How investment in AI for healthcare organizations has changed due to the pandemic
For many health systems, COVID-19 has accelerated investment in AI or emphasized its value across the enterprise.
More than half of healthcare leaders expect artificial intelligence (AI) to drive innovation in their organization over the next year, and four out of five CFOs believe immediate digital transformation will be critical to their organizations’ survival following the pandemic.
It’s a sign that more and more healthcare leaders are turning to AI — including robotic process automation and machine learning — to drive enterprisewide impact. One recent survey shows 57% of healthcare CFOs plan to accelerate the adoption of automation and new ways of working due to the pandemic, compared with 44% of CFOs across industries.
“Before COVID-19, AI was seen more as a novelty with future potential,” says Scott Connor, vice president, financial planning and analysis, Piedmont Healthcare, which is just beginning its journey with AI. “It was more challenging to find defined uses for AI. During COVID-19, the focus has become, ‘How do you begin to predict the future in a very volatile world?’ The need to forecast what the next quarter or the next year is going to look like, both financially and non-financially, has changed how we view AI, especially tools that can help you better prepare for this uncertainty.”
“I certainly think COVID has raised awareness of the importance of AI — in particular, machine learning,” says Greg Nelson, associate vice president for analytics, Intermountain Healthcare, Salt Lake City, Utah. “It has coalesced much of our work around AI. We’re in the process of developing an AI Center of Excellence at Intermountain Healthcare to focus these efforts as an enterprisewide enabler for innovation.”
Most healthcare organizations are ramping up investments in automation in response to COVID-19, including the use of robotic process automation for highly manual, administrative functions. Others are taking a fresh look at AI’s enterprise value proposition.
Even before the pandemic, AI was quickly emerging as a valuable application for healthcare in four areas: administrative, clinical, financial and operational. A fall 2019 survey of healthcare leaders showed that 51% of healthcare providers had already implemented an AI strategy, compared with 22% in 2018. On top of that, half of healthcare industry leaders ranked “automating business processes” as their top priority.
Now, as hospitals seek ways to overcome significant declines in revenue during the pandemic:
- 84% of hospitals have audited their state of digital transformation. Top areas of focus: software solutions that capture revenue and anticipate industry shifts through innovative analytics and forecasting tools.
- 56% of healthcare CFOs believe technology investment will make their company better in the long run, a June 2020 survey shows.
How are hospitals evaluating AI investment decisions across the enterprise and what steps are they taking to achieve value quickly? Leaders from four health systems at varying stages of AI deployment share their insights.
Moving toward a comprehensive AI approach
At OSF HealthCare, staff have fielded more than 137,000 COVID-related digital encounters using tools that were launched days after the coronavirus outbreak emerged in the United States. Key to the health system’s agility: a systemwide strategy for digital innovation, including AI.
There’s Clare, an AI-fueled chatbot that screens individuals for the virus via the Peoria, Ill., system’s website and connects those with symptoms to a 24-hour COVID-19 nurse hotline. The health system initiated the AI chatbot in December 2019, but revamped it to become a COVID symptom tracker in just three days when the pandemic began. Its nurse hotline, “OSF Knows,” went live in just two days this past March, leveraging investments in advanced call center technology designed before the pandemic.
Meanwhile, an all-digital Pandemic Health Worker Program, launched in April 2020, put remote monitoring tools in the hands of those who exhibit COVID-19 symptoms or are at high risk for contracting the virus. Created in partnership with the state of Illinois, the program uses AI and telehealth to digitally support those who need care. It’s an approach that helps prevent unnecessary emergency department (ED) visits throughout the 14-hospital system, while ensuring that infected and vulnerable patients receive personalized care.
The response to these tools has been outstanding. From March through Sept. 6, 2020, more than 123,000 app-driven interactions have taken place through the chatbot, with over 42,500 chats related to the COVID-19 outbreak. Nearly 79,000 patients have received help through the COVID nurse hotline and another 2,750 patients have been served through the Pandemic Health Worker Program.
Three years ago, OSF Healthcare formed a multidisciplinary team to create a digital strategy road map for the system, with AI adoption being an area of focus. Among the projects that the health system sought to implement quickly, an AI chatbot rose to the top due to its potential for high impact.
“Had we not already had the foundation, the vendor relationships, the team and the structure in place to digitally respond to the pandemic, we would have never been able to go live with a COVID AI symptom tracker chatbot within a 72-hour window,” says Jennifer Junis, RN, MSN, senior vice president, OSF HealthCare Saint Gabriel Digital Health. “Had we not invested in our contact center technology, we wouldn’t have been able to come up with a COVID nurse hotline. Without some of the digital tools that we had invested in before the pandemic, we wouldn’t be able to respond digitally on such a large scale — and that would have had a negative impact on our facilities as well as our communities.”
The AI readiness of large health systems varies by organization. For Banner Health, which has explored AI for clinical and operational initiatives on a case-by-case basis, COVID-19 presented opportunities to further leverage existing AI solutions that were implemented prior to the pandemic, such as an online symptom checker, an ED chatbot that keeps patients informed throughout their visit and intelligent automation in revenue cycle. For example, use of robotic process automation (RPA) to ensure COVID-19 claims were not balance billed saved 1,500 man hours while ensuring compliance with federal and state regulations, including the CARES Act. Now, the health system is establishing an internal center of excellence for RPA, with two initiatives that are set to save more than 20,000 man hours through the end of 2020.
“I don’t think the pandemic has caused us to say, ‘Wow, we should use AI more deeply because of what we’ve learned during the pandemic,’” says Anthony Frank, senior vice president, finance, Banner Health. “However, we do have the ability to make decisions faster because of the pandemic, including around AI. If AI is the right solution to solve a problem, we might be more inclined to pull the trigger.”
Healthcare leaders identify top barriers to digital strategy
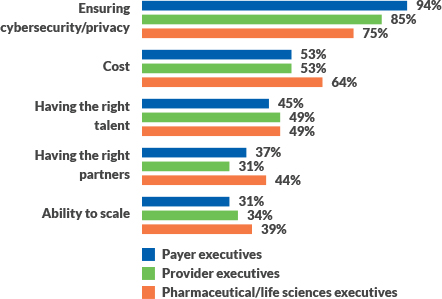
Source: PwC Health Research Institute executive survey, September 2019
For Piedmont, where the initial focus of AI investment has been on machine learning, leaders are now looking more broadly at AI opportunities. “The idea of being able to predict future events and get out in front of emerging trends has become a high priority for our organization. The type of tool that we use to enable these insights is probably less of a defined priority,” said Mark Jackson, director of business intelligence for Piedmont. “I also believe there will be organic growth that comes out of having an AI platform that we can’t even anticipate right now. That’s one reason why we’d like to have an AI platform in place that can serve the vast majority of use cases, rather than trying to implement every vendor’s version of machine learning or AI functionality.”
At Intermountain Health, AI adoption began in the clinical domain prior to the pandemic, with tools that help predict and prevent sepsis, detect pneumonia in chest X-rays in 10 seconds, and develop customized interventions for chronic kidney disease patients. Now, the health system is developing an “AI playbook” to help stakeholders make responsible, ethical decisions around AI investment.
“We view AI as an opportunity to augment intelligence, not replace it,” Nelson says. “We want to make sure that our caregivers know: We’re not going to adopt ‘black box’ AI models that don’t explain to clinicians what a machine or tool is doing. We’re building AI literacy among our team members and exploring what is possible, with a focus on, ‘What are the key problems we are trying to solve and why are they hard to address? What are the operational consequences if we don’t solve these problems? And, more important, what could go wrong if our approach to solving this problem isn’t the right approach?’”
In evaluating AI opportunities, leaders for OSF HealthCare look for “radical efficiencies” — not just whether AI investment will result in cost savings or revenue generation, but also how human capital affected by AI solutions can be redeployed to provide value in other areas. “We’re expanding on some of our lessons learned through the pandemic,” Junis says. “We’re continuing to stand and expand virtual visits across our system, and we’re planning to convert our pandemic health workers into digital health workers. Remote RPA is on our strategic plan for implementation over the next 12 to 18 months.”
Meanwhile, Intermountain relies on a rubric developed prior to the pandemic to help team members assess AI opportunities, considering clinical, operational, and financial benefits and the way in which potential investments align with the organization’s strategies. “In the past couple of weeks, we’ve identified what we consider to be bold AI opportunities, with about 80 projects under consideration, from supply chain to price optimization to care delivery tools,” Nelson said during an August 2020 interview. “We’re working to build an ecosystem of digital innovation that will enable people to operate at the top of their licensure.”
A snapshot of AI implementation before COVID-19
- 51% of providers report they have implemented an AI strategy, compared to 22% in 2018.
- 88% of health plan respondents report they have implemented an AI strategy, compared to 50% in 2018.
- 70% of leaders at life sciences organizations report they have implemented an Ai strategy, compared to 34% in 2018.
- 58% of healthcare employers report they have implemented an AI strategy, compared to 38% in 2018.
Source: Optum Annual Survey on AI in Health Care, 2019
Models for AI implementation
Determining the path to AI implementation is one of the toughest challenges a healthcare organization may face in its journey. So is overcoming common barriers to adoption, including cost, access to talent and having the right partners to support AI innovation.
A recent survey of healthcare executives shows that 43% of healthcare leaders favor a partner that can deliver an all-in-one offering to implement AI (see the exhibit below). It’s viewed as an approach that lessens the implementation burden on employees — a serious concern, given the shortage of data analytics talent in the industry — and resources.
Implementation approaches among organizations interviewed vary. At Banner Health, “We probably have more partners than you might expect,” Frank says. “When we’re seeking to solve a problem with an AI solution, we really want the best of the best rather than a single partner that can do everything, but with varying degrees of success.”
Piedmont Healthcare seeks to develop its business intelligence team members to oversee the introduction of AI in specific functional areas. These team members have dedicated project time with functional leaders within Piedmont Healthcare. “We use the Agile development methodology, planning our work in two-week increments,” Jackson says. “Once we have someone in-house who is well-versed in the tool and we have a couple of use cases under our belt, we promote the use of the tool within the project teams they belong to and generate new use cases.”
OSF HealthCare relies on its innovation team as well as an external partner to identify the top AI solutions available to address a particular challenge. Once candidates are evaluated and a partner is selected, the health system then leans on the expertise of its performance improvement team as well as its multidisciplinary digital transformation team to guide AI implementation in partnership with health system vendors.
“A tight project management team is really key,” Junis says. “When we’re selecting a partner, we use a matrix to narrow our selection to the top two or three candidates and bring that list to our transformational executive, who makes a recommendation. Because traditional IT selection processes in health systems can be rather slow, this helps speed up the process. If we’re choosing a start-up company, a lot of times, we’ll start with some pilot work.”
What do organizations look for in an AI partner? Healthcare expertise is key, leaders agree. So is the ability to quickly harness insight from data.
“Speed to insight has always been a big factor for us in choosing an AI partner,” says Jackson of Piedmont. “That’s what has driven our data warehouse vendor and our vendor for business intelligence visualization tools. We also consider: ‘Is this a tool that lets us iterate on our designs rapidly, or will it potentially slow down the way in which we process work?’ The faster we can fail, the more successful we’ll be because we’ll be able to figure out what doesn’t work to get to what does work.”
Confidence, repeatability, transparency and the ability to explain how the results were derived also are critical, says Nelson of Intermountain.
Amil Kekic, senior director, innovation ventures for Banner Health, recommends selecting a vendor that is well-established in the healthcare industry. “We look at past experiences with other healthcare clients,” he says. “Another key question we consider is, ‘What data elements are needed for this solution, and can we provide those?’ The intended results from the AI solution may not be fully realized if all the data elements can’t be provided.”
Healthcare leaders identify preferred models for AI implementation
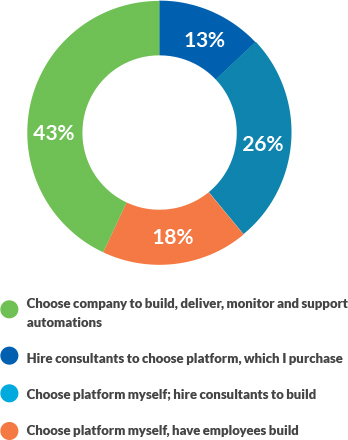
Source: Sage Growth Partners Research Study: The Value of AI, 2020
Assessing AI’s value
Determining the value of AI investment is a growing competency for healthcare organizations. “We continue to work on quantifying the value of these investments,” says Junis of OSF HealthCare. “We have a dedicated finance person for digital strategy so we can better understand the return on investment from these initiatives and bring those value propositions forward.”
Investment for each of these organizations starts with a business case for improvement. Nationally, strategic goals for AI range from improving quality of care — the top priority for 30% of healthcare executives in one recent survey. Nearly three-in-four healthcare executives ranked improving efficiency and reducing costs among their top three priorities.
In evaluating value, it’s important to consider the way in which a tool will impact staff. “Some machine-learning applications can actually create more work if not correctly deployed,” Connor says.
Finding strong use cases for AI also can be a challenge. “You have to parse through the noise of what people think it is and what it can actually do,” Connor says. “The more use cases you have, the more your team will understand what AI can do, and the better prepared your organization will be to leverage these solutions.”
Ultimately, achieving value in AI also requires that leaders have a plan for operationalizing innovation across the enterprise.
“One of the challenges in implementing AI across industries is that we rarely consider the people who will be affected by AI in the design of a solution or in implementing it — and that’s a mistake,” Nelson says. “If a solution is going to trigger an alert to a nurse, for example, nurses need to be part of the first conversation we have about the tool. If we don’t take their perspective into account, we’re going to miss a value opportunity.”
“I’m a pragmatic AI champion,” Nelson says. “Innovation is built into our DNA, so we’ll continue to reach for those really crazy ideas and see whether that spaghetti noodle hits the wall and sticks, but the majority of our time needs to be on practical, pragmatic AI opportunities that leaders across the organization agree are problems that we need to solve. There also must be a readiness to solve them, and it should be feasible to solve these challenges in a fairly short amount of time. So while we take moonshots, the bulk of our activity should be focused on, ‘How do we make a difference today by implementing AI?’”
Making the right moves for a post-COVID future
As hospitals and health systems explore new ways to plan and strategize for the future during COVID-19, many are facing increased urgency to adopt AI to improve their cost structure, workforce resiliency, productivity and revenue generation. No longer will automation of administrative and financial tasks be enough. Following the pandemic, leaders may find that faster adoption of AI and automation across the enterprise will help sustain operations long term.
As these health systems’ experiences show, developing an enterprisewide AI strategy — one with careful consideration around selecting the right model, choosing an experienced partner for implementation and maintenance and assessing the value of AI investment — is key to achieving sustainable value in a transformative environment.
About Olive
Olive thinks humans should do human things, and AI should do AI things. In fact, manual, robotic work is one of the leading reasons that one out of every three dollars spent in healthcare is on administrative costs. Olive’s AI workforce was built specifically for healthcare, automating high-volume tasks to make healthcare more efficient, more affordable and more human with AI. Olive’s all about improving your operations today, so you can reinvent the future of healthcare tomorrow. Learn how Olive is changing the future of healthcare with healthcare’s AI workforce at www.oliveai.com.
This published piece is provided solely for informational purposes. HFMA does not endorse the published material or warrant or guarantee its accuracy. The statements and opinions by participants are those of the participants and not those of HFMA. References to commercial manufacturers, vendors, products, or services that may appear do not constitute endorsements by HFMA.






