Getting to the root causes of denials
- Telling the story of why a denial happened in the first place begins with understanding the reason, the issue and ultimately the root cause.
- The root cause should be written in a way that enables the reader to act on a specific cause with little additional study.
- Collect valid data based on actual root cause rather than only relying on the reason codes returned by payers.
Despite dedicated efforts, the steady rise in claim denials is a mounting concern for hospitals, health systems and physician practices. A review of denial and audit data can help providers prevent errors that lead to denials, and in the process reduce financial loss and increase resource efficiency.
3 emerging trends call for a proactive denial and appeal strategy
A proactive approach is essential to identifying root causes as the basis for denial management and prevention. Here are three trends to know:
1. Clinical validation. We’re seeing an increase in clinical validation denials that are based on a combination of clinical indicators and coding references by the payer. Placing clinical validation under the coding umbrella further complicates the appeal process.
2. Payer targets. Payers tend to focus on 10 to 12 diagnoses. Knowing those focus areas is critical to flagging records for more in-depth review. Use of data analytics to identify the diagnoses that show the highest denial rates and revenue risks is the foundation for building a proactive denial prevention and appeal strategy.
3. Managed care contracts. Breaking down silos extends beyond coders and physicians to include managed care. Organizations are increasingly focused on how diagnoses are defined in managed care contracts and the impact on payer denials.
Using denial data to identify root causes — reason, issue and root cause
Telling the story of why a denial happened in the first place begins with understanding the reason, the issue and ultimately the root cause. Claim Adjustment Reason Codes (CARC) are used to communicate a reason for a payment adjustment — why a claim or service line was paid differently than it was billed.
One of the most common reasons cited is “not deemed a medical necessity by the payer.” But what is the true issue? For example, denial issues can be related to coding, documentation or incorrect status. While CARCs and audit issues describe why the payer or auditor is not paying for a service or claim, the root cause is the confirmed or potential internal failure that caused the variance in payment for the service or claim. What did the organization do to cause the denial?
Whereas denial or audit issue data is typically readily available and easily identified through claims data analysis, identifying the root cause requires internal analysis of the medical record, charges and the billed claim to determine the potential root cause or internal failure. Root causes should be defined operationally to determine the level of analysis required internally.
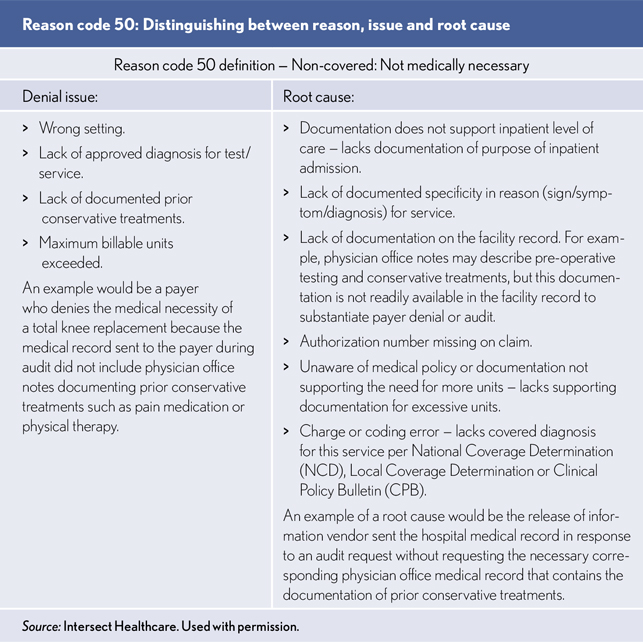
An example of a root cause would be the release of information vendor sent the hospital medical record in response to an audit request without requesting the necessary corresponding physician office medical record that contains the documentation of prior conservative treatments.
Writing a specific root cause is important
The root cause should be written in a way that enables the reader to act on a specific cause with little additional study. For example, writing “Documentation does not support inpatient level of care,” is a broad statement and could encompass many different problems, yet we often see it used as a root cause. While the denial issue is intended to be a broad category, the root cause should be as specific as possible to pinpoint the problem that needs to be corrected to prevent the denial from recurring.
For example, a root cause could be lack of documentation of two midnights expectation for a traditional Medicare admission. Another specific root cause could be lack of documentation of recovery sooner than expected, which would be required for an inpatient traditional Medicare admission that doesn’t pass the two midnights.
Avoiding denials based on actual root cause versus reason codes
To avoid denials, it is important to collect valid data based on actual root cause rather than simply relying on the reason codes returned by payers on 835 remittances and explanation of benefits. When properly collected, analyzed and reported, this information can be used to:
- Identify patterns and trends that inform denial management strategies.
- Define the service site, service type, payer and possibly physicians where issues originate and offer education and training to decrease denials caused by internal failures.
- Communicate with payers to establish specific contract terms regarding payment and appeal rights.
The benefits of a technology approach to denials management
Integrating denials management, analytics and technology solutions can help organizations accomplish the following goals:
- Determine the root causes of payer denials
- Capture coding and clinical validation changes
- Provide targeted education on the front end of the revenue cycle
- Increase knowledge of payer contract terms to mitigate risk
- Move from payer denial management to prevention
- Centralize workflows for unified denial management and appeals
Breaking down silos — a multidisciplinary model
Root cause analysis requires breaking down silos through a multidisciplinary approach that promotes honest discussions about internal processes that may require re-education, training and revision. The goal of data analytics is to identify and quantify preventable errors on the front end before they become denials on the back end.
To achieve that goal, your core team should include leadership from coding, patient access, utilization management, managed care, revenue cycle, clinical documentation improvement, health information management, legal, compliance and any additional representatives from areas involved in denial management. Provide ongoing education and bring payers into the conversation. Identify the roadblocks, the biggest issues.
To determine which denials you can prevent, go deep into the data using interactive reports. Meaningful data can provide a valuable roadmap for establishing a denial management process.
With consistent and timely review of denial and audit data and ongoing communication regarding the root causes of denials and audit findings, providers can reduce financial loss and unnecessary resource consumption by preventing errors that lead to denials.





