Optimal use of APPs can enhance a health system’s post-COVID-19 financial recovery
The experience of a Western Pennsylvania health system shows that a focused effort to optimize the use of advanced practice providers (APPs) can yield millions in increased revenue and operating margin opportunities — which can contribute significantly to a successful recovery from the COVID-19 crisis.
As hospitals and health systems plan for post-COVID-19 recovery, their focus will be on optimizing care delivery and lowering expenses while increasing revenues to help ensure financial sustainability. Enhancing the use of existing resources will be a critical part of organizations’ plans for the recovery.
Rather than simply returning to “business as usual,” organizations will need to make financial and operational improvements to adapt to the changed environment after COVID-19, including taking steps to optimize the clinical workforce and care delivery models. And as part of this effort, leaders should make it a priority to reassess the role of APPs, given these practitioners’ extensive training, broad skill sets and ability to adapt to different practice settings.a
Before the pandemic hit, many hospitals and health systems were beginning to prioritize the optimization and engagement of their APPs to enhance access and improve the cost of care. As one of the fastest growing segments of the healthcare workforce, APPs constitute, on average, more than one-third of a U.S. healthcare provider organization’s clinical workforce.b Moreover, in response to COVID-19, more than three-quarters (78.6%) of organizations are redeploying or plan to redeploy APPs to front-line specialties as a result of clinical staffing shortages in critical departments.c This trend is a clear indicator of the important role this workforce can play in helping their organizations achieve care delivery goals in times of crisis.
Despite the significant growth in APP workforce, however, healthcare organizations all too often have not seen reciprocal gains in revenue and access. Without corresponding increases in patient volume or revenue, operating margins cannot sustain any unsupported cost.
The disconnect between APP staffing and performance has several primary causes, including:
- Inefficient care delivery
- Underutilization of the APPs
- Redundancy in tasks between physicians and APPs
- Misalignment of physician and APP compensation plans
Nonetheless, when leveraged effectively, APPs can provide a significant return on investment (ROI) in the form of additional operating margins from existing resources without the added expense. For hospitals, achieving such an ROI from their APP workforces is important at any time, but it is now critical for them as they begin their recovery from the COVID-19 crisis. The road to successfully optimizing an organization’s APP workforce begins with developing and implementing an intentional strategic plan and framework, whose elements are outlined in the sidebar below (“4 elements of an APP workforce strategy”).
Case Example: Excela Health
The effective pursuit of an APP workforce strategy is exemplified by Excela Health, a three-hospital system in Greensburg, Pennsylvania, with more than 550 physicians and 150 APPs across 35 clinical specialties.
Like many healthcare organizations, Excela was adding APPs to help provide clinical coverage and improve access. Excela recognized that despite the rapid growth of the APP workforce over the previous five years, many APPs were being underutilized in their current roles. This disconnect was due to a lack of a comprehensive workforce planning process and clearly defined APP work expectations when the APPs were hired. The underutilization was affecting not only financial performance but also the ability to recruit and retain APPs.
Excela’s leadership realized that the organization’s inability to tap into the full potential of its current APPs was undermining its current recruitment efforts and ability to increase job satisfaction and retention within its APP workforce.
Committed to getting ahead of the extraordinary pace of change in healthcare, Excela developed and implemented new structures and processes to expand support for the APP workforce, with three broad primary objectives:
- Defining and communicating consistent work expectations for APPs
- Clarifying their role on the care delivery team
- Enhancing the environment for all clinicians
The process
Excela assembled a steering committee of key stakeholders to perform a comprehensive review of its current APP workforce practices. Included on the committee were the chief human resources officer, the COO of the medical group, the chief medical officer, service line leadership and four practicing APPs to represent each major specialty area. Support from finance included:
- Quantification of operating margin and revenue opportunity
- Data extraction for financial modeling
- Post-project financial and metric monitoring
The process was conducted in three phases over a six-month period:
- Assessment and education
- Design
- Implementation
The assessment and education phase included internal surveys and interviews with practicing physicians and APPs to understand their perceptions of the APP culture, utilization and the practice environment. The committee also reviewed cash compensation levels, pay practices and work-effort expectations, and compared the findings with market benchmarks.
Important findings included the following:
- About 77% of the APPs had been working at Excela for less than five years.
- The external turnover rate was 11% (compared with 10% nationally) and the internal turnover rate was very high, at 18.3% (compared with 6.3% nationally).
- Only 38% of APPs perceived themselves to be utilized to their maximum potential.
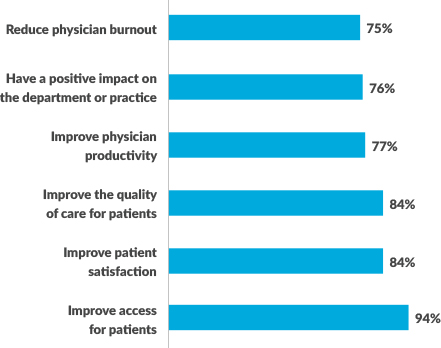
- Physicians perceived that APPs could have a significant impact on patient and organizational outcomes.
- Work expectations for APPs were not clearly defined.
- Despite regular market assessments, compensation had fallen behind local competition and included inconsistent incentive opportunities.
Excela Health survey of how physicians perceive the impact of APPs
Through educational sessions, Excela offered APPs and physicians an opportunity to review these organizational findings and provide feedback. The sessions also covered rules and regulations surrounding APP scope of practice based on updated information from the Centers for Medicare & Medicaid Services and state boards of nursing and medicine.
Using data and insights from these assessments, Excela created a comprehensive APP strategy to help guide the design and implementation phases of the process. The strategy included the creation of the following:
- APP compensation structures based on specialty roll-up and incentive opportunities for all practicing APPs
- Consistent policies regarding on-call and extra-shift pay practices
- Standard work expectations for all APPs based on their respective specialty areas and practice settings
- Newly defined care models within seven specialties (primary care, OB/GYN, orthopedics, sports medicine, cardiology, general surgery and neurology), in which APPs would play a central role in improving financial performance and patient access based on patient needs
- A standardized process for reviewing new APP positions to ensure expectations for each role is clearly identified and communicated with the recruiting team
- A group of APP leaders engaged in all processes and decisions to ensure transparency and APP involvement
The results: Garner new net revenue opportunities
The review process enabled Excela to design a comprehensive roadmap to optimize APP practice, improve APP retention and engagement and drive desired organizational results. Excela’s leaders determined that addressing the following four components within its APP workforce strategy would present potential new net revenue opportunities amounting to as much as $4.2 million.
1 Structure and engagement. Excela began adding more APP representatives to organizational committees and developed a formal onboarding program for APPs.
2 Clarity of roles. The health system defined roles and expectations for all APPs, including work effort (hours, shifts, etc.) and productivity requirements. The goal was to promote effective team-based care and enhance utilization by allowing APPs to practice at the top of their license.
3 Compensation and pay practices. Excela sought to develop an APP compensation plan more closely aligned with team-based goals, physician colleagues and the clearly defined APP work-effort expectations.
4 Communication and transparency. APP leaders were educated about compensation practices and philosophy and involved them in annual market reviews (at a level deemed appropriate). It was determined APPs should receive clear and regular communication regarding their role, expectations and performance.
Following implementation, Excela’s APP year over year turnover rate decreased from 7.66% to 6.58%, representing a 14% reduction. Further, as a result of improved APP utilization, APP productivity improved by 18% through the first six months, resulting $4,323,596 of annualized incremental revenue. The $2,108,035 through the first six months prior to COVID-19 outbreak, exceeded the projected revenue opportunity identified during project discovery. Finally, APPs also were reported to be better engaged as a result of their being more deeply involved in organizational initiatives and having more frequent communication with senior leadership. These advancements have proved valuable in Excela’s initial COVID-19 response.
Excela Health: Pro forma of APP proposed optimization
| Department | Description | Implementation timing | Metric | Baseline metric | Annualized amount* (low range) | Annualized amount* (high range) |
| General | Reduce turnover by 1% to 2.25% annually† | 4/1/2019 | Turnover | 11% turnover | $280,474 | $631,066 |
| Sports medicine | One additional encounter 3-5 days/week‡ | 5/1/2019 | Clinic encounter | 314 encounters/month | $17,833 | $29,722 |
| Neurology | 5% to 7.5% efficiency improvement in outpatient clinics | 5/1/2019 | Clinic encounter | 765 encounters/month | $158,347 | $236,887 |
| Neurology | 10 to 12 additional encounters/day/every other week§ | 4/1/2019 | Clinic encounter | 765 encounters/month | $340,566 | $408,679 |
| OB/GYN | 15 additional encounters/weekend from weekend coverage | 7/1/2019 | Clinic encounter | 0 encounters/month | $178,240 | $178,240 |
| Orthopedics | Hand surgery parallel clinic – incremental visits | 7/1/2019 | Clinic encounter | 0 encounters/month | $96,536 | $193,072 |
| Orthopedics | APP osteoporosis clinic (0.5 Incremental) | 7/1/2019 | Clinic encounter | 0 encounters/month | $214,525 | $429,049 |
| Cardiology | Four to six ambulatory clinic visits/day | 7/1/2019 | Clinic encounter | 482 encounters/month | $214,525 | $321,787 |
| Primary Care | 247 to 309 additional visits/week with standardized schedules | 7/1/2019 | Clinic encounter | 4,281 encounters/month | $1,242,839 | $1,553,549 |
| Gastroenterology | 31 to 46 additional encounters/week | 7/1/2019 | Clinic encounter | 0 encounters/month | $331,526 | $491,942 |
| Total offsets | $3,075,411 | $4,473,993 | ||||
| Orthopedics | Incremental APP to cover ER call and same-day clinic | 7/1/2019 | ($137,333) | ($137,333) | ||
| Orthopedics | 0.5 incremental osteoporosis clinic APP expense | 7/1/2019 | ($68,667) | ($68,667) | ||
| Orthopedics | 0.5 osteoporosis coordinator and annual subscriptions | 7/1/2019 | ($32,496) | ($32,496) | ||
| Total costs | ($238,496) | ($238,496) | ||||
| Net | $2,836,915 | $4,235,498 |
†Excela response to 2018 SullivanCotter APP Organizational Practice Survey; difference between Excela turnover and national average turnover.
‡Based on one additional non-concussion visit as first appointment of the day.
§New outpatient visits on hospital service day (AM, physician; PM, APP).
Source: SullivanCotter, 2018
Lessons learned
Based on Excela’s experience, organizations can benefit from adopting a clear set of principles for successful care team redesign, with engaged APPs:
- Define team-based care models based on patient needs and not individual clinician preferences.
- Seek consistency whenever possible, and allow for variability where needed.
- Ensure APPs work to their full potential and support top-of-license practice.
- Build a culture and infrastructure within the care team that supports the integration, retention and engagement of APPs.
- Measure progress to ensure sustainability.
As healthcare organizations discuss and plan for post-COVID operations, circumstances will compel them to consider adopting a new model of care delivery that supports their ability to help expand access and improve affordability. Excela’s experience can serve as a roadmap for successful integration, utilization and optimization of the APP workforce. With clearly defined roles, goals and work expectations to support top-of-license practice, APPs can play a critical part in driving operational performance and supporting financial sustainability.
Acknowledgement
The authors of this article would like to acknowledge others who contributed to the article:
- Jerod Smith, CRNP, Thoracic and Vascular Services, Excela Health
- Brian Berry, BSN, MS, MBA, Anesthesiology, Excela Health
- Michael Schellhammer, PA-C, Orthopedics, Excela Health
- Andrew Fisher, PA-C, General Surgery, Excela Health
- Joel Villegas, consultant, SullivanCotter
- Tim Loch, CFO, Franciscan Sisters of Christian Charity
4 elements of an APP workforce strategy
The post-pandemic recovery plans should incorporate a comprehensive APP workforce strategy with the following goals in mind.
1. Defining clinical care expectations. Clinical care expectations, such as scope of practice, coverage requirements and patient volumes, are components of work effort required by a clinician to administer the required care. To enable APPs to have the greatest impact, it is critical to ensure these expectations align with patient needs, innovations in care delivery and organizational goals. After COVID-19, for instance, these expectations for APPs may include innovations such as telehealth, and the specific role for APPs in delivery of telehealth services should be clearly defined.
2. Clarifying team roles. As the focus on revenue intensifies, clarifying roles among physicians, APPs and other care team members can help to improve financial performance and maximize value from existing resources. Aligning roles on the care team can help to avoid duplicative activities and ensure top-of-license practice.
3. Controlling expense. Historically, organizations report an APP average external turnover rate of about 10%.[d] With the average direct cost of turnover for each APP position ranging between $85,832 and $114,919, this amount can represent a significant cost for organizations.[e] Reducing turnover can be an attractive target for cost savings. Although turnover is driven by several factors, underutilization is often an overlooked yet important consideration.
4. Enhancing performance. Aligning physician and APP compensation and performance programs with organizational goals can help to drive desired results by improving patient access, satisfaction and quality outcomes while also stabilizing revenue. For example, an aligned quality or access incentive program for physicians and APPs can ensure that the clinical team is working cooperatively as opposed to working under a variety of different and sometimes conflicting goals that can create competition between the team members.
Examples of clinical work expectations for APPs
Production
- Minimum clinical production metrics (e.g., work relative-value units [wRVUs], shifts, collections, and encounters
- Patient facing hours (expectations vary by specialty)
Coverage
- Practice location (e.g., inpatient, ambulatory, operating room)
- Specialty-defined standard hours/shifts
- Call and cross-coverage responsibilities
Documentation
- Timely completion of medical records
- Timely submission of charges
Quality/Service
- Patient satisfaction
- Clinical outcomes
Citizenship
- Meeting attendance
- Participation and adherence to evidence-based medicine protocols, order sets, and other standards
Footnotes
a. Examples of APPs are nurse practitioners, physician assistants, certified registered nurse anesthetists and certified nurse midwives.
b. “Advanced practice providerp compensation programs shifting to address growing market demand and vhanging models of care,” CISION PR Newswire, Feb. 4, 2020.
c. SullivanCotter, Market response to COVID-19: physician and advance practice provider compensation practices survey report, April 15, 2020.
d. SullivanCotter, 2017-2019, Advanced Practice Provider Compensation and Pay Practices Survey Report.
e. SullivanCotter, 2018, Cost of APP Turnover Report.





