An organization’s consumer strategy must change with the times
Consumerism remains a high priority in healthcare, but healthcare organizations should be prepared for priorities to shift in the wake of changes brought about by the coronavirus pandemic affecting both work practices and patient behavior, according to a recent survey conducted jointly between HFMA and CareCredit.1
The survey, conducted in October 2020, included 44 total questions answered by 296 HFMA members. Of those respondents, 40.5% were directors, 18.6% managers or supervisors, 17.2% CFOs, 9.5% vice presidents and the remainder a mixture of presidents, controllers, assistant or associate vice presidents, or other leadership roles.
Responding to patient struggles
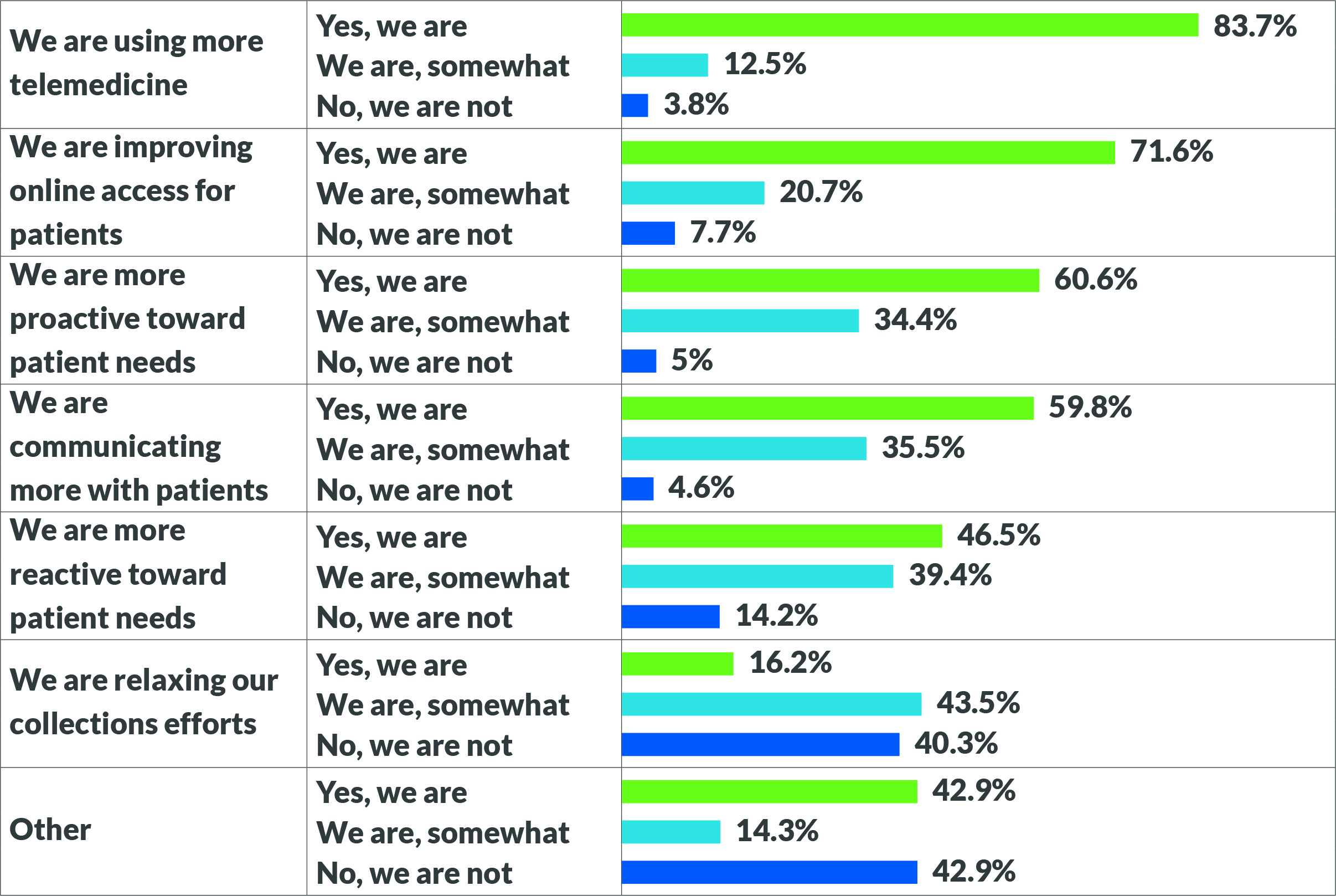
Patients are facing financial challenges unlike ever before. As of December 2020, the U.S. unemployment rate was 6.7%, compared with 4.5% in March.2 Respondents to the HFMA survey said they are employing various strategies to ease the burden among their patients, as seen in the exhibit on page 43. The use of telemedicine and online access for patients were clear areas of focus for 83.7% and 71.6% of respondents, respectively, particularly in larger organizations.
On the financial side, although many responding organizations said they are changing their habits around patient billing, many are not. Only 16.2% of respondents said they’re relaxing collections efforts, while 40.3% reported that they are not. Furthermore, organizations that are relaxing efforts report the highest levels of write-offs, due to aging of receivables and perceived importance of patient balance responsibility. To counter this trend, survey respondents said they are focusing their primary efforts on collecting from insurers, rather than patients.
At Texas Health Resources, a 24-hospital system in the Dallas-Fort Worth area, the mantra is to provide patients with “hope and options,” said Jeff Mincher, vice president of revenue cycle operations.
“We try our best every day to meet patients where they are on the financial journey and help them understand their financial obligation for the care they need,” he said.
Mincher’s health system chose not to suspend patient billing as some health systems did at the beginning of the pandemic. Instead, they took — and continue to take — a targeted approach to ensure that patients with the ability and propensity to pay will do so, while offering payment options to those who need them.
“Patients want to be heard and know that we take their concerns seriously. We screen for financial assistance needs and provide flexible payment arrangements,” he said. “We find if we can get a patient to agree to a payment arrangement and set it up on auto-pay, they largely meet that obligation.”
For Kimberly Scaccia, vice president of revenue management at Mercyhealth in Wisconsin and Illinois, adjusting to the pandemic was a trial by fire, as her first day on the job was March 23, 2020. Previously, Mercyhealth had large self-pay receivables, a small staff collecting them and no partner to help. Furthermore, staff did not regularly have conversations with patients about their financial responsibility on the front end; 70% of the health system’s self-pay receivables were after insurance, which meant there was ample opportunity to break down for patients exactly what insurance would cover and how much would be owed out of pocket.
“During a pandemic, it’s hard to ask people for money, but you have to help them understand their financial responsibility,” she said.
Right away, the health system began discussing ways to have conversations with patients, including training staff to ask for payment and offering payment tools and strategies such as financial counseling, charity care and no-
interest payment plans that can help ease patients’ financial burden. This tracks with the survey, in which 95.3% of respondents said they are fully or somewhat communicating more with patients and 95% said they are fully or somewhat more proactive toward patient needs. Only 5.12% said they are reducing or eliminating payment collection from patients at the time of service.
In an environment where patients are delaying care, provider organizations should use every tool they have to encourage patients to get the care they need, said Shannon Burke, general manager, health systems, CareCredit.3
“Provider organizations want to spend less time on billing and more time caring for patients, but that is a challenging balance to strike,” Burke said. “Flexible payment arrangements can ensure patients are getting the care they need with minimal strain on accounts receivable or the revenue cycle.”
Priorities shift, but the larger goal remains
Consumerism has been an important strategy in the industry for some time, but how organizations approach it has always varied. The first phase of the joint research conducted by HFMA and CareCredit found that the very definition of “healthcare consumerism” varied depending on the organization’s trends and priorities.4 Much has changed since that phase, which was conducted in September 2019. For example, telemedicine was not a topic of discussion in the early research and was largely not considered an industry priority, but it quickly became essential at the onset of the pandemic.
The second phase of research, conducted in February and March of 2020, indicated that although organizations reported more success when their consumerism initiatives were proactive rather than reactive, 43% of respondents reported an approach that balanced both proactive and reactive initiatives.5 The third phase of research indicated that although healthcare organizations did indeed ramp up their strategies around telemedicine and online access in response to the pandemic, they stopped short of eliminating their previous systems. Only 11.06% of respondents said they are “very much so” reducing or eliminating acceptance of physical tender such as cash or check, with 23.04% doing so “somewhat,” although many have taken steps toward a contactless patient financial experience (41.47% “very much so” and 50.69% “somewhat”).
“The pandemic created a common focus and rallying cry for clinical, operational and financial teams,” said Todd Nelson, HFMA’s director of partner relationships and chief partnership executive. “Organizations took on a collaborative approach to everything from caring for the communities they serve, to protecting their caregivers, building resiliency in supply chain and financial sustainability and recovery. It placed the highest priority on all initiatives that influenced pandemic-related services.”
The remote workforce of the future
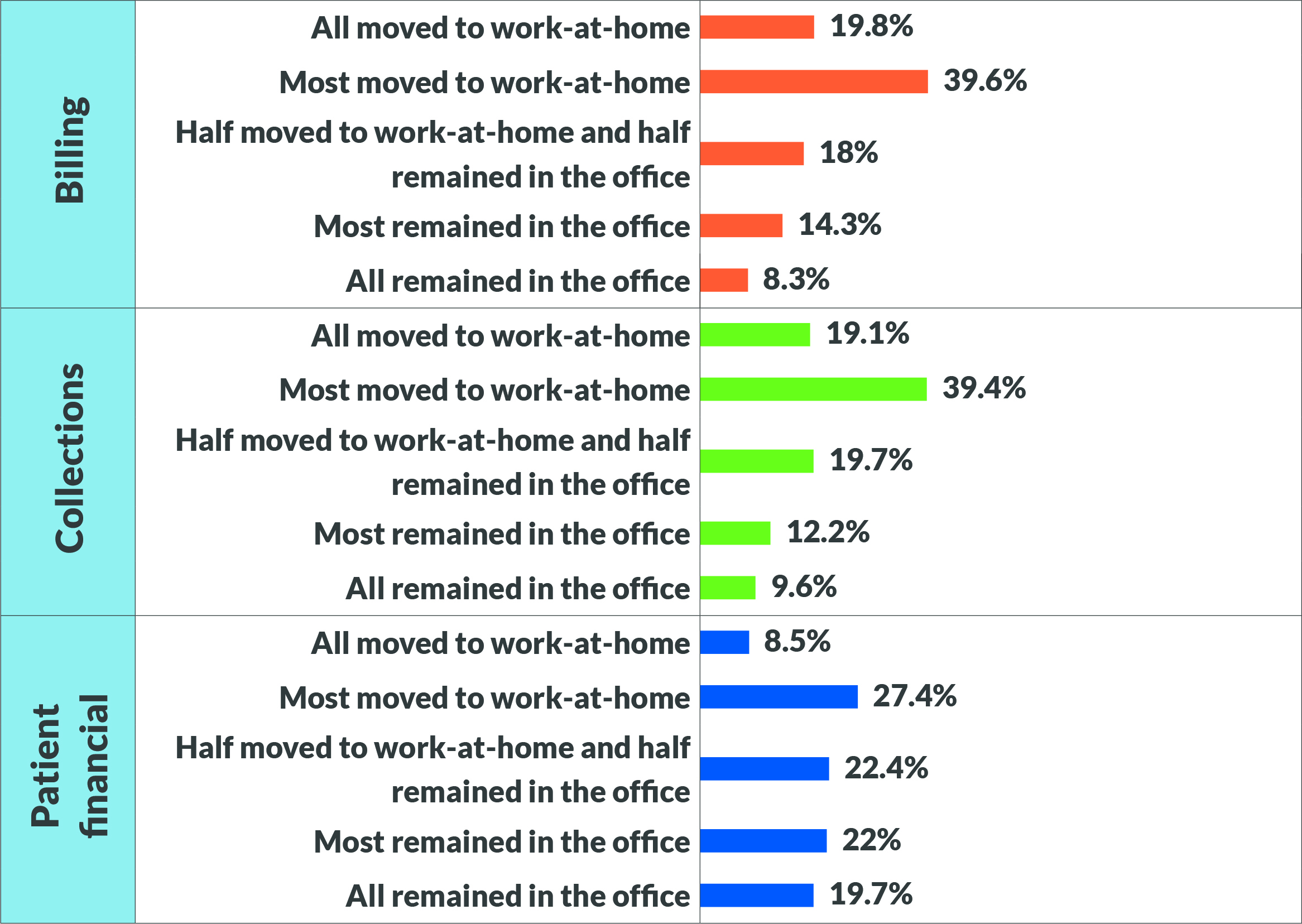
Another key element that has changed since early 2020 is where staff perform their duties. As of October 2020, 33% of the workforce was working remotely 100% of the time, according to a Gallup poll.6 Respondents to the HFMA survey indicated across services that most in-house employees moved to remote work, as seen in the page 45 exhibit. Very few respondents indicated that they’d kept all employees on-site. Organizations that put a heavy focus on digital services and strategies such as contactless transactions, telemedicine and improved online access report the most work-at-home employees.
Many healthcare organizations already had employees working from home before the pandemic, making the transition easier, but these organizations revisited their approach to ensure continued high performance. Texas Health Resources serves as one example.
“We evaluated positions that are required to be on-site due to the work they perform and created socially distant workspaces, staggered days in the office and hours worked,” Mincher said. The health system also has worked to ensure employees are connected and engaged while working from home both from a technology standpoint and a cultural one.
“We are discovering that our employees do miss the water cooler talk,” Mincher said. “We have meetings where we encourage the use of camera and the chat features, and I find starting a meeting off with a fun icebreaker where people can update the group in the chat can be an easy break in the day. We also encourage meetings to be less than 60 minutes.”
Staying nimble was key for healthcare organizations as they moved employees to work from home and, eventually, back to the office. At Luminis Health, a regional health system headquartered in Annapolis, Maryland, around 85 of the 90 people on the revenue cycle staff on two campuses chose to begin working remotely, according to executive director Zubair Ansari. Some prefer working in the office, and one person did not have internet service at home, so the system worked to provide that employee with the funds to obtain it. Luminis Health also conducted a staff survey and formed a safety committee that developed a strategy to help employees feel safe when on-site. That plan included seating diagrams to allow for social distancing as well as signage and hand sanitizing stations.
Mercyhealth’s Scaccia said she envisions a hybrid model going forward, even after the pandemic has ended. From a practical standpoint, such a model means less space and expense, and the process of moving through the pandemic with a remote workforce has been an exercise in management, she said.
“Some of the areas where I had the biggest concern to send people home have just blossomed,” she said. “I think we’re going to come out of this a whole lot stronger than we were in the beginning.”






