Why success in cost reduction is a matter of trust
Achieving and sustaining healthcare cost savings depends on trusted data and clinician engagement, but some organizations struggle to find the right mix.
The financial punch of the pandemic continues to depress hospital margins, demanding that healthcare organizations tighten their focus on cost reduction this year. But hospital leaders say they face internal barriers to cost reduction — and it’s holding them back from cost saving success.
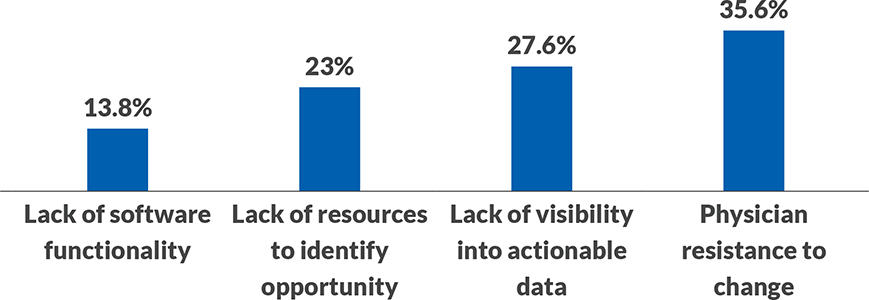
Sixty-three percent of respondents to an HFMA/Craneware survey say their biggest barriers to achieving cost savings are physician resistance to change and lack of visibility into actionable data. Yet just 31% of organizations always involve clinicians in these discussions. Further, more than half are seeking to improve their cost analytics solution.
“Healthcare leaders can’t tackle cost reduction without support from clinicians, and they can’t engage clinicians unless they provide data that clinicians trust,” said Pietro Ferrara, senior vice president, Craneware. “To move the needle on cost reduction, leaders must seek ways to more actively engage clinicians in discussions around cost. They also must strengthen their ability to help clinicians visualize cost-savings opportunities and understand the action steps needed for improvement.”
Deepening relationships and data insight
The survey found that organizations that more frequently engage clinicians in discussions around cost reduction are better prepared to achieve their cost-reduction goals.
“Clinical and financial collaboration is one of the conduits to cost-savings success,” said Richard Gundling, senior vice president for HFMA. “When leaders take the time to obtain clinician input regarding savings opportunities, they come away from these discussions with a better understanding of why cost variance exists. They also build connections with clinicians that heighten engagement and lead to longer-term success.”
For example, consider a hospital where two physicians performing heart valve replacements at a large hospital achieve nearly the same margin per case. However, a deeper dive into the data reveals that Physician A’s patients have ICU stays that are 26 hours longer, on average. Meanwhile, Physician B uses more expensive drugs to treat heart-valve patients.
“While the math shows a similar overall margin per case, having a costing solution that adopts an activity-based costing methodology tells a different story,” Ferrara said.
At this hospital, leaders shared the analysis with the physicians, who were not aware that such differences existed. Physician A was targeted to reduce ICU time by 50% with small modifications. Meanwhile, Physician B learned that his colleagues used other brand-name drugs that were less expensive yet achieved similar outcomes.
“The hospital saved nearly half a million dollars with this process improvement project,” Ferrara said. “So many times, clinicians do not have access to this level of actionable information. It would have been easy for the hospital to look at margin alone. By using an activity-based costing system to examine where variances existed, leaders were able to share insights and data that the physicians trusted, and it led to decreased costs and better care.”
Eighty percent of survey respondents agree that cost reduction should be a strong focus for their organization this year, with nearly 58% saying they are equally focused on cost reduction and revenue enhancement (exhibit not shown).
However, one-in-three respondents say they are not well-prepared to achieve cost-reduction goals.
Further, 56% plan to make changes to their cost accounting solution within the next year, another indication that leaders aren’t satisfied with the degree of insight they currently receive. (See the exhibit below.)
These deficiencies — combined with the low percentage of organizations that always involve clinicians in cost-savings discussions — put organizations’ efforts to reduce expenses and bolster their bottom line at risk.
“Healthcare has been very late to the game in involving those who are directly involved in operations — from physicians to nurses to technicians — in expense reduction,” said Neal Peterson, CRCR, sales executive, Craneware. “In other industries, like manufacturing and the automotive industry, it’s intuitive to approach people on the production line to uncover opportunities to reduce costs.”
For cost reduction to happen at the resource level, clinicians need data they can relate to and trust — for example, clinical operational data rather than revenue cycle data. The data also should enable physicians to make comparisons to their peers, internally and externally.
Healthcare leaders identify biggest barriers to cost-savings success
When thinking about your cost reduction strategy, what is your organization’s single biggest barrier to success?
The move toward activity-based costing
More and more, healthcare organizations are finding that traditional methods for making cost-cutting decisions, such as ratio of costs to charges (RCC) or relative value units (RVUs), do not provide the level of accuracy they need.
“RCCs can lead a hospital to believe a service isn’t profitable when it actually is,” said Naveed Ismail, vice president, customer management, Craneware. “The data also aren’t meaningful to clinicians, as they don’t reflect all of the activities involved in caring for a patient, providing a less-than-complete picture of a clinical event.”
Instead, activity-based costing, which captures each service in the patient journey, provides a more accurate picture or resource consumption. It uses clinical, financial and operational data to capture costs at the individual encounter level.
However, even among organizations that have begun to use activity-based costing, some still show room for improvement.
“We spoke with one health system that incorporates some elements of activity-based costing, but staff perform them manually — and it takes them weeks to gather the information and analyze the data,” Peterson said. “If you have an application that can support you in that effort, you can produce more results and more actionable information, which is key to gaining clinicians’ trust.”
Ferrara likens the difference between costing approaches as the difference between doughnuts and croissants. “Finance professionals have been selling doughnuts to the C-suite for a long time, but in a post-pandemic world, doughnuts no longer make the cut,” he said. “Moving from RCCs to activity-based costing is like going from doughnuts to croissants: It’s a dramatic switch, but it is more effective, and it provides the clinical operational data that physicians and clinicians seek.”
But gaining the most from an activity-based costing solution requires that health systems have access to data analysts who are experienced in marrying financial, clinical and operational data to capture a holistic view. They must also be committed to engaging clinicians in discussions around profitability, rather than asking clinical leaders to make blanket cuts, such as across-the-board expense reductions of a certain percentage.
Restoring trust for a better bottom line
How can healthcare finance leaders best engage clinicians in cost-cutting initiatives? Following are three approaches to consider.
Determine whether you have the staff expertise to deploy an automated solution effectively. Most organizations do not have the bandwidth to stand up an activity-based costing tool on their own. In purchasing an activity-based costing solution, leaders should look for a tool that is easy to implement and light on infrastructure requirements, such as cloud-based solutions that can refresh data quickly. They should also partner with a vendor that can teach them how to use this tool well. Without this education, organizations will struggle to make the most of their investment.
Prioritize which areas to measure. Activity-based costing is resource-intensive, and organizations might not have the data analytics support to examine all areas at once. Determine which service lines present the highest areas of concern related to resource consumption and variation in care. Then, assemble a team of clinicians who can help you dig deeper into the data, uncovering nuances in care that can add expense without significant improvements in quality.
Meet with clinicians in these areas regularly. Once you’ve determined your top areas of focus, meet with clinicians at least once every two weeks to discuss the data and examine where opportunities for cost improvement exist. This keeps the group’s efforts top of mind, helping to ensure that clinicians are invested in the project. It also builds trust between finance and clinicians and buy in around the data itself. When the data view presented accurately reflects the patient journey, finance and clinicians will be better positioned to not only reduce cost, but also improve value.
About Craneware
Craneware (AIM: CRW.L), the leader in automated value cycle solutions, collaborates with all U.S. healthcare providers to plan, execute and monitor financial and operational performance so they can continue to drive better outcomes for the communities they serve. Craneware’s Trisus platform combines revenue integrity, cost management and decision enablement into a single SaaS-based platform. Our flagship solution, Chargemaster Toolkit®, continually earns KLAS recognition in the Revenue Cycle – Chargemaster Management category and is part of our value cycle management suite, which includes charge capture, strategic pricing, claims analytics, patient engagement, revenue recovery and retention, and cost and margin intelligence solutions. Learn more at craneware.com
This published piece is provided solely for informational purposes. HFMA does not endorse the published material or warrant or guarantee its accuracy. The statements and opinions by participants are those of the participants and not those of HFMA. References to commercial manufacturers, vendors, products, or services that may appear do not constitute endorsements by HFMA.






