Aligning for a Sustainable Healthcare Future
A report on HFMA's 2025 Thought Leadership Retreat

Segments of the U.S. healthcare system often operate at cross purposes, meaning improved alignment will be vital to achieving systemic progress.
Fragmentation is apparent not only between payers and providers or clinicians and administrators, but also in the tension between efforts to innovate while keeping care cost-effective, and between formulating policy and putting it into practice.
“Bridging these divides is essential to improving access, affordability and financial sustainability,” said C. Ann Jordan, JD, president and CEO of HFMA.
HFMA’s 2025 Thought Leadership Retreat highlighted creative and practical opportunities for solutions. The 18th annual event, held Sept. 25-26 in Washington, D.C., gathered leaders representing various healthcare segments to discuss ways to enhance stakeholder alignment.
“We find ourselves at an existential tipping point,” Jordan said. “On one hand, innovation is accelerating at a pace beyond what our current structures and payment models can contain. On the other hand, policy shifts in Medicaid and the [Affordable Care Act], misaligned stakeholder incentives and eroding public trust are shaking the foundations of our system.”
In a poll asking attendees to pick the biggest obstacle to realizing true systemic alignment, the leading choice in the resulting word cloud was reimbursement, followed by issues such as cost and trust. Those roadblocks can be overcome through collaborative efforts that promote shared incentives and an understanding that true reform should center on how all parties can best serve the patient.
The following were some of the pivotal areas of discussion among thought leaders and attendees at the retreat (see below for the sidebar on attendee discussions, and to download the full report, click the cover image above).
1. New sources of strain
Ongoing healthcare policy developments are not expected to help the sustainability or alignment of the healthcare system. The 2025 budget reconciliation bill known as the One Big Beautiful Bill Act (OBBBA) has been projected to increase the pool of uninsured Americans by 10 million over a decade.
That’s on top of a demographic trend that will funnel an ever-increasing share of limited resources toward the Medicare population over the next 10 to 15 years, said James Mathews, PhD, a policy expert and principal with Health Policy Alternatives, and formerly executive director of the Medicare Payment Advisory Commission.
“The drill is going to be figuring out how to do more — and in many cases much, much more — with less,” Mathews said.
Hospitals and health systems already are in a collective bind amid many of the constraints that have been apparent since the COVID-19 pandemic, said Praveen Mekala, MBA, the CFO of Lahey Clinic, part of Cambridge, Mass.-based Beth Israel Lahey Health. Margins are narrowing and cash flow is tightening.
“The word unprecedented gets tossed around quite a bit,” Mekala said. “I wouldn’t say this is an unprecedented time, but it is definitely an extreme time.”
Nonprofit community health plans could face existential challenges due to the looming OBBBA cuts, said Ceci Connolly, president and CEO of the Alliance of Community Health Plans, and that could lead to a consolidation of the market around a handful of national insurers.
“If you think you would like more choice, more competition and a local nonprofit that does not answer to shareholders, that’s one reason you need to be very concerned,” she said.

2. The payer-provider opportunity
Payers and providers can respond to the challenges by aligning around a business model that gives all parties incentives to promote prevention and population health management, Connolly said.
“Let’s get away from hospital as the goal and [get to] health being the goal,” she said. “And there’s a huge, huge role to play in that partnership when you get upstream.”
Other worthy steps include unifying patient messaging and simplifying billing and eligibility processes, Connolly and Mekala said. Meanwhile, federal policy should move past the current focus on check-the-box Medicare quality measures that emphasize processes, instead assessing quality through the prism of outcomes.
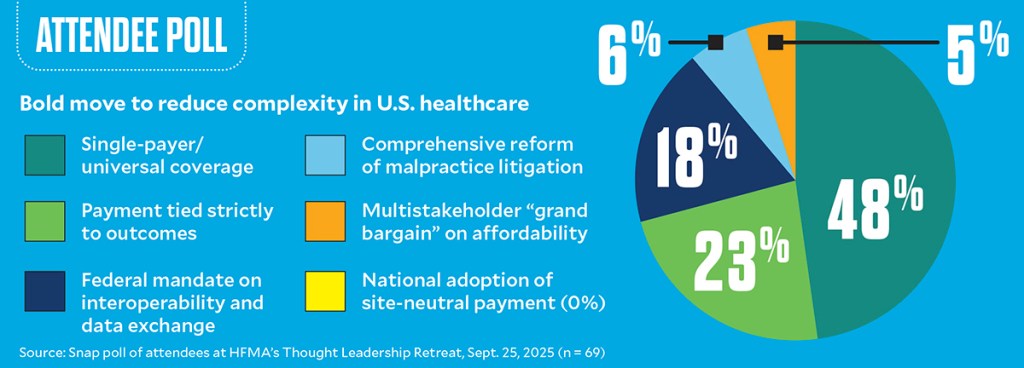
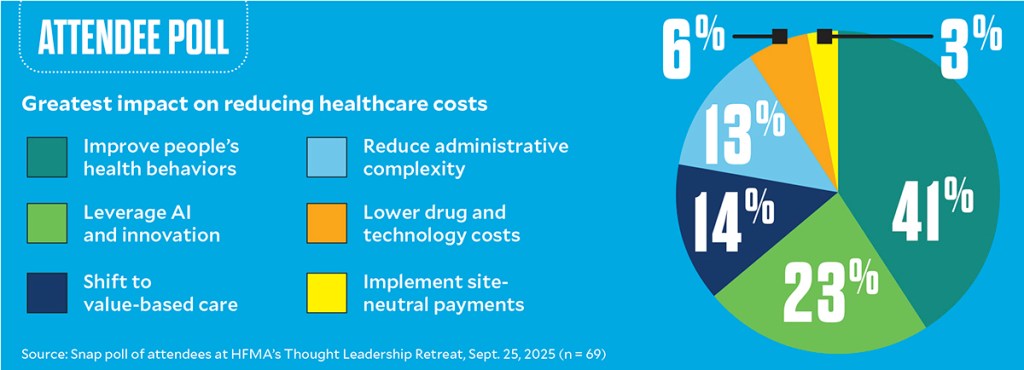
In polling (see below), a plurality of Thought Leadership Retreat attendees picked single-payer healthcare as a bold reform that would reduce systemic complexity. Payment tied to outcomes was another leading choice, followed by federal interoperability mandates.
Interoperability would be an especially compelling step toward improved alignment, Mekala said.
“That’s a big driver of the complexity, [the] administrative burden right now,” Mekala said. “When you think about plan-provider, regulatory [issues] around clearance [and] eligibility, there’s no standardization on the back and forth.”
A concept that could increase the level of cohesiveness in the system while bypassing the political controversy and potential drawbacks of a single-payer system is a multistakeholder “grand bargain,” Mathews said.
The idea would entail aligning incentives across a person’s lifetime by achieving better synchronicity among Medicare, Medicaid and commercial payers.
“While that person is in the charge of a given entity, that entity should be doing what they can to maintain that person’s health on a proactive basis,” Mathews said.
3. The physician-administration dynamic
The healthcare system tends to spawn silos, whether the divide is between physician specialties, physicians and nurses or clinicians and administrators, members of a physician leadership panel said. Collaboration across all clinical and nonclinical professionals is critical to ensuring truly patient-centered care.
A care episode can turn complex when coordination falls short, said Peter Angood, MD, president and CEO of the American Association for Physician Leadership, describing the barriers potentially encountered in a scenario where the patient moves among the emergency department, operating room (OR), ICU, general nursing floor and hospice.
For example, each surgeon or proceduralist wants unique instruments, workflows and teams, said Claude Brunson, MD, an anesthesiologist. Continuity can be tenuous even within the OR because of individual-clinician preferences that may be coupled with routine ancillary-staff shift changes during the day.
“Where’s the standardization? Should the teams be standardized? All of these are [considerations] that should go on when getting a patient into a complex care environment where we’re going to perform a surgical procedure and then aim for that care event to come out with a good outcome,” Brunson said.
When looking at the clinical sprawl of the healthcare system, it’s easy to see why misalignment can be the norm. Said Angood, “How do you coordinate and align 160 different physician specialties in your system with all the 75 other clinical job types and ensure that good quality patient care happens consistently?”

4. The case for physician leadership
One organizational strategy that can increase cohesiveness is preparing physicians for leadership roles. Physician leaders can connect the clinical and administrative realms strategically, but only if the physician develops the level of administrative competency needed to be credible.
Brunson experienced the challenges when transitioning to an administrative role at the University of Mississippi Medical Center. He strived to retain close ties with the clinical workforce while also proving himself to fellow administrators who had taken a more traditional route to their positions.
“If you can successfully bridge that, you’re bringing two very important parts of the health delivery system together, and [colleagues] are respecting that individual clinician [and thinking] it’s a good thing that you were a clinician,” Brunson said.
When physicians get into administration, he added, they develop a greater appreciation for the challenges of managing a healthcare system. That gives them a perspective they can communicate to their colleagues.
“The frontline clinicians almost all the time want to do the thing that’s right for the patients and families,” said Michael Lalor, MD, MBA, president and CEO of Trellis Supportive Care in Winston-Salem, N.C., and clinical assistant professor of medicine at Wake Forest University. “However, at an organizational level, there may be things that have to go in a different direction.
“To see on a day-to-day basis how we can then bring this back to the staff and let them know the importance of the direction we’re going relative to the desires that they’re looking for, I think [that communication] becomes key to success.”
5. The nursing-finance dynamic
Nurses’ role in care delivery makes their participation in organizational leadership essential. Yet, as with physicians, integrating clinical and financial perspectives can be challenging.
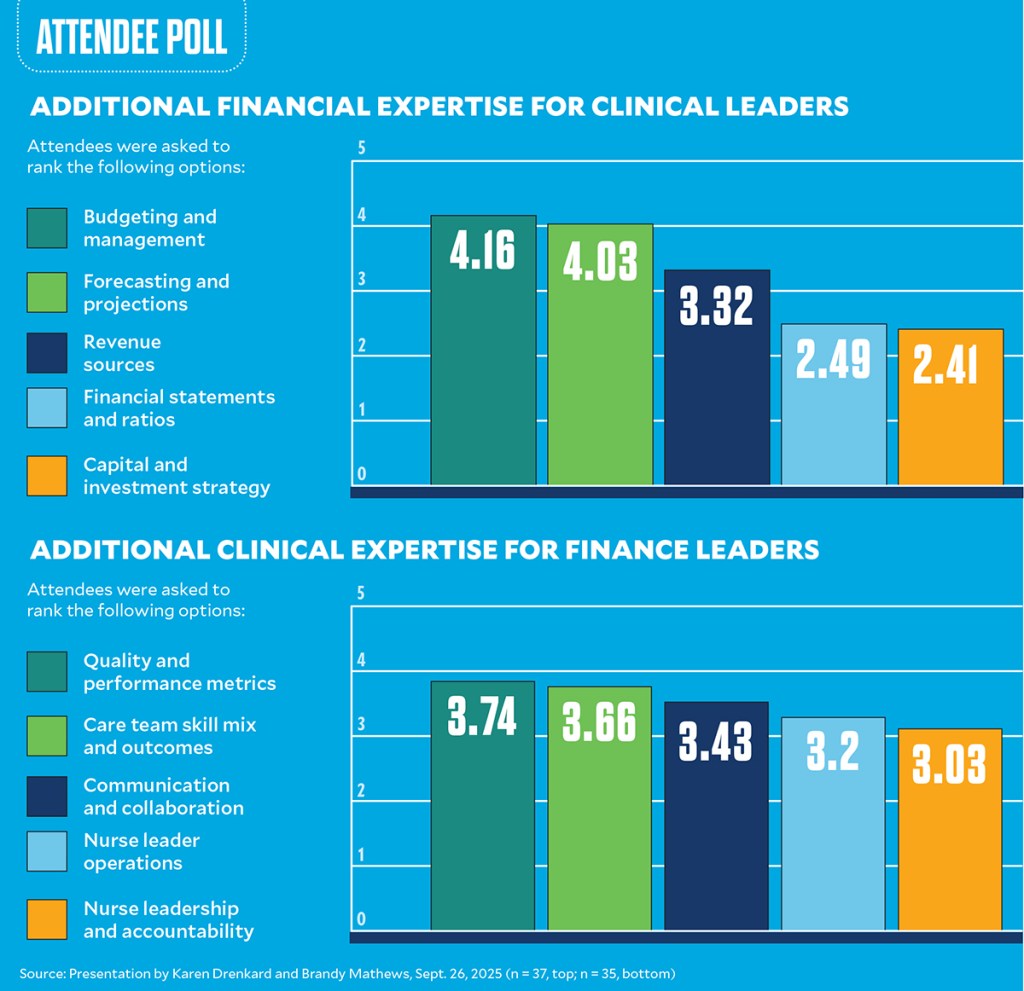
In audience feedback conducted during a presentation by representatives of the American Organization for Nursing Leadership (AONL), the financial expertise of clinical leaders was viewed as limited. Areas in which clinical leaders can bolster their financial acumen in the context of healthcare operations, according to responses, include budgeting and expense management, forecasting and projections, revenue sources, and financial statements and ratios (see below).
Similarly, finance leaders’ understanding of clinical operations was viewed as surface-level. Room for growth includes additional knowledge in areas such as quality and performance metrics, the skill mix and outcomes of the care team, and communication and collaboration.
“Creating some sort of a shared language between the two [leadership disciplines] is going to be important,” said Brandy Mathews, DNP, chief nursing officer with UK HealthCare for Good Samaritan Hospital and Emergency Services.
That work can help nurses gain financial fluency and finance leaders to become familiar with the operational and clinical impacts of their decisions, said Mathews and Karen Drenkard, PhD, a healthcare strategy consultant and AONL board member.
Nurses and finance leaders share the underlying goal of ensuring affordable and sustainable healthcare and wellness, Drenkard said. When differences emerge, that’s due to diverging areas of focus such as clinical outcomes and margin management.
6. Areas of common ground for nursing and finance
AONL aims to close the gap between the two disciplines via various initiatives, including a Nursing Value and Impact Subcommittee, which was convened to generate policy recommendations based on the idea that nursing is not a labor cost center, but rather human capital that yields measurable value if it receives appropriate levels of investment. That notion is often obscured in traditional accounting systems, Drenkard and Mathews said.
In collaboration with Todd Nelson, HFMA’s director of partner relationships and chief partnership executive, AONL continues to advance tools such as the Span of Accountability Index for nurse managers and the Nursing Resources ROI calculator. These allow leaders to analyze quality and operational data, calculate returns on nursing investments, and build a clear business case for staffing, technology and resource allocation.
Collaborative principles should extend beyond simple civility to affect operational behaviors, Drenkard and Mathews said. Clinical and finance leaders should cooperate on developing shared targets and definitions of value and engage in joint decision-making rather than unilateral cost-cutting.
“Nurses want to be financial stewards, too,” Drenkard said, noting that financial health supports patient care and the clinical mission. In addition, strong interdisciplinary relationships can help the organization avoid blunt labor-cost reductions.
“Nobody wants their health system to be in the red,” she said.

7. Forward thinking on sites of care
Notable progress toward aligning with patients will come from finding better ways to meet them where they are. Home-based care programs are a key step in that direction.
“We do very little truly patient-centered care, if we’re really honest with ourselves,” Bruce Leff, MD, professor of medicine at Johns Hopkins School of Medicine and a pioneering researcher of models including hospital-at-home, said during a session that also featured leaders with the Institute for Healthcare Improvement.
In Leff’s vision, “If someone needs a primary care visit in the home, they get it. If they need hospital-at-home care, they get that in the home. [When] they are finished with their acute episode at home, now you can do the rehabilitation at home and build it all out of there.”
Several decades of research, including randomized controlled trials and national demonstrations, have revealed significant benefits of hospital-at-home in metrics of costs, outcomes and patient satisfaction.
Even so, adoption of the model often is slowed by cultural and technical barriers. Challenges include capturing ROI when savings accrue to Medicare or society at large rather than to an individual hospital.
Organizations may grasp how to implement a home-oriented care model yet still not appreciate “how challenging it is to change hardwired behaviors,” Leff said. “I’m not even talking at the meta level. A lot of the Excel sheets that you all use in evaluating opportunities for new programs, that’s an example of the hardwired stuff.”

8. Transformation in rural healthcare
For rural healthcare organizations, opportunities to align stakeholders and improve sustainability could emerge from the $50 billion Rural Health Transformation Program (RHTP).
The RHTP, which was funded by the OBBBA, will pay out up to $10 billion per year to states between 2026 and 2030. The idea is to “catalyze needed change in rural health systems and not necessarily perpetuate the status quo,” Emily Chen, MBA, a senior advisor with CMS’s Office of the Administrator, said during a presentation. (For up-to-date coverage of RHTP funding allocations, visit HFMA’s news feed.)
The program marks the largest-ever rural health funding effort, Chen noted. As part of a cooperative agreement with the federal government, states can expect close monitoring and continuous technical assistance while maintaining the flexibility to implement tailored improvement initiatives that best serve their populations.
Progress will be formally measured through annual outcomes reporting, and interstate collaboration to share best practices for applying the funding is encouraged.
States can use the funding to improve rural population health through various initiatives, Chen said. For example:
- Promoting prevention, behavioral health and chronic disease management
- Supporting sustainable access via rural clinical networks and centers of excellence
- Enhancing workforce development through local healthcare training pipelines and rural residencies and fellowships
- Implementing value-based care programs aligned to rural settings by using the funding to front the startup costs for such models
- Incorporating technology such as telehealth, consumer tech and improved infrastructure for interoperability
The fund is meant to jump-start initiatives that will outlast the five-year window, Chen emphasized.
“Successful initiatives from this program may serve as a [platform] for future policymaking and legislation, and so we’re really excited about the possibilities,” she said.

9. Profound changes from AI
Regarding opportunities to improve the healthcare system, AI brings ample promise along with a bit of peril.
The ongoing era for AI is one where “science fiction becomes science fact,” said Jose Morey, MD, founder and CEO of Ad Astra Media LLC.
The technology is not eliminating clinicians but rather augmenting them, he said. Even as the Food and Drug Administration has approved more than 1,000 AI tools over the last 15 years, demand for physicians and specialists has increased.
Aviation presents a blueprint for how clinical settings can use AI, said Morey. Commercial aircraft essentially fly themselves, but there are two pilots with rigorous training in control of every cockpit.
“If you can actually create an AI system that truly democratizes healthcare and eliminates medical errors, if this is actually given to everyone, to the entire populace, this could be very game changing, both from a cost perspective, but then ultimately from a family perspective,” Morey said.
Drug discovery timelines could shift from years to minutes or seconds through AI and quantum computing, and scientists are engineering new amino acids — the building blocks of life — by editing DNA and teaching bacteria to manufacture the new compounds.
Future smart homes could continuously monitor a person’s vital signs, negating the need for the wearable devices that have become mainstream in recent years. And specialty care could increasingly migrate from the hospital to primary care, community settings and patients’ homes.
Such developments “could completely change the concept of what a modern-day hospital system may be,” Morey said.
In that context, a company like Amazon or Facebook might have the capabilities to fill the void that would arise if rural hospitals struggle to maintain operations amid ongoing financial strain, he added.

10. Final words on aligning to improve healthcare
A closing session at the retreat focused on pervasive problems and realistic solutions.
“I see [the] days cash on hand of these hospital systems. It’s declining and it’s frustrating,” said Allen Gracey, MBA, CPA, vice president and head of healthcare with Visa. “It really says this is our call to action [for] how we can attack that and make it sustainable from a financial standpoint.”
Fundamentally, “The system rewards heroic care,” said Alex Ding, MD, MBA, deputy chief medical officer with Humana. “We underinvest in prevention, chronic disease management and sustaining quality of life. And I would argue, from where I sit on the payer side, really the payment structure is not fit for purpose.”
A better financing system could be envisioned as “health as a subscription service,” he said, aligning incentives toward prevention and sustainable health.
In addition to drastic technological change, healthcare leaders should acknowledge demographic shifts, with millennials outnumbering baby boomers, said Nick Patel, MD, a strategic advisor for Abridge. Younger generations want healthcare on demand, similar to watching shows on Netflix, and are more likely to seek out behavioral healthcare.
“The technology needs to move with us,” Patel said. “The policies need to change in regard to: If we’re going to really start to rely on AI and automation, gen-tech processes, then we need to have tort reform as well” to clarify liability issues around AI.
Asked what types of changes could make a difference, the panelists cited strengthening primary care, advancing digitization of billing and payment processes, collaborating across different organizations, and applying technology to develop practical solutions rather than simply chasing state-of-the-art tools.
“Leadership doesn’t require having all the answers,” HFMA’s Jordan said. “Just the courage to move forward amid uncertainty and work collaboratively.”
Takeaways from attendees
Breakout discussions involving attendees, whose roles span administrative, clinical and policy leadership positions with providers and health plans, are an annual staple of HFMA’s Thought Leadership Retreat. Here’s a sampling of the insights that came from the discussions on improving alignment to achieve a more sustainable healthcare system.
Aligning strategy and policy. Healthcare policies should promote whole-person care, including behavioral health, while recognizing that the industry’s complexity and inelastic demand make pure free-market solutions impractical. Behavioral economics can be leveraged to encourage healthier choices among consumers.
Reducing complexity and administrative burden. Complexity can be managed by streamlining regulations, addressing malpractice risk and shifting prior authorization to be supportive rather than obstructive. Standardization of key information (e.g., on insurance cards) could represent a quick win for the industry.
Using technology to realize progress. AI’s most immediate value lies in reducing administrative tasks and clinician burnout, with efficiency gains the easiest way to gauge ROI. However, complex AI systems are expensive, risky and evolving rapidly and must offset labor costs to be financially sustainable.
Improving affordability. Affordability depends in part on shifting away from a system that rewards heroic medicine toward one that supports appropriate, patient-centered care. Greater trust between payers and providers is key to enabling alternative payment models that are viable and impactful.
Looking toward the future. Looming pressures — such as Medicare insolvency, accelerating costs of commercially insured care, and advances in AI — could be the shocks that drive meaningful healthcare transformation. Care must evolve toward patient-driven choice and convenience, with one-stop-shopping solutions for comprehensive needs like dementia care.
Thank you to our sponsors
HFMA thanks Abridge, Aspirion, Humana, Innovaccer, SuperDial and Visa for their support of the 2025 Thought Leadership Retreat.











