Reimagining The Patient-Caregiver Relationship
By Nick Hut, HFMA Senior Editor
At the center of efforts to improve the U.S. healthcare system, the patient-caregiver relationship must become more holistic, seamless and personalized, say health system leaders and industry experts.
In that quest, the Chesterfield, Missouri-based Mercy system has implemented a new artificial intelligence-based pilot to identify patients with diabetes who need A1C tests, with those patients receiving text messages that encourage them to get tested. The innovation is an example of an analytical approach to targeting high-risk patients while there’s still time to prevent a chronic condition from escalating.

overstretched, nurses who are hard to find.”
— Cheryl Matejka, CFO at
Mercy, Chesterfield, Missouri
Mercy CFO Cheryl Matejka said the program has improved outcomes for the health system’s 10,000-patient panel.
The program also bolsters productivity for clinical teams that are increasingly stretched thin. Instead of making separate phone calls to inform patients of a diabetes diagnosis, direct them to get tested and discuss the results, a physician can convey the important information in one call. Interactions with patients become more personal, efficient and substantive.
In the absence of the program, “It’s mind-blowing to think of how many additional care hours we would have spent for physicians who are overstretched, nurses who are hard to find, medical assistants who are hard to find,” Matejka said. “Anything that we can do to take non-value-added work off their plate can only help.”
Such approaches represent a step forward for a clinical model that would benefit from fundamental changes.
“The patient-clinician relationship needs to be reframed and reoriented,” said Zeev Neuwirth, MD, an author and podcast host and the chief clinical executive for care transformation and strategic services at Atrium Health. “It’s an outdated model.”
The push isn’t happening only out of an awareness that the system too frequently fails to meet the needs of patients and prospective patients clinically and financially. There’s also intensifying concern about a workforce that has been sapped by the COVID-19 pandemic.
The needed changes span clinical and operational processes, payment models and technological innovations. The targeted result, Neuwirth said, should be a continuous, contextual relationship in which physicians act as expert consultants, utilizing team members and technology to proactively identify health issues that can be addressed in a clinical setting, at home or virtually.
Contrast that with the current state of the relationship, which in many cases is reduced to a 15- or 20-minute consultation “in a 10-by-10 box called an exam room,” Neuwirth said. “And you don’t even have [clinicians’] undivided attention because they’re spending much of their time documenting and checking boxes.”

A matter of survival
Clinicians who don’t adjust to a new paradigm for patient relationships may find themselves getting phased out of an industry that’s being transformed by technology.
— Joel Selanikio, MD, based in Washington, D.C.
“Most of the people within tech believe, as I believe, that 10 years from now, 20 years from now, healthcare will be addressing a much smaller set of things than it currently does,” said Joel Selanikio, MD, a physician and TED speaker.
“The pie — or, as the military says, the area of reference — for healthcare will get smaller and the area for tech will get bigger,” Selanikio said. “Certain things that people have traditionally done with doctors will not be done with doctors. It’ll be you and your phone, or you and your virtual-reality headset, or your watch or your wearable.”
Patients will continue to require acute care in specialized settings, and no one necessarily expects to establish a true relationship with clinicians who provide those services. Where clinicians should focus on optimizing the relationship is the area between that space and the expanding range of health-related activities, such as weight control, that conceivably will fall within the bounds of self-care.
Such a scenario leaves treatment of chronic conditions as a part of healthcare in which the clinician-patient relationship will be pivotal.
“It’s even more going to be focused on folks who have conditions where they have to see the same doc each time,” Selanikio said. “The normal wellness kind of stuff, people will find, can be much more efficiently and effectively addressed by other methods.”
Even before such changes take hold, the patient-clinician relationship has to evolve to meet the changing expectations of healthcare consumers.
In a Kaufman Hall report this year on healthcare consumerism, a key finding was that a “disconnect exists between consumers’ health management activity and their healthcare providers.” Survey results in the report show 70% of more than 3,500 respondents wanted providers to more actively support health management activities in areas such as nutrition and exercise.
The financial parameters of a new landscape
Although the new model for patient-clinician relationships will require clinicians to change their approaches to patient engagement and hone their skills, the most fundamental needed changes are systemic.
For starters, the fee-for-service payment structure is not conducive to establishing the type of clinical model that meets the consumer expectations articulated in the Kaufman Hall report
A volume-driven payment model “is not supportive of the actual purpose and mission of the work,” Neuwirth said. “The mission of primary care, and I would say many specialties, is not to churn patients and click RVUs. The purpose is actually to keep people healthy and prevent them from needing more care downstream.”
Payment structures should better support the more extensive interactions that would be central to Neuwirth’s vision of the physician-as-shepherd model. Value-based payment (VBP) is vital to promote preventive care in particular.
In acute settings as well, today’s predominant payment models aren’t conducive to helping clinicians meet population health challenges. VBP better supports processes that address disparities and fill identified care gaps.
“It helps us care for patients regardless of where they are and really study where we potentially have care that we can get ahead of to help those patients,” Matejka said.
Revamped key performance indicators need to accompany new payment structures, Neuwirth said. It’s still uncommon for clinical staff to be measured on and primarily reimbursed for their ability to keep patients out of the emergency department (ED) or the hospital, to avoid readmissions or to reduce the total cost of care by improving clinical and nonclinical determinants of health.
Behavioral data science: A burgeoning field of study looks at how to connect with consumers

“We still don’t understand what motivates individuals, what’s important to them, what’s the activation that’s required for us to be able to really engage individuals more in their own self-care.”
— Steve Miff, PhD, president and CEO of the
Parkland Center for Clinical Innovation
Steve Miff, PhD, president and CEO of the Parkland Center for Clinical Innovation, views three prongs as essential to providing the best possible patient care: clinical expertise, holistic approaches that encompass social and personal determinants of health, and behavioral data science.
The study and application of the last of those is still in the early stages.
“We still don’t understand what motivates individuals, what’s important to them, what is the activation that’s required for us to be able to really engage individuals mor in their own self-care,” Miff said. “There are things such as somebody’s capacity for self-care, their behaviors, their preferences — that whole component of how consumer make decisions.”
Those insights are far more advanced in other sectors, such as retail, where the ability to sell products hinges on a company’s ability to read its customers. “That’s our biggest opportunity,” Miff said. “It’s something that we’ve identified to double down on and start to see if we can understand much better through data.”
Once those insights are in hand, he added, a corollary question becomes: “How do we reach patients in a way that’s hyperpersonalized and conducive to them?”
Elements of a new clinical template
The evolution of the patient-clinician relationship is ongoing and sweeping. Experts say clinicians need to adopt models that promote coordination, digitization, customization, accessibility, and comprehensive and team-based care.
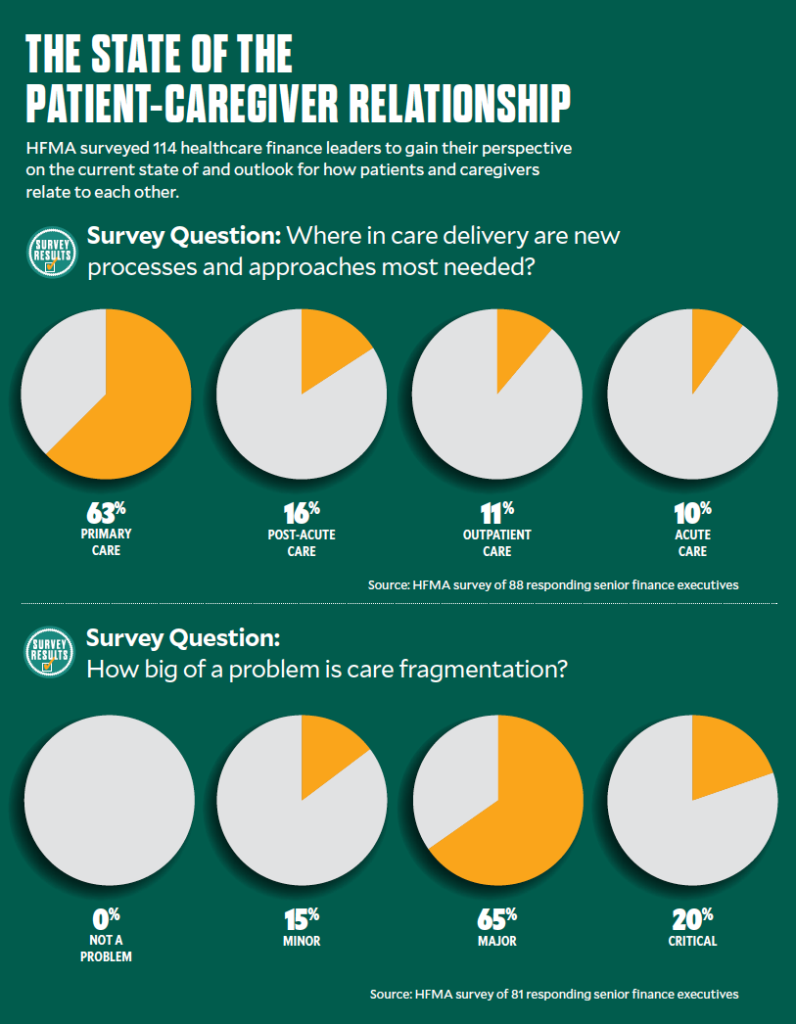
Coordination. The lack of coordination in U.S. healthcare has been a persistent hindrance to effective clinical operations. Among respondents to an HFMA member survey, for example, 85% said fragmentation is either a “critical” or “major” problem.
As stakeholders search for solutions, they should start by examining the lack of integration in their own operations, said Steve Miff, PhD, president and CEO of the Dallas-based Parkland Center for Clinical Innovation (PCCI). An independent, not-for-profit organization, PCCI strives to both serve the healthcare needs of its community and pursue transformative initiatives that can have an industrywide impact.
PCCI uses data to identify broad clusters of patients who have clinical, socioeconomic and demographic characteristics in common. Integrated practice units care for specific clusters — bringing together “the right specialties, support services, you create a virtual behavioral health consult and are able to holistically bring all those together to treat the whole person,” Miff said.
One issue for the healthcare system to address is the void specifically in ambulatory settings of care coordination resources such as mental health and social work support, said Cynthia Barginere, DNP, RN, COO at the Institute for Healthcare Improvement (IHI), Boston. If organizations struggle to implement such capabilities, they can consider utilizing the services of vendors that connect patients to post-discharge social resources.
Digitization. Clinical teams will need proficiency in digital technology to keep up with trends in remote monitoring. Data from wearables and other monitoring devices will have to be rapidly collected and analyzed, with teams proactively responding to the findings in real time.
“It requires a centralized model because you need to be able to do it 24/7,” Miff said.
Such models have a proven track record at PCCI-affiliated Parkland Health & Hospital System in efforts to prevent ICU admissions or deterioration of patients with sepsis. Miff said the same approach can work with remote monitoring and hospital-at-home programs once organizations learn how to apply algorithms to risk stratification.
“If you have over a hundred patients, you want to know the 10 who you need to pay attention to right now versus going down the line until you get to the hundredth and then starting over again,” he said.
Customization. In an HFMA survey of healthcare finance leaders, 62.5% cited primary care as the setting in which the need for new processes and approaches is most urgent. One issue with primary care is that many clinicians and staff are expected to be equally adept at caring for 28-year-olds and 88-year-olds, Neuwirth said.

— Zeev Neuwirth, MD, chief clinical executive, Atrium Health
Patient segments such as seniors and women would fare better if care specialization for those groups were routine, he said. For example, data has shown the impact of senior-focused practices such as CareMore Health and Iora in keeping patients out of the ED.
Segmentation and customization thus become central to optimal care. Teams should be geared clinically, operationally and from a business-model perspective to take care of specific groups, Neuwirth said.
Furthermore, the pandemic has driven home that “cultural insensitivity and even racism are built into the system,” he said. “It’s not even about the individuals [working in healthcare]. We really have to put in systemic interventions and protocols. You could talk about it, and you could even do training about it, but you have to protocolize this and get it embedded so that the system actually helps the provider to help the patient.”
To provide optimal treatment to an increasingly diverse patient base, the clinical workforce itself needs to become more diverse. That comes down to “having a very sincere effort and a very specific effort from the pipeline all the way through the system,” Barginere said. (As described in the report 10 Steps Toward Health Equity, produced from a 2022 HFMA event for industry thought leaders, racially concordant care is seen as vital to reducing disparities in health.)
Accessibility. Clinical leaders increasingly are focused on removing obstacles to obtaining in-person healthcare that’s convenient, readily available and high-quality.
A single parent with a full-time job might not make it back for a crucial follow-up visit at a clinic that’s open only during standard business hours. Clinical teams should be able to proactively identify such barriers and find solutions or workarounds, including through collaboration with community resources such as transportation outlets or daycare agencies.
“We need to be able to have those workflows to follow up and connect that individual to those services,” Miff said.
Comprehensive care. Clinical operations are looking to incorporate processes with which to address social determinants of health (SDoH).
“You hope that your doctor will take the time and talk to you about your life,” Neuwirth said.
But even if physicians can overcome the constraints of the FFS payment system and find that time, he added, “They have not been trained, and there’s no protocol to help them figure out what those contextual factors are.”
At Mercy, community health workers are embedded in the ED to help clinicians guide patients in “getting to a proactive place in terms of their care” after they depart, Matejka said.
SDoH factors are an emphasis in those interactions. For example, patients with asthma receive guidance on addressing triggers in their home in addition to getting needed treatment. ED clinicians also are provided with resources that help them direct patients to behavioral healthcare settings as needed.
Team-based care. Building a distinct team around the physician will become increasingly common as more organizations look to address disparities and SDoH issues with help from staff such as social workers and health coaches. Physicians thus need to do a better job helping patients understand the team concept.
“If you don’t introduce members of your team as part of your core team, the patients may engage with them differently,” said Timothy Johnson, MD, system vice president of clinical integration with SSM Health in St. Louis.
A point especially worth clarifying is that advanced practice providers (APPs) such as nurse practitioners and physician assistants have authority to treat patients even if they’re technically under the supervision of a physician.
“For so many things, having them see the advanced practice providers that I partner with is so much faster and equally effective,” Johnson said. “I can focus on the sickest of the sick, and my APPs can take care of the less acute patients, which means they get faster care — and they still get great care.”
Grasping the notion of team-based care also will help more patients embrace remote health monitoring instead of thinking they should travel to consult with a physician for every situation that arises.
A sea change that’s underway
Neuwirth doesn’t see the advancement of the patient-clinician relationship as a pie-in-the-sky scenario. On the contrary, he said, it’s already happening in ways that are more profound than most people could have anticipated even a few years ago.
The onus now is on legacy providers to keep pace.
“In the 30-plus years I’ve been in healthcare, I’ve never seen this type of tech enablement and positive energy around this movement,” Neuwirth said, citing disrupters such as Laguna Health, CVS Health and Walmart, and integrated payers such as Optum and Humana (see Part 3 of the series), all of which are innovating to center healthcare on the consumer.
“These are the most analytically sophisticated, consumer-oriented [companies] with incredible vertical integration of various assets and capabilities. And they’re part of this transformative movement,” he added. “And so, I’m super-excited, not primarily from a clinical, business or tech perspective, but from a humanitarian perspective.”
That’s because the ongoing transformations “will rehumanize healthcare. They’ll improve not only access to healthcare, but the experience of healthcare and health for all.”
Addressing burnout as a vital step to better care
Clinician burnout was a problem before the pandemic and has grown in urgency since. The issue leads to suboptimal care by contributing to staffing shortages and reducing the effectiveness of clinicians during patient encounters.

at the Institute for
Healthcare Improvement,
“Some of the noise in the system prevents [clinicians] from having that feeling of joy associated with the work that they’re doing,” said Cynthia Barginere, DNP, RN, COO at the Institute for Healthcare Improvement (IHI), which promotes the healthcare Quadruple Aim of lower costs, better population health, better patient experiences of care and better clinician experiences of care.
“Hospitals and health systems can take a step back and start to really listen to the workforce as they describe where some of those pain points are within the system,” Barginere added. “I think we did a really good job of that during COVID, where we actually asked staff: ‘What are some of the things that are just ridiculous that would give you back time, give you the opportunity to really sit and have a conversation with your patient?’”
Technology and predictive analytics can be used to support decision making, she said — not to replace critical judgment, but to ensure important information is readily available so physicians don’t need to rely on memory. But organizations need to implement technology in a way that supports staff rather than stymies them.
Barginere asked, “Are we actually using human factors science to ensure that the way we’re using technology is consistent with how humans behave, and what works for them, and building it into workflows as opposed to layering it on top?”
Documentation burdens and redundancies are another area that needs addressing, she said: “Could we take some of the waste out of the system by not having the same people asking [a patient] the same questions throughout the system, [thus] making it easier for clinicians to do the work?”
Another key issue affecting clinicians’ mental and emotional well-being is the reported rise in violence in clinical settings. In a poll conducted this year by the American College of Emergency Physicians, for example, 85% of emergency physicians said the rate of violence had increased in the past five years.
“That’s traumatic for all clinical staff,” said Steve Miff, PhD, president and CEO of the Parkland Center for Clinical Innovation (PCCI). “You walk into a patient’s room and have no idea who you’re going to interact with and what’s going to happen. Can we use AI and predictive algorithms to give a sense of the risk that you are going to have a violent event, and how do you actually deescalate proactively and prepare?”
Leadership approaches also make a difference in burnout mitigation, said Timothy Johnson, MD, system vice president of clinical integration with SSM Health. As a clinical leader, he inquires with staff about what brings them joy, and prods them to offer something specific and actionable beyond just “taking care of patients.” From there, leadership can take steps to create such an environment for the clinician.
Said Barginere, “We would get a lot further in even just the engagement of clinicians [if they] know, ‘You mean you really want to know what I think? You’re really going to make changes based on what I tell you is important?’”