How Texas Health Resources improved patient access and preservice revenue
Texas Health Resources, a major nonprofit health system based in Arlington, is a top performer on key patient-access metrics. By the date they receive services, 95% of scheduled patients are preregistered, authorizations have been secured for 98%, and health coverage status has been resolved for 100%.
The health system’s Patient Access Intake Center (PAIC), with about 95 full-time employees, fields more than 550,000 telephone calls a year and, in 2018, collected $13.5 million in patient preservice revenue.
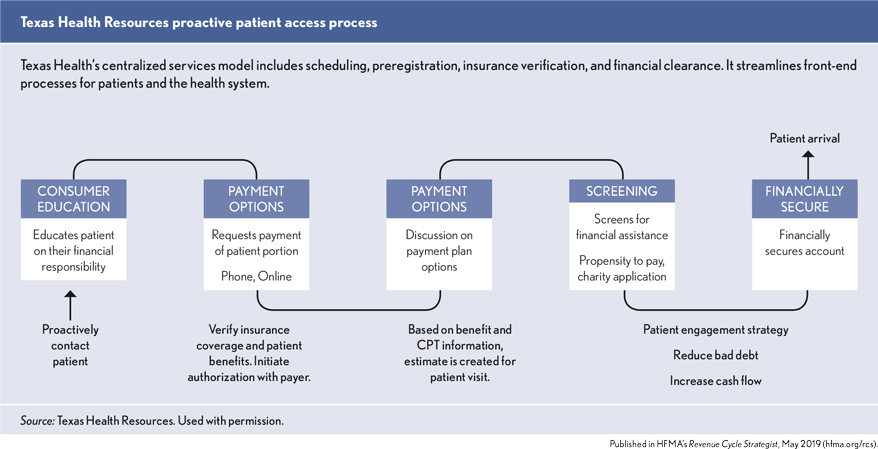
Patti Consolver, senior director of patient access in system services at Texas Health Resources, says centralized services — scheduling, preregistration, insurance verification and financial clearance — can streamline front-end processes for patients and the health system. Here’s how it works at Texas Health
Reducing patient hold time
The majority of scheduled patients are scheduled by their physician offices. However, patients have the ability to self-schedule their procedures, such as radiology, either through the patient portal or via telephone with the Enterprise Scheduling department.
If a patient’s health coverage can be easily verified during the telephone call, and the patient’s out-of-pocket responsibility will not pose a challenge, the scheduler can quickly preregister the patient. However, in most cases, schedulers forward the calls to the PAIC for preregistration or financial clearance because there may be more tasks necessary to financially secure the account than can be accomplished on the portal or the initial call with the Enterprise Scheduling department. That avoids long hold times that patients often experience when the same person handles both scheduling and preregistration.
As soon as patients are scheduled, schedulers are free to take another call. As part of preregistration, patients are asked how they intend to pay estimated out-of-pocket costs. If necessary, patients are referred to a member of the financial clearance team, who can determine if patients are eligible for financial assistance or help arrange payment plans.
Aligning workflows for the patient experience
Texas Health has been on a journey to centralize many of its ancillary functions so that consumers have a seamless experience accessing and navigating through the health system regardless of hospital location. In order to do this, Consolver adds that it was important to communicate and help educate physician offices and other entity departments on the roles and responsibilities of each of the centralized areas.
For example, Consolver recalls situations in which physicians’ offices complained to a hospital that an insurance authorization was not completed in a timely manner. Hospital leaders assumed that the PAIC was to blame, when, in fact, health plans require that physicians initiate authorization requests — that responsibility is not the access center’s purview.
For that reason, Consolver works to make sure hospital and physician-office administrators understand the PAIC’s work. “It’s important that they understand the role of your team — and what they are responsible for,” Consolver says.
Her department provides pamphlets to physician offices so physician office staff members can help educate their patients on how to preregister.
Download the Texas Health Resources preregistration pamphlet.
“As soon as the decision is made that the patient needs to have a procedure at one of our hospitals, they can give the pamphlet to the patient to explain the steps needed to get scheduled and preregistered,” she says.
The pamphlet informs patients on the following tasks:
- How to self-schedule appointments either by telephone, e-mail or patient portal.
- How to request cost estimates by phone.
- How to preregister online, by telephone or by e-mail.
- How to pay outstanding balances, set up payment plans and/or take care of other billing issues.
The pamphlet alerts patients that they will be expected to pay estimated out-of-pocket costs before service as part of the preregistration process. “We will get you registered, collect any estimated costs and get an authorization for your insurance all before the day of your appointment so you can have a stress-free experience,” it reads.
Incorporating best practices
A big benefit of centralized front-end processes is increased efficiency. When staff worked in individual hospitals, they were able to preregister, on average, three to four patients per hour, Consolver says. When centralized auto-dialing technology was adopted, that average rose to between five and six patients an hour.
Success factors for Texas Health include the following elements:
Teleworking. Top performers can work from home three days a week. About 40% of Texas Health’s insurance-verification staff and about 25% of the preregistration staff meet the criteria.
To qualify, staff members must have consistent high levels of productivity — at least 5% higher than the all-staff average; have no corrective actions in their performance records and have near-perfect quality scores. “These are folks who are self-sufficient, have most likely been in the role for a good period of time and have a history of top performance outcomes,” Consolver says. “And if they are not able to continue meeting that same performance level when they work from home, they are brought back into the office and re-evaluated.”
See related sidebar: 2 tech tips for efficiently contacting patients
Call labs. “Due to advances in consumer-focused technology, the entire preservice journey can be captured electronically from the point of scheduling until the patient leaves the registration area. This continuous flow of information allows us to conduct monthly call labs with staff to review the patient experience and constantly improve,” Consolver says.
The recordings are also useful for “call lab” training and retraining patient-access staff. Recorded calls can be used to demonstrate excellent customer service on the phone or how to handle unusual situations.
Addressing consumerism
Creating a preservice center with financial clearance as an integral step can help organizations address consumers with greater financial needs while remaining competitive and mitigating revenue loss. By centralizing scheduling, preregistration, insurance verification and financial clearance, Texas Health Resources has streamlined front-end processes and improved patient experience.
Interviewed for this article:
Patti Consolver is senior director, Texas Health Resources, Arlington, Texas, and a member of HFMA’s Lone Star Chapter.
Melanie Ann Thorsen is an application specialist at Texas Health Resources





