Healthcare leaders view care coordination as an increasingly vital investment, survey finds
An HFMA survey of healthcare finance leaders found varying approaches to care coordination payment mechanisms, infrastructures and strategies for generating an ROI.
- A large majority of healthcare finance leaders expect to increase their investments in care coordination over the next two years, an HFMA survey found.
- Some respondents said they receive funding from health plan partners or Medicare, but payment mechanisms for care coordination remain works in progress.
- Survey respondents see the biggest ROI from care coordination in managing high-risk patients and in activities such as guiding care transitions.
As population health management becomes more of a focal point in healthcare, providers are ramping up their care coordination programs to ensure patients don’t fall through the cracks.
That trend was apparent in a recent HFMA survey, with 70% of respondents saying their care coordination budget will climb during the next two years.
“With increasing efforts to reduce the total cost of care for patient populations, care coordination has become an effective strategy for health systems to more efficiently deliver care,” said Katie Gilfillan, HFMA’s director of healthcare finance policy, physician and clinical practice. “Better care coordination ensures patients have access to care in the appropriate settings and optimizes their care paths.”
Where the increased spending is likely to go
Staffing will be the primary area of investment for care coordination budgets, according to the survey, which was conducted in Spring 2019 and included responses from 81 healthcare finance executives. Almost half of respondents’ care coordination budgets is allocated to staffing, with the remainder evenly split among technology, analytics, social support resources and behavioral health integration.
“We make a significant investment each year in salary and benefits,” said Donna Littlepage, senior vice president for accountable care strategies with Carilion Clinic in Roanoke, Virginia. “It’s an investment we feel we need to make to take better care of our patients.”
“All too often, people buy a solution and say, ‘Hey, this is a new solution, and it will do X, Y and Z,’” said John Zabrowski, senior vice president and CFO with Virginia Hospital Center in Arlington, Virginia. “But if somebody isn’t doing the blocking and tackling and making sure the workflow is as effective as it can be, the benefit of technology can’t be leveraged as much.”
Technology moves to the forefront when an organization is ready to scale a care coordination program, Zabrowski added.
Risk stratification tools and processes constitute the most important investment in care coordination, said Bruce Henley, vice president and CFO with St. Elizabeth Physicians, the multispecialty physician organization of St. Elizabeth Healthcare in the Greater Cincinnati area.
“Technology is a must, but it’s also the people,” Henley said. “The technology is great at identifying the high-risk patients, but then you have to be able to operationalize that information. Communicating and coordinating with your providers in your practices is crucial because the technology won’t catch every high-risk patient.
“Once you identify that high-risk or rising-risk population, the people whom you have to monitor, then you can start to develop the personnel and processes that you need to develop a successful care management program.”
Finding ways to pay for care coordination
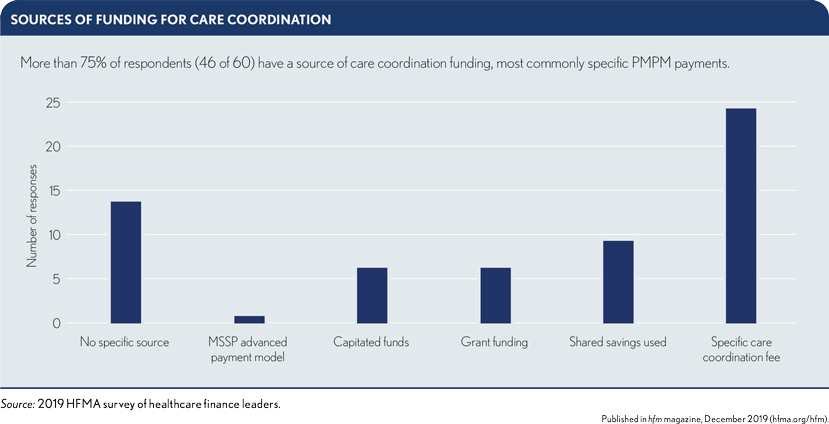
Funding mechanisms for care coordination vary, with 24 of 60 respondents (40%) to one question saying they build a per member per month fee or other specific care coordination fee into their payment model. Others use shared shavings, while 14 of 60 (23%) said they don’t have a specific funding source.
Carilion Clinic began its care coordination program when it launched a patient-centered medical home around 2008, Littlepage said. At first, internal investments were the sole funding source.
“Once we put it in place, we then made it part of our payer negotiations to tell them that we were doing this, we were doing it for their members, and they should help us fund this,” Littlepage said. “The majority of them did. We get a per member per month fee from many of our payers — Medicare Advantage, managed Medicaid and commercial — to help support our care coordination activities.”
Carilion Clinic also invests a portion of the incentive payments it gets from quality-measurement programs, including in Medicare Advantage, as well as shared savings.
Henley estimates that 80% of funding for the care coordination program at St. Elizabeth Physicians comes from Medicare’s Comprehensive Primary Care (CPC) Plus program and commercial payers. “There are other components that are necessary for a robust program that we internally fund as part of the mission of the organization,” he said.
Establishing an infrastructure
A plurality of survey respondents (42%) reported locating care coordinators both centrally and in individual departments or practices, but only a third said they allocate the cost of care coordinators back to the practice or department level.
After assessing the efficacy of its care coordination program in the early stages, Carilion Clinic moved its coordinators out of the clinic setting.
“I can see the arguments on both sides of that,” Littlepage said. “You build relationships with the providers by being in the practice. But we also know those very same relationships are why, when someone asks you to do something that’s not part of your daily duties as a care coordinator, it’s awfully hard to say, ‘No, I can’t do that.’”
St. Elizabeth Healthcare installed a comprehensive care coordination system after launching the program with funding from Medicare’s earlier CPC initiative and commercial payers.
Even though only about half the practices were in the original CPC program, St. Elizabeth leadership decided to expand the care coordination effort throughout the organization to best serve its entire patient population.
“Our healthcare advocates in our offices work with patients and work with our central team to identify those patients who need to be monitored weekly, monthly or maybe once every three months or so,” Henley said.
Among the services provided by the organization’s central ambulatory care management team:
- Care coordinators identify care gaps that need to be closed and work directly with patients to help them navigate the system.
- Pharmacists and pharmacy technicians perform medication adherence on-site with physicians and patients.
- Social workers help patients in areas such as obtaining needed medications or transportation to appointments.
The ROI for care coordination
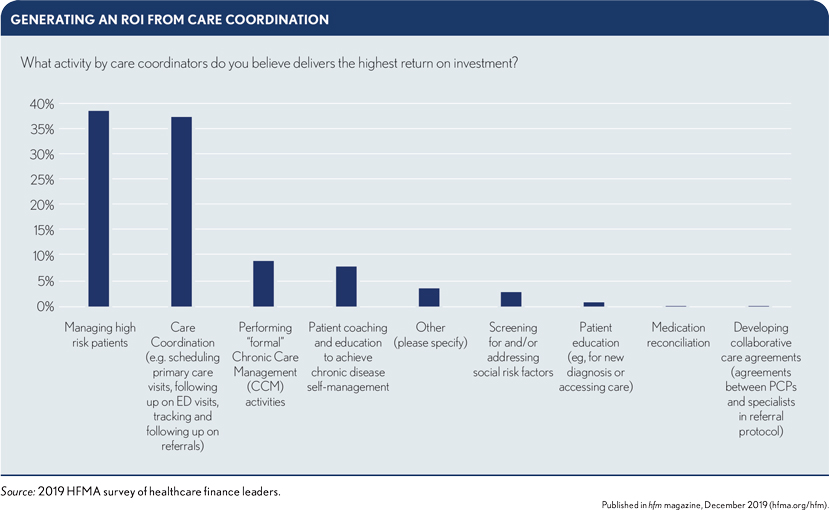
A slight plurality of survey respondents (38%) cited ”managing high-risk patients” as the activity through which care coordinators can generate the highest ROI.
Carilion Clinic focuses not on patients who already require a high level of healthcare services but rather on those who are about to fall into that category.
“Those are the people you can impact and prevent from getting there,” Littlepage said.
To optimize care coordination for high-risk patients, providers can incorporate care-quality dashboards and scorecards, survey respondents said in group discussions. Such tools allow coordinators to zero in on care gaps.
Other steps that can enhance the ROI of care coordination for high-risk patients, respondents said, include:
- Integrating care coordination into physicians’ workflows as an optional referral
- Providing risk-stratifying information to identify patients at risk for readmissions or ED visits
General care coordination, such as managing care transitions, also was cited by many survey respondents (37%) as the activity that produces the highest ROI. Specific strategies may focus on:
- Scheduling of wellness visits
- Scheduling of screenings, follow-up visits and referral visits, with regular outreach
The scope of practice for coordinators
Physicians and other clinicians should be educated on the services that care coordinators can provide, survey respondents said in group discussions. Such information can help ensure both that care coordinators are not working beyond the scope of their training and that their time and skill sets are being maximized.
The skill sets of care coordinators, respondents said, may involve:
- Clinical activities, such as post-discharge follow-up calls, diabetes counseling and dietary counseling
- Nonclinical activities, such as helping with patients’ transportation needs
“We haven’t had a lot of focus yet on community health workers,” Littlepage said, noting that Carilion Clinic employs five such workers in conjunction with a local United Way agency and federally qualified health center.
“That’s an area where I think there’s still a lot of opportunity — in the social determinants, trying to assist patients more. We’re beginning to record that data more fully and will determine how best to react to it.”





