‘A just cause’: HFMA’s CEoH initiative addresses the factors that impede quality of health and raise healthcare costs
Preventing the preventable is a phrase HFMA members likely will hear often in the year ahead as HFMA moves forward with a global effort to encourage the creation of efficiencies and processes that keep people healthy and reduce the costs of care and care management.
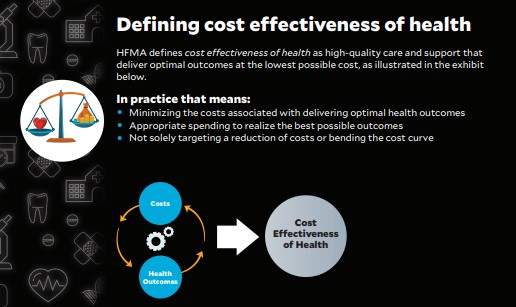
Focused on the concept of cost effectiveness of health (CEoH), the goal is to develop a system for care that is needed, accessible and affordable.
“Cost effectiveness of health is essentially about keeping people healthy,” said Joseph J. Fifer, FHFMA, CPA, HFMA president and CEO. “It’s about minimizing the impact of chronic conditions on the health of individuals and on our economy and society. By ensuring optimal health outcomes at minimal cost, we can refocus the value chain on health.”
It’s about minimizing the impact of chronic conditions on the health of individuals and on our economy and society. By ensuring optimal health outcomes at minimal cost, we can refocus the value chain on health.”
— Joseph J. Fifer, HFMA president and CEO
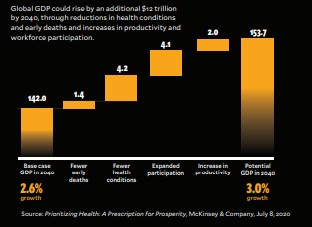
The emphasis on health, rather than healthcare, is intentional. Research by McKinsey & Company shows that more than 40% of health improvements can be achieved with a net cost of just $100 per additional healthy life year. Better health — which can be achieved in part through interventions that improve population health — also promotes economic growth.
Even efforts to reduce headache frequency in people who suffer from chronic migraines could mitigate the socioeconomic impact of migraines, estimated at $100.4 billion in decreased productivity per year, while providing substantial relief to migraine sufferers, research shows.
But those are just a few reasons why a broader focus on improving cost effectiveness of health — not just healthcare — should be a strategic priority for healthcare leaders. For healthcare finance leaders, it’s an opportunity to shape solutions for optimizing health spending rather than risk having new models for cost effectiveness imposed on them.
A societal imperative

“This is an issue that is much bigger than the healthcare industry,” said Tammie Jackson, FHFMA, CHFP, HFMA Chair. “Today, 80% of health hinges on social, behavioral and environmental factors. It’s going to take cross-sector collaboration to address the risks associated with social determinants of health. It will also require that every individual become personally accountable for their own health.”
Jackson also underscored the need for collaboration on a global level. “Right now, everyone is trying to solve for some version of cost effectiveness in their own way,” she said. “By working collectively with stakeholders in different industries and healthcare colleagues around the world, we can develop much more comprehensive and sustainable solutions that provide value.”
The mathematics of healthcare spending are very familiar to U.S. healthcare finance professionals. Nationally, healthcare expenditures comprised 19.7% of U.S. gross domestic product in 2020, which equates to $4.1 trillion, or $12,530 per person, according to CMS. As the rate of spending continues to climb, national healthcare spending could reach $6.2 trillion by 2028.
“Healthcare costs will be the No. 1 campaign issue in 2022 and beyond, and the healthcare industry needs to develop a better response,” said healthcare policy analyst Paul Keckley. “It’s not enough for healthcare leaders to say, ‘It just costs more because it does.’”
Given that the federal deficit totaled nearly $2.8 trillion in fiscal year 2021, healthcare must be part of the solution in reducing that debt.
“I think it’s mathematically inevitable that if we don’t make the long-term financial investments to support cost effectiveness of health, efforts to reduce healthcare spending will happen to healthcare organizations, rather than organizations being at the center of this work,” Fifer said. “Why shouldn’t healthcare finance professionals lead these efforts?”
Competitive incentive
Market forces also dictate that the move toward CEoH must become a strategic priority for health systems. Consider that Walmart is not only expanding its healthcare footprint in underserved communities, but also collaborating with health systems to combat food insecurity, which puts individuals at increased risk for adverse health outcomes.

executive and author
Healthcare disruptors like One Medical, Oak Street Health, ChenMed and Village MD are attracting patients in primary care, an area that presents strong opportunities to reduce healthcare costs through better access to care and care management. These disruptors have captured millions in private equity dollars from investors who are keen to make money by moving the needle on health costs.
Meanwhile, payer-provider partnerships between health plans and large systems are rising in some markets, driven by a desire to strengthen access to care, quality of care and cost management.
In this environment, healthcare leaders who delay making bold moves toward achieving CEoH could put their future at risk, experts say. “The longer you wait, the longer it’s going to take,” said Zeev Neuwirth, MD, chief clinical executive for care transformation and strategic services, Atrium Health. “And the question is, where is that going to put you in the market at that point in time?” Neuwirth is also the author of Reframing Healthcare: A Roadmap for Creating Disruptive Change.
How to begin

To embark on this journey, leaders must begin to think more broadly about health and well-being.
“How do we enhance the well-being of individuals by not only treating them when they are sick, but helping them lead healthier, happier, more productive lives?” said David Johnson, CEO, 4sight Health. “We need to care as much about promoting health and preventing disease as we do about cost-effective treatment of disease.”
Getting there will require not just a shift in mindset, but also a collaborative emphasis on:
- Eliminating fragmentation in care
- Developing partnerships that proactively meet individuals’ whole-health needs
- Reevaluating the ways in which CEoH is incentivized, and developing new models for value
- Providing social supports for vulnerable populations — including virtually
- Committing to learning from other providers around the world in assessing what works, what doesn’t and next steps that could bring healthcare closer to this goal
“Collectively, we can begin to compile a much more comprehensive approach,” HFMA Chair Jackson said.
Non-standard partnerships
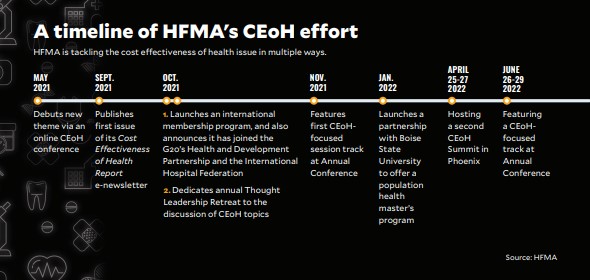
HFMA’s efforts to lead work around CEoH formally kicked off with a Cost Effectiveness of Health Summit in May 2021, which focused on opportunities to achieve a more sustainable model for delivering healthy outcomes at lower cost. Now, as HFMA expands membership to include countries beyond the United States and the United Kingdom, members will gain an opportunity to share learnings on delivering value from around the world.
“People all over the world are talking about this topic,” Fifer said. “While our country spends more on healthcare than other countries, we’re farther along in adoption of value-based payment than other countries, even though we still have a long way to go,” he said. “We also have much to share when it comes to quality of inpatient care and patient safety. So, there is mutual learning that can occur on a global scale to achieve this aim.”
An economic boost
In 2022, HFMA also will seek what Jackson calls “nonstandard partners” — organizations and companies outside healthcare delivery — to sound a drumbeat for change and lead efforts to achieve cost transformation.

Richard L. Gundling, FHFMA, CMA, senior vice president, healthcare financial practices for HFMA, anticipates that this work will complement HFMA’s research around improving value in healthcare as well as the Association’s decades-long commitment to promoting a more consumer-centric approach to care, communications and billing. He also envisions that the Association could one day provide training and certification around CEoH, much as it does in the areas of revenue cycle and healthcare finance.
Leaders acknowledge that the work ahead will not be easy. “This is a cultural shift in thinking about health costs,” said Mary Mirabelli, senior vice president of strategy for HFMA. “Our job is to bring awareness to this issue and make it clear why this is a matter of strategic importance for healthcare leaders at every level.”

president of corporate strategy
Mirabelli said the effort could be considered a “just cause,” which has been defined as a specific vision of an ideal state of the future that inspires people. “It is about doing something good for society by focusing on health, and invites many new constituencies into the effort,” she said. “Just think about how many of us it will take to make this a reality. It is incredibly inspiring.”
The change in emphasis from cost effectiveness of healthcare to cost effectiveness of health is expected to prompt new ways of thinking. Over time, Mirabelli said, the hope is that these efforts will provide healthcare finance professionals with the tools to engage team members across their organizations in making this transformation.
Healthcare finance professionals are uniquely positioned to provide the vision for this effort. “I don’t see how this will happen if we don’t have finance playing a major leadership role,” Neuwirth said. “You need a multidisciplinary team to inform this effort, from clinical to operations to technology. The finance folks have the experience and the wisdom and the technical skill to determine not just how to make cost transformation initiatives happen, but also to sustain them.”
It’s an opportunity for healthcare finance professionals to help guide the future of healthcare delivery.
“There are many organizations that could lead this effort, but few are doing it,” Fifer said. “We have the courage to go for it.”