Auth-DP software helps streamline prior authorizations to reduce denials
How do you help healthcare organizations navigate the biggest challenges in healthcare?
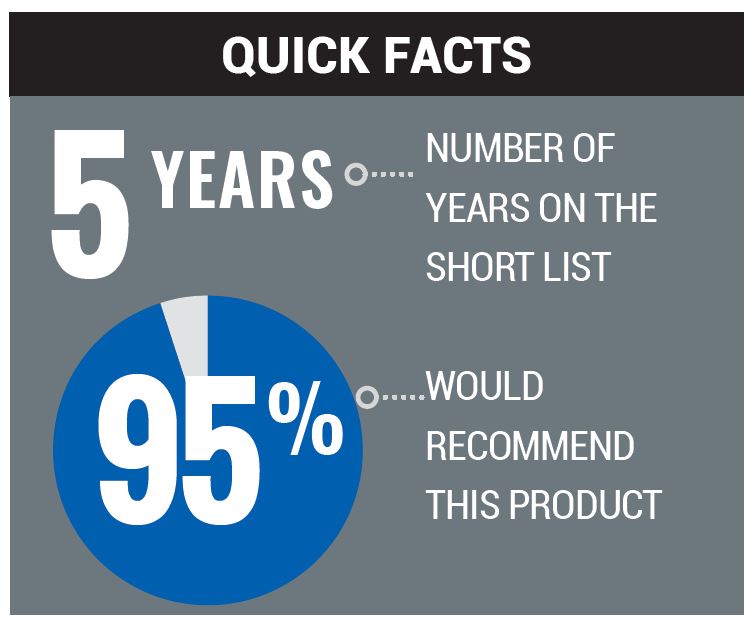
Increasing prior authorization requirements at the payer, plan and procedure code level are putting more burden on providers to ensure proper eligibility and authorization checks prior to patient care. With more complex authorization requirements, manual processes that take upwards of 25 minutes per request are no longer sustainable. Auth-DP, a software suite by Recondo, automates the prior authorization process by determining whether an authorization is required; initiating the request; pre-filling necessary data and submitting the authorization. In addition, the solution regularly queries payers to determine the authorization’s status, so providers can quickly ascertain whether it’s approved prior to a scheduled service.
With Auth-DP, providers increase employee productivity, improve days out on notification of authorization status and ensure authorizations are secured prior to service, drastically reducing authorization denials to the tune of millions of dollars.
What advice would you offer to healthcare leaders when choosing among vendors?
Make sure the software vendor has a deep library of authorization-related rules, as this revenue cycle area is highly complex and depends on deep mapping of requirements down to the plan and procedure code level in many cases. Validate that the vendor has expertise and experience in building a comprehensive rules library and can demonstrate the solution’s expected value. This information can be gleaned through a business impact analysis or other ROI calculator that uses the client’s actual historical data and average results from similar clients.
In addition to assessing a vendor’s technical experience, also verify its subject matter expertise. Often solution vendors will bring a technology approach to a problem when processes or workflows may be contributing factors to the issue. Implementing technology solely for technology’s sake is not going to deliver the results that provider organizations need or expect. Having product or implementation team members who have worked in healthcare facilities is crucial as these knowledgeable experts can offer the practical experience needed to drive improvement. Finally, ensure you and the vendor are aligned in your priorities and you have a structured approach to implementation to lay the groundwork for success from day one.
What is some advice you can give providers for a successful implementation of a new product or service?
Prior to implementing technology, perform an assessment of current workflows, processes and tools to identify issues and address those before onboarding new technology. In addition, we find that education and training are crucial. Without it, staff may avoid using a new technology because they’re afraid of a mistake that will affect their performance. Training and education go a long way in ensuring success.
Recondo
Recondo Technology, now a part of Waystar, offers an AI-powered software-as-a-service (SaaS) platform that helps healthcare providers achieve sustainable financial performance while delivering a better patient experience. Leveraging purpose-built AI in the forms of robotic process automation, machine learning, and natural language processing, Recondo delivers industry-leading automated, accurate, and actionable financial clarity to the healthcare revenue cycle. Recondo empowers more than 900 hospitals with solutions that connect providers, payers, and patients to ensure revenue cycle efficiency across the care continuum. The company’s patented software and expertise streamline operations, allowing providers to be paid more, faster, and at a lower cost.






