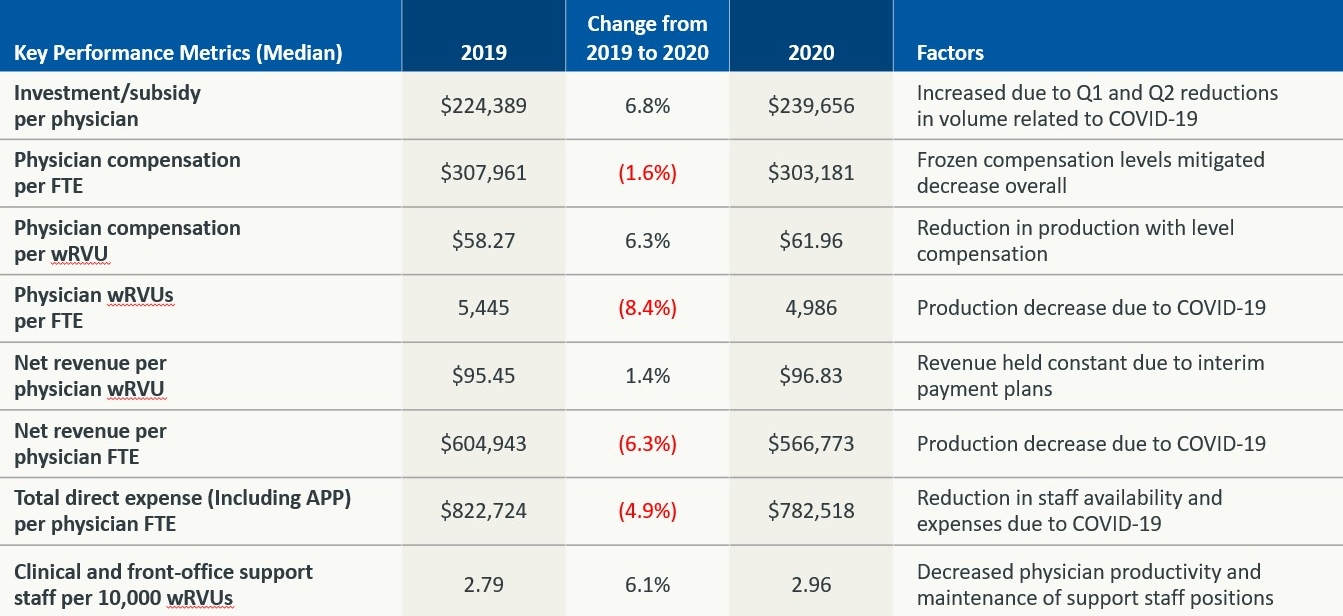
Source: Kaufman, Hall & Associates, LLC, Physician Flash Report, April 2021.
Footnotes
a Kaufman Hall’s Physician Flash Report uses actual data from the most recent three years sampled on a recurring monthly basis from Axiom Comparative Analytics from Syntellis Performance Solutions, which incorporates data analytics on more than 68,000 physicians, 28,000 advanced practice providers, and 100 specialties. The sample of physicians represents data from across the United States. Physicians of all types are represented, from family medicine physicians to neurosurgeons, and from single physician practices to large academic physician groups. Advanced statistical techniques are used to standardize data, identify and handle outliers, and ensure statistical soundness prior to inclusion in the report.
b Kluger, J., “You May be surprised by the type of American who is postponing basic health care during the pandemic,” TIME Magazine, Feb. 23, 2021.






