How a health system can realize tangible benefits from its digital health strategy

Many health systems today are intent on developing and implementing an effective digital health strategy, and their CFOs are likely to play a prominent and collaborative role in this effort.
To achieve success in digital health, a health system likely will first need to address the issue of governance. For many health systems, the path to success starts with creating a new leadership role of chief digital officer (CDO) and then forming a three-way alliance and governance model involving the CDO, the CFO and the chief medical officer (CMO).a Here, we discuss key considerations these leaders need to collectively address to ensure their organization’s digital transformation produces real value for patients and the health system’s physicians and staff.
It’s not just about geography anymore

Health systems are undertaking a digital transformation because they realize the traditional geography-driven business strategy is no longer adequate to address their current circumstances. They are no longer simply delivering healthcare in a physical location that is the sole consideration driving consumer behavior. Consumers today, both patients and providers, expect more differentiated experiences, accessible through a choice of either physical or digital means. Much as retail businesses offer grocery or merchandise pick up, combining digital and physical access, health systems should aim for a hybrid model that allows for a similarly differentiated experience. Digital experiences can be offered, for example, through care delivery, automated processes and education.

Digital is a product business
Organizations that have chosen to go digital should realize that their new outputs are differentiated digital products that include experiences. Ultimately, a product should have the following characteristics:
- An end-to-end experience
- Independence of modality
- The ability to generate demonstrable ROI over a relatively short timeline
For example, a knee surgery or an oncology episode treatment starts with education, research and possibly a consultation. These steps are followed by diagnosis, treatment and post-treatment management, ultimately leading to improvement in vitality or quality of life. Many of these steps can be accomplished digitally, while some in-person steps can be augmented through digital experiences.
In fact, when such a process is integrated across physical and digital products and experiences (as the retailers have been doing now for some time), it may be possible to achieve better outcomes than can be achieved with strictly in-person experiences. (See also the online sidebar “5 phases to designing and operationalizing a digital product” at hfma.org/hfm for a discussion of development and implementation phases of a single digital product.)
Implications for the senior finance executive
With any fully developed digital strategy, it clearly is not enough to develop just one product. Health systems should have multiple products aligned to a set of key service lines that can be differentiated in their markets. Building a portfolio of such products will require an investment period followed by growing returns, yielding a traditional J-curve such as is shown in the exhibit below . The key is to create the right mixture of a portfolio to shorten the time required to realize value and to reduce the depth of initial investment.
Collective J-curve of portfolio containing multiple products
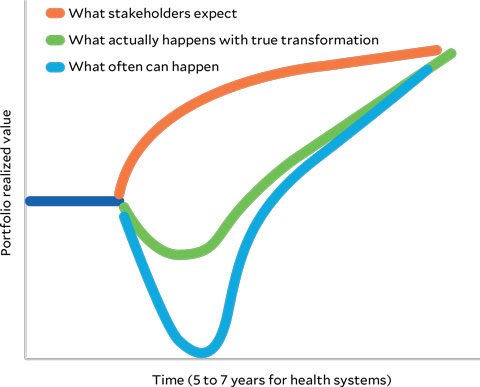
The expectations for a portfolio and diff erent possible results depicted here are based on the authors’ experience and observations of common behaviors both in healthcare and other industries.
In their oversight role in this strategic undertaking, the senior finance leader should ensure the organization adheres to the following key operating norms for promoting high performance and optimal governance for such a product portfolio.
- 1. Ensure the mindset is product-centric, as opposed to project-centric. The cardinal mistake of most health systems pursuing a digital strategy and encountering challenges to do so quickly is to lose focus on individual products. Developing a product (whether an orthopedic surgery experience or immediate virtual care visit) should be seen as a journey that will continuously evolve with the preferences of consumers. A project has partial resources allocated to it that often are stretched thin, and it has an end date. Products endure, evolve and earn value by keeping in step with consumers.
- 2. Strategically invest capital expenditure (CapEx) funds. Health systems can capitalize any digital product they build as appropriate. Each organization has its own nuances for sizing and allocating capital budgets (e.g., based on its own accounting policies and the impact on its bond rating), but capitalizing always should be considered when it serves the organization’s overall financial health projecting forward.
- 3. Combine budgets from a few departments. Product investment should never be relegated to one department only. Ideally, clinical operations and IT should share the budget for an internal joint venture. In addition to assigning joint ownership over financial outcomes, joint budgets create the critical mass required for success.
- 4. Pick at most half a dozen key performance indicators (KPIs), including financial ones. Too many KPIs make a new operating model even more difficult to attain. Keep it simple, and ensure there are a few lagging indicators tied directly to financials, such as incremental revenue or margin gains.
- 5. Plan to scale operations and financials together. Health systems often are riddled with numerous successful pilots that cannot be scaled, especially financially. Speed to generate experiences for customers is important, but scale is just as, if not more, important. The operations and IT team should have a plan in writing that can be associated with a financially scalable plan. A critical next step is to create and adopt a disciplined approach for tracking performance to ensure accountability.
2 more essential ingredients: Patience and perseverance
Realizing tangible value from digital health products is a new challenge for health systems that cannot be met overnight. But by following these five guidelines with patience and perseverance, and with appropriate buy-in from their fellow C-suite executives, health system finance leaders can ensure their organizations’ digital strategies will be successful.
Footnote
a. Forming this alliance was the topic of our column “Crossing the chasm on digital transformation” in the March 2021 issue of hfm.





